
Emerging challenges in the health
systems of Kerala, India:
qualitative analysis of
literature reviews
Manesh Muraleedharan
SCRI, Symbiosis International University, Pune, India, and
Alaka Omprakash Chandak
Symbiosis Centre for Healthcare, Symbiosis Institute of Health Sciences,
Symbiosis International University, Pune, India
Abstract
Purpose – The substantial increase in non-communicable diseases (NCDs) is considered a major threat to
developing countries. According to various international organizations and researchers, Kerala is reputed to
have the best health system in India. However, many economists and health-care experts have discussed the
risks embedded in the asymmetrical developmental pattern of the state, considering its high health-care and
human development index and low economic growth. This study, a scoping review, aims to explore four major
health economic issues related to the Kerala health system.
Design/methodology/approach – A systematic review of the literature was performed using PRISMA to
facilitate selection, sampling and analysis. Qualitative data were collected for thematic content analysis.
Findings – Chronic diseases in a significant proportion of the population, low compliance with emergency
medical systems, high health-care costs and poor health insurance coverage were observed in the Kerala
community.
Research limitations/implications – The present study was undertaken to determine the scope for future
research on Kerala’s health system. Based on the study findings, a structured health economic survey is being
conducted and is scheduled to be completed by 2021. In addition, the scope for future research on Kerala’s
health system includes: (1) research on pathways to address root causes of NCDs in the state, (2) determine
socio-economic and health system factors that shape health-seeking behavior of the Kerala community,
(3) evaluation of regional differences in health system performance within the state, (4) causes of high out-of-
pocket expenditure within the state.
Originality/value – Given the internationally recognized standard of Kerala’s vital statistics and health
system, this review paper highlights some of the challenges encountered to elicit future research that
contributes to the continuous development of health systems in Kerala.
Keywords Kerala health system, Kerala health insurance, Kerala public health, Heart disease,
Health economics, Emergency healthcare
Paper type Review
JHR
36,2
242
© Manesh Muraleedharan and Alaka Omprakash Chandak. Published in Journal of Health Research.
Published by Emerald Publishing Limited. This article is published under the Creative Commons
Attribution (CC BY 4.0) licence. Anyone may reproduce, distribute, translate and create derivative works
of this article (for both commercial and non-commercial purposes), subject to full attribution to the
original publication and authors. The full terms of this licence may be seen at http://creativecommons.
org/licences/by/4.0/legalcode
Sincere thanks to the Symbiosis Center for Research and Innovation for their continuous support.
Heartfelt thanks to Mr. Deepanshu Lekhi for his guidance and support. Sincere thanks to Ms. Neha Saini
for her expert editing.
Received 6 April 2020
Revised 8 May 2020
27 May 2020
Accepted 13 June 2020
Journal of Health Research
Vol. 36 No. 2, 2022
pp. 242-254
Emerald Publishing Limited
e-ISSN: 2586-940X
p-ISSN: 0857-4421
DOI 10.1108/JHR-04-2020-0091
The current issue and full text archive of this journal is available on Emerald Insight at:
https://www.emerald.com/insight/2586-940X.htm
Introduction
In India, health care follows a decentralized approach in which implementing and executing
health facilities is the responsibility of each state, with considerable overlook from the central
government. Health-care financing and policymaking are the responsibilities of the central
government, whereas implementing the policy is the responsibility of the state government
[1–3]. The national health policy established in 1983 was the first initiative toward
implementing a structured health-care system and introducing various national health
programs in the country. Records indicate that because of the decentralization and health
care being a state’s responsibility, a considerable disparity can be observed in the health-care
delivery standards among different states; some states are still struggling, whereas others
display enormous improvements [4].
Kerala has a gross domestic product (GDP) per capita of US$3,200 and is classified as a
lower-middle-income state. Kerala is well known for maintaining one of the best health-care
systems in the country for decades [5]. The “Kerala model of development” became a widely
used term after the survey conducted by the Center for Developmental Studies on poverty
and unemployment in 1975. According to experts, irrespective of its low per capita income,
Kerala’s health system has excelled and continuously garnered national and international
attention. As stated by various health surveys, including the central government’s analysis
reports, Kerala leads many other states in having high health-care standards and life
expectancy rates, low maternal mortality rate and the lowest infant mortality rate in the
country (Table 1). Hig h literacy r ates and wom en empowerment have con tributed
significantly toward this achievement. However, numerous past experiences and studies
indicate that Kerala is in the era of an emerging puzzle because of its high morbidity rate with
low mortality rate, besides having a significant increase in non-communicable diseases
(NCDs) [3, 6–11].
This unique community has taken enormous steps to reduce mortality by implementing
robust primary care facilities, resulting in a significant increase in chronic degenerative
diseases among the middle-aged and adult population [12, 13]. A significant proportion of
adults in Kerala are living with chronic morbidities, especially illnesses such as hypertension,
diabetes and atherosclerosis, which are known to develop chronic complications such as
heart failure and kidney diseases [9, 11, 14]. Moreover, previous studies state that the
approach of the Kerala population toward seeking timely emergency medical attention was
questionable [8, 9, 15]. Golden hour treatment is the most effective option during the acute
phase of a stroke or coronary event and is possible only during the early hours of these
illnesses. Golden hour treatment protocols are advised by medical authorities such as the
American Heart Association and American Stroke Association. The golden hour is 4 h 30 min
for an acute stroke and 6 h for an acute coronary event [16]. Delayed treatment or consultation
Measure National Kerala
Maternal mortality rate 130/100,000 46/100,000
Infant mortality rate 32/100,000 10/100,000
Literacy rate (%) 70.04 93.91
Life expectancy (years) 68.56 74.9
Per capita GDP (US$) 2,009.979 3,200
CVD death rate 272/100,000 Male: 382; Female: 184
Diabetes prevalence (%) 11–12 18–20
Hypertension prevalence (%) 28–30 30–38
Source(s): NITI Aayog, National Sample Survey, Kerala 2018 [1], Kerala budget analysis 2020; World Bank
national accounts data 2018–2019
Table 1.
Comparison of various
socio-economic and
health-care indicators
of Kerala state
and India
Health systems
of Kerala
243

for acute coronary syndrome or a stroke may lead to mortality or a high incidence of disability
[8, 9, 15]. Delayed treatment can also lead to ineligibility to access the golden hour treatment,
which may result in severe heart failure or stroke, often requiring long-term care, medication
and rehabilitation [17, 18]. High morbidity status with low coverage of health insurance or
other reimbursement facilities can prove lethal to the long-term financial sustainability of a
community. Therefore, it is essential to analyze previous studies and reports to explore the
loopholes in Kerala’s health system.
Methodology
This study adopted a systematic review design with the purpose of exploring and describing
the literature related to the health systems of Kerala and to identify emerging challenges and
prospective research areas.
Data sources
Journal publications and gray literature such as relevant websites of the Government of India
and state government reports available in the public domain.
Searching strategy
Data search and identification were done mainly using PubMed, Scopus and Google Scholar
to retrieve journal publications. A Boolean search was employed using keywords and
operators. The literature search was conducted between October and November 2019. The
process of literature identification and refinement are summarized in Figure 1.
Data selection (inclusion and exclusion)
Studies and reports between 2010 and 2019 related to health systems of Indian states were
included. Within these studies and reports, the following data were selected: socio-economic
indicators, health system indicators, emergency health management system data and health
financing data. Abstracts only and conference proceedings were excluded.
Total citaons –10Total citaons –608
287 without duplicates
118 arcles idenfied
(109 journals + 9 official
documents)
77 journals selected for
review
Manual screening
of abstract/ tle
Exclusion (31)
• Not related to Kerala
health system
• Conference
proceedings/ no
clear methodology/
no full informaon
Figure 1.
PRISMA flow diagram
JHR
36,2
244

Quality check process
A reviewer and an external expert independently screened the articles using a standard
quality assessment scale. Disparities in the selection of the documents were resolved by
manual agreement.
Data management
Mendeley was used for the management of references. The articles were initially stored,
categorized and refined in Mendeley based on the date of publication, topic and authenticity.
The selected articles were analyzed after converting them to Microsoft Word format. A
coding analysis toolkit (CAT) was used for coding the document.
Data analysis
The World Health Organization reports on health system performance were reviewed and
used to develop preliminary codes for data analysis. Quantitative data served a descriptive
statistical analysis using frequencies and proportions, whereas qualitative data served a
thematic content analysis. Dixon–Wood’s critical interpretive synthesis was employed for
qualitative data.
A reviewer and an external expert individually coded the articles based on the preliminary
codes developed. Operational definitions of codes were adjusted to iron out disparities.
The themes developed were as follows:
(1) Theme 1: Increasing burden of NCDs and chronic morbidity
(2) Theme 2: Low utilization of emergency health-care facilities
(3) Theme 3: Inequalities in the performance of the health system
(4) Theme 4: High out-of-pocket expenditure
Ethical issue: Review paper do not need approval code
Results
Theme 1: increasing burden of non-communicable diseases and chronic morbidity
Various records and experts have discussed the issue of high morbidity and low mortality in
Kerala state and the long-term effects and complications associated with this [5, 6, 11, 19, 20]
The prevention of communicable diseases and NCDs was one of the major objectives of the
12th five-year plan developed by Kerala state, 2012–2017. The case fatality rate of acute heart
failure, which was up to 25% in the 1980s, is as low as 4% at the moment [15, 21, 22]; the same
trend was observed for several similar NCDs [23]. This prevented a significant proportion of
mortality among the middle and old-age population, which resulted in a higher number of
people suffering from chronic illnesses [24, 25]. Studies have shown that 74% of the morbid
population suffers from chronic illnesses [7, 9–11]. The substantial rise of chronic illnesses
such as hypertension and diabetes in the middle-aged population was reported as a
significant concern, and many medical practitioners and researchers considered the state as
the diabetes capital of India [9–11, 26, 27].
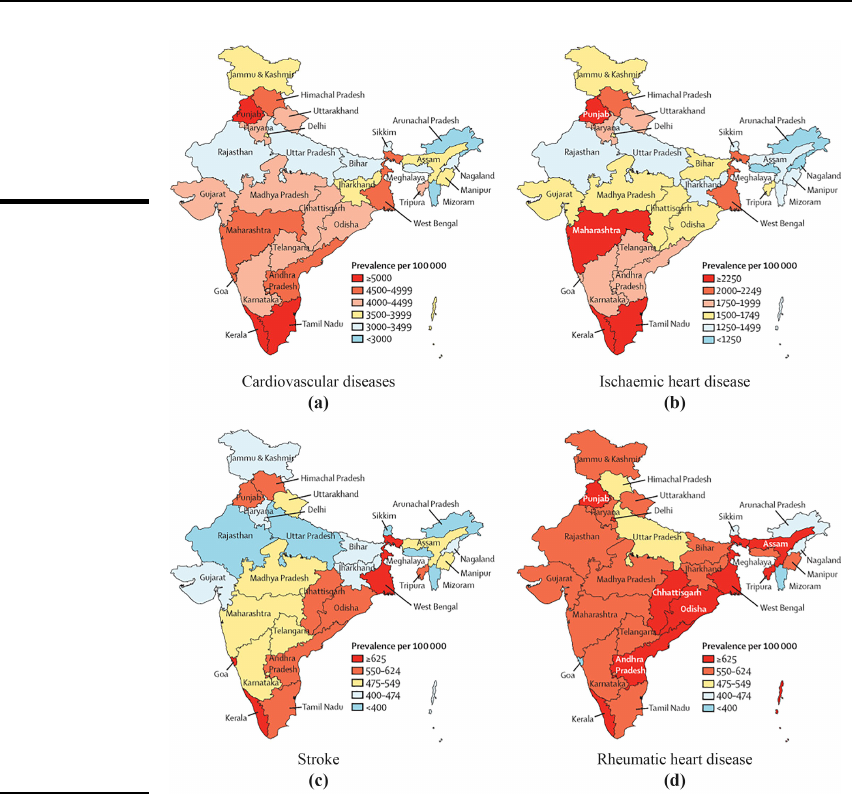
The prevalence of diabetes among people in Kerala was projected to be around 14%, while
it was around 40% for hypertension [11]. A recent study [28] mapped the prevalence of major
NCDs of various Indian states (Figure 2). The map shows a high prevalence of cardiovascular
diseases, ischemic heart diseases, stroke and rheumatic heart diseases in Kerala compared
with other states in the country. However, it is important to consider that a high literacy rate
and awareness can be directly related to a higher reporting of diseases [29]. However, none of
the literature or official reports showed any decline in the NCD statistics for 25 years.
Health systems
of Kerala
245
An increase in chronic morbidity is a real burden to any community. Hence, it is important to
study Kerala’s population characteristics in-depth and to intervene early [3, 20].
Theme 2: low utilization of emergency health-care facilities
A recent survey by the directorate of economics and statistics of Kerala concluded that only
around 11% of the total registered deaths were medically certified, indicating that most of the
deaths occurred outside medical environments. The survey also indicated that more than
30% of the deaths found among the young and middle-aged population were aged below 64
years [28]. However, the study did not reveal the causes for deaths that occurred outside the
medical environment. Further study is needed, especially because of the higher mortality
found among young and middle-aged people. Another noticeable fact is the low utilization of
the golden hour treatment for any vascular illness, especially for stroke and cardiovascular
Figure 2.
Crude prevalence of
cardiovascular
diseases and major
component causes in
the states of India
(2016). The changing
patterns of
cardiovascular
diseases and their risk
factors in the states of
India and the global
burden of disease [30]
JHR
36,2
246

diseases [5, 8, 9, 22, 31 ]. Studies related to emergency cardiac or stroke treatment in the Kerala
population are scarce [8, 9, 32]. One of the studies concluded that the pre-hospital delay in
acute stroke patients is significantly high compared to other communities. A similar study
done on an acute cardiac event group exhibited concurrent findings of low utilization of pre-
hospital emergency services in Refs. [8, 33].
The higher pre-hospital delay was associated with multiple stops the victims took before
reaching the specialty center [8]. However, the reasons behind this observation were not
revealed by the previous studies. According to some studies, awareness of the population
regarding recognizing symptoms of a cardiac or cerebrovascular illness was contentious
[5, 8, 32]. Patients with more disturbing symptoms such as limb weakness or chest pain
arrived at hospital facilities earlier compared with subtle or vague symptoms [5, 8, 32, 34].
Some studies reported the issue of under-reporting of less severe or benign illnesses,
especially among the poor [14, 35]. Higher education and better socio-economic status were
factors for recognizing symptoms of vascular illnesses [34, 36]. Most studies from India and
other countries concluded that people with higher educational qualifications tended to visit
the hospital early in the event of an acute cardiac attack or stroke [ 37– 40]. Regarding the pre-
hospital emergency services in the state, some were termed as “not satisfactory” by some
studies [9, 21, 28, 41, 42]. Additionally, organization-level management nicks play a role in the
failure of emergency management in case of vascular ailments [9, 32]. Kerala’s health system
has achieved tremendous success in its primary care strategies; however, their emergency
care efficiency is contentious. Only a few studies and limited data are available in this aspect,
and most of them are limited to a particular disease or region.
Theme 3: inequalities in the performance of the health system
Kerala is a relatively small state compared with other territories in India [43, 44]. The living
standards and socio-economic inequalities were found to be higher in the urban areas
compared to rural areas [14, 20, 45, 46]. Sometimes, this variation was observed in the same
rural or urban territory, and regions occupied by lower financial class people seemed to utilize
medical facilities at a lower rate [27]. Another interesting observation in the literature was the
disparity between the north and south regions of the state, which was more evident in the
past and is gradually narrowing down [47]. The southern part of the state is considered better
in many areas of development, including living status and health-care consumption [20, 47].
Some studies revealed that certain regions lagged in the process of health-care improvement.
For example, the Malabar region was far behind in the mortality reduction programs in the
early stage [12], whereas higher morbidity was observed in the developed regions [43, 48].
This disproportionality is vividly depicted in the comparison of health-care infrastructure
distribution in various districts [47]. A large geographical area in northern Kerala is still
dependent on a few tertiary care public medical centers for specialty treatment and has no
active tertiary care institutions in two major districts, Kasargod and Wayanad. On the
contrary, a small geographical area in southern Kerala possesses a relatively large number of
medical institutions. Trivandrum is the southernmost district and is flooded with several
national and state-level specialty centers. Table 2 illustrates the disparities in the distribution
of health-care facilities in the state. The northernmost districts of Kasargod and Wayanad
have no low density of specialty medical facilities, and the bed ratio was low at 6.3 and 8.69,
respectively. On the other hand, Trivandrum had a bed ratio of 18.48, with multiple specialty
centers. Apart from this, all major private health-care players were concentrated in cities with
a high population density. Quality of care and ease of access made private health facilities a
primary choice in Kerala [49]. Public health-care facilities in Kerala are still struggling with
financial and infrastructure crises. Although this was a nationwide observation, Kerala has
also not made any differences [50–
55]. Some studies have evidenced the caste or community-
based stratification with poor health security coverage and higher health risks over certain
Health systems
of Kerala
247

marginalized groups in Kerala [14, 45, 56]. In addition, some studies reported gender-based
inequalities, which were more evident in marginalized social groups [43, 57].
Theme 4: high out-of-pocket expenditure
The health system of Kerala has proved to be the best in India and is considered a model
health system to be followed to achieve a high human development index for a struggling
economy. However, the literature reveals that health financing in the state has been criticized
because of the high rate of catastrophic expenditure on health and poor insurance coverage.
Some surveys reported the financial status as a reason for restricting people from seeking
health care [14, 59]. Recent reports based on various surveys showed that only a small
percentage (less than 40%) of India’s population availed themselves of any kind of health
insurance protection [60–62]; Kerala is also struggling to improve its health insurance
coverage [59]. The private health-care sector plays a significant role in Kerala’s health-care
system and is considered to be the highest compared to other states [31]. Some reports claim
that it was slightly above 90%. Moreover, it was revealed that the people in Kerala fell below
the poverty line because of costly treatment-related expenses, which are the highest in the
country [10, 31, 63]. Catastrophic health expenditure after an acute heart failure treatment
was reported in around 80% of the families [10]. An increase in early-onset lifestyle and
vascular illnesses have propelled a large number of families toward financial crisis [64].
The 12th five-year plan aimed to provide comprehensive financial risk protection to the
public and emphasized various health insurance and reimbursement schemes under state and
central governments. Nevertheless, many recent surveys reported that Kerala has not yet
achieved significant improvement in this sector [10, 46, 65]. Most of the government initiatives
failed to reach the poor and needy communities in the state [65]. The official report states that
the outreach of ambitious public health insurance programs under the aegis of Comprehensive
Health Insurance Agency, Kerala (CHIAK) is making substantial progress, with a total
enrolment of around 4,100,000 families [66]. However, the scope of this scheme has limited
penetration and restricted specialty treatment access and financial support [46, 65, 67–70].
Sometimes, the disease event itself was high in the population group, leading to un-availed
health security [10]. Despite all the efforts made by the government and private insurance
facilities, socio-economic status, employment and disease profile have an adverse impact on
insurance coverage in the state [46, 48, 65, 68]. One of the futuristic approaches the state
District MCH GH DH TH Beds/10,000
Trivandrum 1 2 2 6 18.48
Kollam 1* 0 1 8 6.59
Kottayam 1 4 0 3 15.37
Alappuzha 1 1 1 7 16.35
Pathanamthitta 1* 2 1 4 11.31
Idukki 1* 0 1 4 7.28
Ernakulam 1 2 1 11 9.92
Thrissur 1 2 1 6 11.23
Malappuram 1 1 3 6 8.6
Kozhikode 1 1 1 7 12.35
Palakkad 1* 0 1 6 4.88
Kannur 1 1 1 7 21.63
Wayanad 0 1 1 2 8.69
Kasargod 0 1 1 2 6.3
Source(s): Directorate of health sciences 2011, 2013 [58]
Abbreviations: MCH – Medical college hospital, GH – general hospital, DH – district hospital, TH – taluk
hospital, * – not fully functional
Table 2.
Distribution of public
modern medicine
institutions across
Kerala
JHR
36,2
248

government recently implemented is offering emergency care to all without the immediate
payment of hospital bills, even in the private sector, but some of the reported limitations of
this program include confusion among the public and late catastrophic issues [53, 71]. Apart
from its highest educational achievements and robust health system, Kerala is known for its
low GDP; this can impact insurance coverage. In reality, experts state that the neediest
marginal population is devoid of financial protection during an adverse disease event
[14, 46, 48, 65, 72, 73].
Discussion
Kerala’s health system is unique, not only in India but also at a global level because it has
accomplished more from less [74]. Its asymmetrical development has been one of the most
discussed topics for decades, considering that it maintained high health-care standards while
struggling with sluggish economic growth. However, experts reveal that some risks have
emerged in this unique community, the most obvious being the increase in the number of
morbid populations with a lower mortality rate. Various studies have mentioned the
increasing burden of NCDs and the challenges in managing them.
From the data obtained, a model illustrating inter-related health system issues was
synthesized (Figure 3). These issues are discussed in detail under the results section. The
authors believe that these represent a potential research agenda on the Kerala health system.
Several studies and reports stated the higher prevalence of NCDs in the state such as heart
disease, stroke, hypertension and diabetes. Often, this observation is explained as the result
of increased life expectancy as a higher number of aged individuals suffer from chronic
illnesses. However, the life-course perspective is often overlooked. Future studies related to
risk factors and an upstream determinant of NCDs is necessary for the community.
From the data obtained, it is clear that about 30% of the total mortality in Kerala involves
people below 64 years of age. Unfortunately, medically certified deaths represent only 11% of
all registered deaths. As a result, less is known about the cause of deaths that occurred
outside medical environments. Improving mortality data is important not only to enrich data
but also to shed light on reasons for not seeking medical care during terminal illnesses.
Studies show that emergency health-care utilization of the public in the state is low. This
will create socio-economic shifts like increased disability-adjusted life years and long-term
care costs. Factors embedded in the population for this behavior are infrequently studied and
mentioned. Some of the literature reported reduced awareness and socio-economic factors as
the reasons; however, most of the data are limited due to a narrow target population or limited
sample size.
• Low mortality with high morbidity
• Increased burden of non-communicable diseases
• Low compliance toward emergency health-care ulizaon
• High disability adjusted life years (DALY)/ long-term
• Low insurance or other reimbursement coverage
• Long-term economic burden
Figure 3.
Synthesized health
economic model
Health systems
of Kerala
249

One major study [8] suggested that patients took multiple stops before reaching the
appropriate specialty center. However, it remained unclear whether delays were due to health
system inefficiencies, or patient-related factors, or patient’s family-related factors. Studies
related to the efficiency of the health system, including the referral system, in managing
emergency vascular diseases are important. Further, public awareness about and access to
specialty centers needs to be studied to inform health system development efforts. We
suggest future studies on emergency medical care in Kerala to focus on the socio-economic
status, access and quality of care, as suggested by the widely used three delays concept.
Based on the results presented, it is clear that delay in the golden hour treatment can result in
disability or long-term medical care. One study showed that 80% of the families faced
catastrophic health spending in the state after a cardiac failure. Further studies to compare
the medical expenses in patients who availed themselves of golden treatment and those who
did not receive it could enhance insight into the cost-benefit of golden treatment, including a
comparison of mortality rates, length of hospital stay and quality of life after treatment.
Another interesting factor is the observable disparity in the socio-economic status and
health-care delivery in various regions of the state, such as rural–urban and north–south
regional disparities. Differences are observed even within certain rural or urban communities
based on the financial strata. Based on the evidence, high out-of-pocket expenditure is
considered one of the major issues, which is making health financing more complex in the state.
Although government-provided health insurance and reimbursement made significant
progress in the state, out-of-pocket health-related expenses remain high. Studies related to the
various health insurance schemes are needed. These should include coverage of diseases and
a co-payment policy for health expenditures. Further, homogeneity of the health-care cost
across the state within and between public and private health-care providers is another
recommended research area.
Finally, the interactions of the various issues raised were not clearly discussed in the
selected literature. Future studies could include a focus on the relationship between insurance
coverage and health-care utilization, and insurance coverage versus subscriber and disease
profile.
Conclusion
This scoping review revealed emerging challenges in Kerala’s health system in relation to the
rise of NCDs and identified various research needs that could contribute to further the
development of Kerala’s health system. Based on the study findings, a structured health
economic survey study is already under process and has been planned to be completed by
2021. In addition, the scope for future research on Kerala’s health system includes:
(1) research on pathways to address root causes of NCDs in the state, (2) determine socio-
economic and health system factors that shape health-seeking behaviors of the Kerala
community, (3) evaluation of regional differences in health system performance within the
state and (4) causes of high out-of-pocket expenditure within the state.
Conflict of Interest: None
References
1. India, Ministry of Health and Family Welfare. National health policy 2017. [cited 2020 March].
Available from: https://www.nhp.gov.in//NHPfiles/national_health_policy_2017.pdf.
2. Chokshi M, Patil B, Khanna R, Neogi SB, Sharma J, Paul VK, et al. Health systems in India. J
Perinatol. 2016; 36(Suppl.3): S9-12. doi: 10.1038/jp.2016.184.
3. Kumar BG. Low mortality and high morbidity in Kerala reconsidered. Popul Dev Rev. 1993; 19(1):
103-21. doi: 10.2307/2938386.
JHR
36,2
250

4. Arokiasamy P. India’s escalating burden of non-communicable diseases. Lancet Glob Health.
2018; 6(12): e1262-3. doi: 10.1016/S2214-109X(18)30448-0.
5. Zachariah G, Padinharepurayil M, Narayanan KM. A Kerala model for cardiovascular research?.
Indian Heart J. 2016; 68(6): 862-5. doi: 10.1016/j.ihj.2016.06.002.
6. Panikar PGK. Fall in mortality rates in Kerala: an Explanatory hypothesis. Econ Polit Wkly. 1975;
10(47): 1811-8.
7. Thayyil J, Jayakrishnan T. Morbidity and health Care expenditure in Kerala. The 23rd
International Conference on Health and Development Issues, Strategies and Options, Kannur
University, Thalassery. Kerala. School of Development Studies, Kannur University; 2008.
8. Ashraf VV, Maneesh M, Praveenkumar R, Saifudheen K, Girija AS. Factors delaying hospital
arrival of patients with acute stroke. Ann Indian Acad Neurol. 2015; 18(2): 162-6. doi: 10.4103/
0972-2327.150627.
9. Clark EG, Watson J, Leemann A, Breaud AH, Feeley FG, Wolff J, et al. Acute care needs in an
Indian emergency department: a retrospective analysis. World J Emerg Med. 2016; 7(3): 191-5. doi:
10.5847/wjem.j.1920-8642.2016.03.005.
10. Daivadanam M, Thankappan KR, Sarma PS, Harikrishnan S. Catastrophic health expenditure &
coping strategies associated with acute coronary syndrome in Kerala, India. Indian J Med Res.
2012; 136(4): 585-92.
11. Soman CR, Kutty VR, Safraj S, Vijayakumar K, Rajamohanan K, Ajayan K, et al. All-cause
mortality and cardiovascular mortality in Kerala state of India: results from a 5-year follow-up of
161,942 rural community dwelling adults. Asia Pac J Public Health. 2011; 23(6): 896-903. doi: 10.
1177/1010539510365100.
12. Thomas MB, James KS. Changes in mortality and human longevity in Kerala: are they leading to
the advanced stage?. Glob Health Action. 2014; 7: 22938. doi: 10.3402/gha.v7.22938.
13. Menon GR, Singh L, Sharma P, Yadav P, Sharma S, Kalaskar S, et al. National Burden Estimates
of healthy life lost in India, 2017: an analysis using direct mortality data and indirect disability
data. Lancet Global Health. 2019; 7(12): E1675-84. doi: 10.1016/S2214-109x(19)30451-6.
14. Mukherjee S, Haddad S, Narayana D. Social class related inequalities in household health
expenditure and economic burden: evidence from Kerala, south India. Int J Equity Health. 2011;
10: 1. doi: 10.1186/1475-9276-10-1.
15. Krishnan MN, Zachariah G, Venugopal K, Mohanan PP, Harikrishnan S, Sanjay G, et al.
Prevalence of coronary artery disease and its risk factors in Kerala, South India: a community-
based cross-sectional study. BMC Cardiovasc Disord. 2016; 16: 12. doi: 10.1186/s12872-016-0189-3.
16. Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, et al. Thrombolysis with
alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359(13): 1317-29. doi: 10.
1056/NEJMoa0804656.
17. Dandona L, Katoch VM, Dandona R. Research to achieve health care for all in India. Lancet. 2011;
377(9771): 1055-7. doi: 10.1016/S0140-6736(10)62034-X.
18. Bhargava B, Paul VK. Informing NCD control efforts in India on the eve of Ayushman Bharat.
Lancet. 2018. doi: 10.1016/S0140-6736(18)32172-X.
19. Government of Kerala, Thiruvananthapuram State Planning Board. Twelfth five year plan (2012–
2017): report of the expert committee on health. [updated 2014 Nov; cited 2020 March]. Available
from: https://kerala.gov.in/documents/10180/2926ef37-1cff-452b-83f3-69473c1a7707.
20. Suryanarayana MH. Morbidity and health care in Kerala: a distributional profile and implications.
Mumbai: Indira Gandhi Institute of Development Research; 2008.
21. Patel A, Mohanan PP, Prabhakaran D, Huffman MD. Pre-hospital acute coronary syndrome care in
Kerala, India: a qualitative analysis. Indian Heart J. 2017; 69(1): 93-100. doi: 10.1016/j.ihj.2016.07.011.
22. Mohanan PP, Mathew R, Harikrishnan S, Krishnan MN, Zachariah G, Joseph J, et al. Presentation,
management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India:
Health systems
of Kerala
251

results from the Kerala ACS Registry. Eur Heart J. 2013; 34(2): 121-9. doi: 10.1093/eurheartj/
ehs219.
23. Dandona L, Dandona R, Kumar GA, Shukla DK, Paul VK, Balakrishnan K, et al. Nations within a
nation: variations in epidemiological transition across the states of India, 1990–2016 in the global
burden of disease study. Lancet. 2017; 390(10111): 2437-60. doi: 10.1016/S0140-6736(17)32804-0.
24. Harikrishnan S, Jeemon P, Prabhakaran D, Vijayaraghavan G, Bahuleyan CG, Suresh K, et al.
PM148 Differences in the presentation, management and outcomes among patients presenting to
cardiologists and non-cardiologists in Kerala, India. Results from the Kerala Acute Coronary
Syndrome Registry. Global Heart. 2014; 9(Suppl.1): e92. doi: 10.1016/j.gheart.2014.03.1541.
25. Kumar SK. Kerala model of development - critical analysis and a design for the future. Pilani:
Birla Institute of Technology and Science; 2013.
26. Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, et al. The increasing burden of
diabetes and variations among the states of India: the Global Burden of Disease Study 1990-2016.
Lancet Global Health. 2018; 6(12): E1352-62. doi: 10.1016/S2214-109x(18)30387-5.
27. Kutty VR, Soman CR, Joseph A, Pisharody R, Vijayakumar K. Type 2 diabetes in southern Kerala:
variation in prevalence among geographic divisions within a region. Natl Med J India. 2000;
13(6): 287-92.
28. India, Ministry of Home Affairs. Office of the Registrar General. Report on medical certification of
cause of death 2015. New Delhi: Office of the Registrar General; 2017.
29. Bhatia S. Public health expenditure and health status in India: an inter-state analysis. Amritsar:
Guru Nanak Dev University; 2011.
30. Prabhakaran D, Jeemon P, Sharma M, Roth GA, Johnson C, Harikrishnan S, et al. The changing
patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden
of Disease Study 1990-2016. Lancet Glob Health. 2018; 6(12): e1339-51. doi: 10.1016/s2214-109x(18)
30407-8.
31. Wilson C. Dis-embedding health care: marketisation and the rising cost of medicine in Kerala,
South India. JS Asian Dev. 2009; 4(1): 83-101. doi: 10.1177/097317410900400106.
32. Yoo SGK, Davies D, Mohanan PP, Baldridge AS, Charles PM, Schumacher M, et al. Hospital-Level
cardiovascular management practices in Kerala, India. Circ Cardiovasc Qual Outcomes. 2019;
12(5): e005251. doi: 10.1161/CIRCOUTCOMES.118.005251.
33. Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute
cardiovascular disease and stroke, 1999-2011. Circulation. 2014; 130(12): 966-75. doi: 10.1161/
CIRCULATIONAHA.113.007787.
34. Pillai RK, Williams SV, Glick HA, Polsky D, Berlin JA, Lowe RA. Factors affecting decisions to
seek treatment for sick children in Kerala, India. Soc Sci Med. 2003; 57(5): 783-90. doi: 10.1016/
s0277-9536(02)00448-3.
35. Dilip TR. Age-specific analysis of reported morbidity in Kerala, India. World Health Popul. 2007;
9(4): 98-108. doi: 10.12927/whp.2007.19527.
36. Rachmawati D, Ningsih D, Andarini S. Factors affecting knowledge towards stroke risks and
early symptoms in emergency department. Malang Neurology Journal. 2020; 6(1): 11-9. doi: 10.
21776/ub.mnj.2020.006.01.3.
37. Mohan B, Bansal R, Dogra N, Sharma S, Chopra A, Varma S, et al. Factors influencing prehospital
delay in patients presenting with ST-elevation myocardial infarction and the impact of
prehospital electrocardiogram. Indian Heart J. 2018; 70(Suppl.3): S194-8. doi: 10.1016/j.ihj.2018.
10.395.
38. Fladt J, Meier N, Thilemann S, Polymeris A, Traenka C, Seiffge DJ, et al. Reasons for prehospital
delay in acute ischemic stroke. J Am Heart Assoc. 2019; 8(20): e013101. doi: 10.1161/JAHA.119.
013101.
39. Pulvers JN, Watson JDG. If time is brain where is the improvement in prehospital time after
stroke?. Front Neurol. 2017; 8: 617. doi: 10.3389/fneur.2017.00617.
JHR
36,2
252

40. McVerry F, Hunter A, Dynan K, Matthews M, McCormick M, Wiggam I, et al. Country-wide
analysis of systemic factors associated with acute ischemic stroke door to needle time. Front
Neurol. 2019; 10: 676. doi: 10.3389/fneur.2019.00676.
41. Huffman MD, Mohanan PP, Devarajan R, Baldridge AS, Kondal D, Zhao L, et al. Effect of a
quality improvement intervention on clinical outcomes in patients in India with acute myocardial
infarction: the ACS QUIK randomized clinical trial. JAMA. 2018; 319(6): 567-78. doi: 10.1001/jama.
2017.21906.
42. Nambiar M, Nedungalaparambil NM, Aslesh OP. Is current training in basic and advanced
cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst
healthcare professionals of North-Kerala. World J Emerg Med. 2016; 7(4): 263-9. doi: 10.5847/wjem.
j.1920-8642.2016.04.004.
43. Haddad S, Narayana D, Mohindra K. Reducing inequalities in health and access to health care in a
rural Indian community: an India-Canada collaborative action research project. BMC Int Health
Hum Rights. 2011; 11(Suppl.2): S3. doi: 10.1186/1472-698X-11-S2-S3.
44. World Bank Group. Kerala: poverty, growth and inequality. Washington, DC: World Bank
Group; 2017.
45. Deshpande A. Does caste still define disparity? A look at inequality in Kerala, India. Am Econ
Rev. 2000; 90(2): 322-5.
46. Vellakkal S. Determinants of enrolment in voluntary health insurance: evidences from a mixed
method study, Kerala, India. Int J Financ Res. 2013; 4(2): 99-107. doi: 10.5430/ijfr.v4n2p99.
47. Jacob S. The Kerala regime and regional disparities in health infrastructure versus outcomes.
India Rev. 2014; 13(1): 58-77. doi: 10.1080/14736489.2014.873680.
48. Dilip TR. Utilization of inpatient care from private hospitals: trends emerging from Kerala, India.
Health Policy Plan. 2010; 25(5): 437-46. doi: 10.1093/heapol/czq012 .
49. Jana A, Basu R. Examining the changing health care seeking behavior in the era of health sector
reforms in India: evidences from the National Sample Surveys 2004 & 2014. Glob Health Res
Policy. 2017; 2: 6. doi: 10.1186/s41256-017-0026-y.
50. Saikia N, Kulkarni PM. Data for research into health inequality in India. Do we have enough?.
Econ Polit Wkly. 2016; 51(26–27): 111-6.
51. Nandraj S. Private healthcare providers in India are above the law, leaving patients without
protection. BMJ. 2015; 350: h675. doi: 10.1136/bmj.h675.
52. Gadre A. India’s private healthcare sector treats patients as revenue generators. BMJ. 2015; 350:
h826. doi: 10.1136/bmj.h826.
53. Jain Y, Patil SB, Phutke GB. Sustaining for-profit emergency healthcare services in low resource
areas. Indian J Med Ethics. 2018; 3(4): 334-6. doi: 10.20529/IJME.2018.062.
54. Malhotra C, Do YK. Socio-economic disparities in health system responsiveness in India. Health
Policy Plan. 2013; 28(2): 197-205. doi: 10.1093/heapol/czs051.
55. Rajeev S. Government health services in Kerala: who benefits?. Econ Polit Wkly. 2001; 36(32): 3071-7.
56. Thresia CU. Health inequalities in South Asia at the launch of sustainable development goals:
exclusions in health in Kerala, India need political interventions. Int J Health Serv. 2018; 48(1):
57-80. doi: 10.1177/0020731417738222.
57. Nair LR, Mathew DM, Samarasinghe A, Pozvek M, Yakobe P, Pandey SR, et al. Public and private
healthcare institutions: preference and expenditure pattern. [updated 2017 Jun; cited 2020 March].
Available from: https://www.cppr.in/wp-content/uploads/2017/06/Public-and-Private-Healthcare-
Institutions-Preference-and-Expenditure-Pattern.pdf.
58. Kerala, Directorate of Health Services. Health at a glance. Kerala: Directorate of Health
Services; 2018.
59. Mohanan PP, Huffman MD, Baldridge AS, Devarajan R, Kondal D, Zhao L, et al. Microeconomic
costs, insurance, and catastrophic health spending among patients with acute myocardial
Health systems
of Kerala
253

infarction in India: substudy of a randomized clinical trial. JAMA Netw Open. 2019; 2(5): e193831.
doi: 10.1001/jamanetworkopen.2019.3831.
60. Anand N. India’s so poorly insured that the family of the deceased gets less than 10% of what it
needs 2019. [updated 2019 Jan 16; cited 2020 March]. Available from: https://qz.com/india/
1525202/life-insurance-coverage-in-india-is-abysmal-says-indiaspend/.
61. Sanghvi D. 56% Indians still don’t have a health cover. [updated 2018 Dec 4; cited 2020 March].
Avail able from: https://www.livemint.com/Money/YopMGGZH7w65WTTxgPLoSK/56-Indians-
still-dont-have-a-health-cover.html.
62. Shoree S, Ruchismita R, Desai KR. Evaluation of RSBY’s key performance indicators: a biennial
study. (Research paper no. 42). Geneva: International Labour Organization; 2014.
63. Narayanan N, Kodali PB. Out of pocket health expenditure and catastrophic health expenditure
among the beneficiaries of comprehensive health insurance scheme in Kerala. Int J Health Sci Res.
2018; 8(9): 207-14.
64. Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and
future directions. Circulation. 2016; 133(16): 1605-20. doi: 10.1161/CIRCULATIONAHA.114.008729.
65. Philip NE, Kannan S, Sarma SP. Utilization of comprehensive health insurance scheme, Kerala: a
comparative study of insured and uninsured below-poverty-line households. Asia Pac J Public
Health. 2016; 28(Suppl.1): 77s-85s. doi: 10.1177/1010539515602306.
66. Kerala, State Planning Board. Economic review 2017. Thiruvananthapuram: State Planning
Board; 2017.
67. Ahlin T, Nichter M, Pillai G. Health insurance in India: what do we know and why is ethnographic
research needed. Anthropol Med. 2016; 23(1): 102-24. doi: 10.1080/13648470.2015.1135787.
68. Devi Nair V. Comprehensive health insurance scheme and health care utilization: a case study
among insured households in Kerala, India. Value Health. 2014; 17(7): A790. doi: 10.1016/j.jval.
2014.08.433.
69. Vijay A, Krishnaveni V. The role of awareness on the level of satisfaction among health insurance
policy-holders with special reference to Ernakulam district, Kerala. Indian J Public Health Res
Dev. 2018; 9(12): 15-20.
70. Varghese T. Determinants of consumer purchase decisions of health insurance in Kerala. Cochin:
Cochin University of Science and Technology; 2013.
71. National Rural Health Mission. Kerala emergency medical services project (KEMP). Kerala:
National Rural Health Mission; 2010.
72. Nair V, Thankappan K, Sarma P, Vasan R. Changing roles of grass-root level health workers in
Kerala, India. Health Policy Plan. 2001; 16(2): 171-9. doi: 10.1093/heapol/16.2.171.
73. Balarajan Y, Selvaraj S, Subramanian SV. Health care and equity in India. Lancet. 2011; 377(9764):
505-15. doi: 10.1016/S0140-6736(10)61894-6.
74. Brown A. Growth and success in Kerala. The Yale Review of International Studies. 2013;
4(1): 85-96.
Corresponding author
For instructions on how to order reprints of this article, please visit our website:
www.emeraldgrouppublishing.com/licensing/reprints.htm
JHR
36,2
254
