
Morbidity and Mortality Weekly Report
Weekly / Vol. 70 / No. 35 September 3, 2021
Continuing Education examination available at
https://www.cdc.gov/mmwr/mmwr_continuingEducation.html
National, Regional, State, and Selected Local Area Vaccination Coverage
Among Adolescents Aged 13–17 Years — United States, 2020
Cassandra Pingali, MPH, MS
1
; David Yankey, PhD
1
; Laurie D. Elam-Evans, PhD
1
; Lauri E. Markowitz, MD
2
; Charnetta L. Williams, MD
1
;
Benjamin Fredua, MS
1,3
; Lucy A. McNamara, PhD
4
; Shannon Stokley, DrPH
1
; James A. Singleton, PhD
1
The Advisory Committee on Immunization Practices
(ACIP) recommends that adolescents aged 11–12 years
routinely receive tetanus, diphtheria, and acellular pertussis
(Tdap); meningococcal conjugate (MenACWY); and human
papillomavirus (HPV) vaccines. Catch-up vaccination is
recommended for hepatitis B (HepB); hepatitis A (HepA);
measles, mumps, and rubella (MMR); and varicella (VAR)
vaccines for adolescents whose childhood vaccinations are
not current. Adolescents are also recommended to receive a
booster dose of MenACWY vaccine at age 16 years, and shared
clinical decision-making is recommended for the serogroup B
meningococcal vaccine (MenB) for persons aged 16–23 years
(1). To estimate coverage with recommended vaccines, CDC
analyzed data from the 2020 National Immunization Survey–
Teen (NIS-Teen) for 20,163 adolescents aged 13–17 years.*
Coverage with ≥1 dose of HPV vaccine increased from 71.5%
in 2019 to 75.1% in 2020. The percentage of adolescents
* Eligible participants were born during January 2002–January 2008. Tetanus
toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine represents
coverage with ≥1 Tdap dose at age ≥10 years. Meningococcal conjugate vaccine
represents coverage with the quadrivalent meningococcal conjugate vaccine or
meningococcal-unknown type vaccine. HPV vaccination coverage includes
receipt of any HPV vaccine and does not distinguish between nine-valent
(9vHPV), quadrivalent (4vHPV), or bivalent (2vHPV) vaccines. Some
adolescents might have received more than the 2 or 3 recommended HPV
vaccine doses. Hepatitis A, hepatitis B, varicella, and measles, mumps, and
rubella vaccines are considered childhood vaccinations and are recommended
for adolescents who are not up to date with these vaccinations. Estimates in
this report include those who might have received vaccinations on-time or as
catch-up. Except as noted, coverage estimates for ≥1 and ≥2 varicella vaccine
doses were obtained among adolescents with no history of varicella disease.
Influenza vaccination coverage data are not included in this report but are
available at https://www.cdc.gov/flu/fluvaxview/index.htm.
INSIDE
1191 Evaluation of Syndromic Surveillance Data
for Studying Harmful Algal Bloom-Associated
Illnesses — United States, 2017–2019
1195 Multiple Variants of SARS-CoV-2 in a University
Outbreak After Spring Break — Chicago, Illinois,
March–May 2021
1201 Screening Programs for SARS-CoV-2 Infections
on a University Campus — Austin, Texas,
September 30–November 30, 2020
1206 COVID-19 Vaccination Coverage Among
Adolescents Aged 12–17 Years — United States,
December 14, 2020–July 31, 2021
1214 Outbreak Associated with SARS-CoV-2 B.1.617.2
(Delta) Variant in an Elementary School — Marin
County, California, May–June 2021
1220 COVID-19 Case Rates in Transitional Kindergarten
Through Grade 12 Schools and in the
Community — Los Angeles County, California,
September 2020–March 2021
1223 Epidemiologically Linked COVID-19 Outbreaks at a
Youth Camp and Men’s Conference — Illinois,
June–July 2021
1228 Association Between COVID-19 and Myocarditis
Using Hospital-Based Administrative Data —
United States, March 2020–January 2021
1233 QuickStats
U.S. Department of Health and Human Services
Centers for Disease Control and Prevention

Morbidity and Mortality Weekly Report
1184 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
The MMWR series of publications is published by the Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention (CDC),
U.S. Department of Health and Human Services, Atlanta, GA 30329-4027.
Suggested citation: [Author names; first three, then et al., if more than six.] [Report title]. MMWR Morb Mortal Wkly Rep 2021;70:[inclusive page numbers].
Centers for Disease Control and Prevention
Rochelle P. Walensky, MD, MPH, Director
Debra Houry, MD, MPH, Acting Principal Deputy Director
Daniel B. Jernigan, MD, MPH, Deputy Director for Public Health Science and Surveillance
Rebecca Bunnell, PhD, MEd, Director, Office of Science
Jennifer Layden, MD, PhD, Deputy Director, Office of Science
Michael F. Iademarco, MD, MPH, Director, Center for Surveillance, Epidemiology, and Laboratory Services
MMWR Editorial and Production Staff (Weekly)
Charlotte K. Kent, PhD, MPH, Editor in Chief
Jacqueline Gindler, MD, Editor
Brian A. King, PhD, MPH, Guest Science Editor
Paul Z. Siegel, MD, MPH, Associate Editor
Mary Dott, MD, MPH, Online Editor
Terisa F. Rutledge, Managing Editor
Teresa M. Hood, MS, Lead Technical Writer-Editor
Leigh Berdon, Glenn Damon, Soumya Dunworth, PhD,
Srila Sen, MA, Stacy Simon, MA,
Jeffrey D. Sokolow, MA, Morgan Thompson,
Technical Writer-Editors
Martha F. Boyd, Lead Visual Information Specialist
Alexander J. Gottardy, Maureen A. Leahy,
Julia C. Martinroe, Stephen R. Spriggs,
Brian Taitt, Tong Yang,
Visual Information Specialists
Quang M. Doan, MBA, Phyllis H. King,
Terraye M. Starr, Moua Yang,
Information Technology Specialists
MMWR Editorial Board
Timothy F. Jones, MD, Chairman
Matthew L. Boulton, MD, MPH
Carolyn Brooks, ScD, MA
Jay C. Butler, MD
Virginia A. Caine, MD
Jonathan E. Fielding, MD, MPH, MBA
David W. Fleming, MD
William E. Halperin, MD, DrPH, MPH
Jewel Mullen, MD, MPH, MPA
Jeff Niederdeppe, PhD
Celeste Philip, MD, MPH
Patricia Quinlisk, MD, MPH
Patrick L. Remington, MD, MPH
Carlos Roig, MS, MA
William Schaffner, MD
Nathaniel Smith, MD, MPH
Morgan Bobb Swanson, BS
Abbigail Tumpey, MPH
Ian Branam, MA,
Acting Lead Health Communication Specialist
Shelton Bartley, MPH,
Lowery Johnson, Amanda Ray,
Jacqueline N. Sanchez, MS,
Health Communication Specialists
Will Yang, MA,
Visual Information Specialist
who were up to date
†
with HPV vaccination (HPV UTD)
increased from 54.2% in 2019 to 58.6% in 2020. Coverage
with ≥1 dose of Tdap, ≥1 dose (and among adolescents
aged 17 years, ≥2 doses) of MenACWY remained similar to
coverage in 2019 (90.1%, 89.3%, and 54.4% respectively).
Coverage increased for ≥2 doses of HepA among adolescents
aged 13–17 years and ≥1 dose of MenB among adolescents
aged 17 years. Adolescents living below the federal poverty
level
§
had higher HPV vaccination coverage than adolescents
living at or above the poverty level. Adolescents living outside
a metropolitan statistical area (MSA)
¶
had lower coverage
with ≥1 MenACWY and ≥1 HPV dose, and a lower propor-
tion being HPV UTD than adolescents in MSA principal
†
Adolescents were considered to be up to date with HPV vaccination if they
had received ≥3 doses, or if each of the following applied: 1) they had received
2 doses; 2) the first dose was received before their 15th birthday; and 3) the
difference between dates of first and second doses was ≥5 months minus
4 days, the absolute minimum interval between the first and second doses.
https://www.cdc.gov/vaccines/programs/iis/cdsi.html
§
Adolescents were classified as being below the federal poverty level if their
total family income was less than the level specified for the applicable family
size and number of children aged <18 years. All others were classified as at or
above the poverty level (https://www.census.gov/data/tables/time-series/demo/
income-poverty/historical-poverty-thresholds.html). Poverty status was
unknown for 711 adolescents.
¶
MSA status was determined from household reported city and county of
residence and was grouped into three categories: MSA principal city, MSA
nonprincipal city, and non-MSA. MSA and MSA principal city were as defined
by the U.S. Census Bureau (https://www.census.gov/programs-surveys/metro-
micro.html). Non-MSA areas include urban populations not located within
an MSA and completely rural areas.
cities. In 2020, the COVID-19 pandemic disrupted routine
immunization services. Results from the 2020 NIS-Teen reflect
adolescent vaccination coverage before the COVID-19 pan-
demic. The 2020 NIS-Teen data could be used to assess the
impact of the COVID-19 pandemic on catch-up vaccination
but not on routine adolescent vaccination because adolescents
included in the survey were aged ≥13 years, past the age when
most routine adolescent vaccines are recommended, and most
vaccinations occurred before March 2020. Continued efforts
to reach adolescents whose routine medical care has been
affected by the COVID-19 pandemic are necessary to protect
persons and communities from vaccine-preventable diseases
and outbreaks.
NIS-Teen is an annual random-digit–dialed telephone
survey** that monitors vaccination coverage in adolescents aged
13–17 years in all 50 states, the District of Columbia, selected
local areas, and some U.S. territories.
††
Parents or guardians of
** Persons living in all identified mobile-telephone households were eligible for
interview. Sampling weights were adjusted for single frame (mobile telephone),
nonresponse, noncoverage, and overlapping samples of mixed telephone users. A
description of NIS-Teen single-frame survey methodology and its effect on reported
vaccination estimates is available at https://www.cdc.gov/vaccines/imz-managers/
coverage/teenvaxview/pubs-presentations/dual-to-single-frame-teen.html.
††
Local areas that received federal immunization funds under Section 317 of
the Public Health Service Act were sampled separately. Those included
Chicago, Illinois; New York, New York; Philadelphia County, Pennsylvania;
Bexar County, Texas; and Houston, Texas. Two territories were sampled
separately in 2020: Guam and Puerto Rico.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1185
US Department of Health and Human Services/Centers for Disease Control and Prevention
eligible adolescents are interviewed to gather sociodemographic
information about the household, and consent to contact the
adolescent’s vaccination provider (or providers) is requested; if
permission is granted, a questionnaire is mailed to the provider
(or providers) to obtain the adolescent’s vaccination history.
Vaccination coverage estimates are based on provider-reported
immunization records and include any vaccines administered
before the 2020 NIS-Teen interview date. This report provides
vaccination coverage estimates for 20,163 adolescents aged
13–17 years.
§§
The overall household response rate
¶¶
was
20.7%; 45.2% of adolescents with completed interviews had
adequate provider data. Data were weighted and analyzed
to account for the complex survey design, and T-tests using
Taylor-series variance estimates were used to assess vaccination
coverage differences by survey year (2020 versus 2019) and
between sociodemographic groups.*** P-values <0.05 were
considered statistically significant. Analyses were conducted
using SAS-callable SUDAAN (version 11; RTI International).
This activity was reviewed by CDC and was conducted
consistent with applicable federal law and CDC policy.
†††
National Vaccination Coverage
In 2020, HPV vaccination coverage (≥1 dose) among
adolescents was 75.1%, and 58.6% were HPV UTD (Figure)
(Table 1). Coverage with ≥1 dose of Tdap and MenACWY
remained high and stable (90.1% and 89.3% respectively).
Among adolescents aged 17 years, coverage with ≥2 doses of
MenACWY was 54.4%, similar to 2019 (53.7%); coverage
increased for ≥1 dose of Men B among adolescents aged
17 years and catchup vaccination with ≥2 doses of HepA
among adolescents 13−17 years from 2019. Coverage surpassed
90% for ≥2 doses of MMR, ≥3 doses of HepB, and ≥1 and
§§
The 2020 NIS-Teen sample included 9,576 females and 10,587 males.
Adolescents from Guam (300), and Puerto Rico (169) were excluded from
the national estimates.
¶¶
The Council of American Survey Research Organizations response rate is
the product of three other rates: 1) the resolution rate (the proportion of
telephone numbers that can be identified as either for business or residence),
2) the screening rate (the proportion of qualified households that complete
the screening process), and 3) the cooperation rate (the proportion of
contacted eligible households for which a completed interview is obtained).
*** The NIS-Teen methodology for weighting and synthesizing provider-reported
vaccination histories has been previously described. https://www.cdc.gov/
vaccines/imz-managers/nis/downloads/NIS-TEEN-PUF19-DUG.pdf
†††
45 C.F.R. part 46.102(l)(2); 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d);
5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
§§§
HepA, HepB, VAR, and MMR vaccines are considered childhood
vaccinations and are recommended for adolescents who are not up to date
with these vaccinations. Estimates in this report include those who might
have received vaccinations on-time or as catch-up.
≥2 doses of varicella vaccine among adolescents without a
history of varicella disease.
§§§
Vaccination Coverage by Selected Characteristics
Among adolescents living in non-MSA areas, vaccination
coverage was lower compared with those living in MSA prin-
cipal cities with ≥1 dose MenACWY (85.7% versus 90.2%
[−4.5 percentage points]), ≥1 dose HPV (68.0% versus 77.8%
[−9.8 percentage points]), and ≥2 doses HepA (76.2% versus
83.6% [−7.4 percentage points])], and being HPV UTD
(49.2% versus 60.4% [−11.2 percentage points]) (Table 2).
These MSA disparities persisted among adolescents at or above
the poverty level but were not significant among those below
the poverty level for HPV UTD status and ≥2 dose–HepA
coverage. The coverage disparity in non-MSA areas compared
with MSA principal cities among adolescents living at or above
the poverty level were largest for HPV UTD status (46.0%
versus 59.8% [−13.8 percentage points]), ≥1-dose HPV cov-
erage (64.9% versus 76.2% [−11.3 percentage points], and
≥2-dose HepA coverage (74.4% versus 83.6% [−9.2 percent-
age points]). Coverage varied by jurisdiction (Supplementary
Table, https://stacks.cdc.gov/view/cdc/109214), race and
ethnicity,
¶¶¶
and health insurance status.****
COVID-19 Pandemic Effects on HPV Vaccination
The COVID-19 pandemic was declared a national emer-
gency on March 13, 2020. To evaluate the impact of the
pandemic on HPV vaccination, CDC conducted two analyses
comparing the 2019 and 2020 NIS-Teen samples. Historically,
HPV vaccination coverage has been lower than coverage with
most other routine vaccines, allowing for more catch-up vacci-
nations among adolescents aged 13–17 years. Most adolescents
had initiated HPV vaccination before March 1 in both survey
¶¶¶
Hispanic adolescents had lower coverage for ≥1 Tdap (−3.9 percentage
points), ≥2 MMR (−4.0 percentage points), ≥3 HepB (−4.3 percentage
points), ≥1 Var (−2.6 percentage points), and ≥2 Var (−3.2 percentage
points) than White adolescents. Black adolescents had lower coverage for
≥2 MenACWY (−2.5 percentage points) than White adolescents. Results
showed higher HPV vaccine coverage (≥1 dose) for Black, Hispanic,
American Indian or Alaska Native, Asian, and multiracial adolescents than
White adolescents. Results also showed higher HPV UTD for Black,
Hispanic, and multiracial adolescents. The higher HPV coverage has been
observed for Black and Hispanic adolescents compared with White
adolescents for several years. https://www.cdc.gov/vaccines/imz-managers/
coverage/teenvaxview/pubs-presentations/NIS-teen-vac-coverage-estimates-
2020-tables.html#table-01
**** Adolescents with any Medicaid insurance had lower coverage for ≥1 Tdap
(−3.1 percentage points) but higher coverage with ≥1 HPV (6.1 percentage
points) compared with adolescents with private health insurance.
Adolescents who were uninsured had lower coverage for all routine
vaccinations (Tdap, MenACWY, and HPV vaccines) compared with
adolescents with private health insurance. https://www.cdc.gov/vaccines/
imz-managers/coverage/teenvaxview/pubs-presentations/NIS-teen-vac-
coverage-estimates-2020-tables.html#table-02

Morbidity and Mortality Weekly Report
1186 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE. Estimated vaccination coverage with selected vaccines and doses* among adolescents aged 13–17 years, by survey year
†
— National
Immunization Survey–Teen,
§,¶
United States, 2006–2020
0
20
40
60
80
100
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020
Percentage vaccinated
Year
≥1 Tdap
≥1 MenACWY
≥2 MenACWY
≥1 HPV vaccine
≥3 HPV vaccine
HPV UTD
2011–2015 ACIP
recommendation
2016 ACIP
recommendation
Single mobile telephone
sampling frame estimates
Abbreviations: ACIP = Advisory Committee on Immunization Practices; HPV = human papillomavirus; MenACWY = quadrivalent meningococcal conjugate vaccine;
NIS-teen = National Immunization Survey–Teen; Tdap = tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine; UTD = up to date.
* ≥1 dose Tdap at age ≥10 years; ≥1 dose MenACWY or meningococcal-unknown type vaccine; ≥2 doses MenACWY or meningococcal-unknown type vaccine,
calculated only among adolescents aged 17 years at time of interview. Does not include adolescents who received their first and only dose of MenACWY at age
≥16 years; HPV vaccine, nine-valent (9vHPV), quadrivalent (4vHPV), or bivalent (2vHPV). The routine ACIP recommendation for HPV vaccination was made for females
in 2006 and for males in 2011. Because HPV vaccination was recommended for males in 2011, coverage for all adolescents was not measured before that year; HPV
UTD includes those with ≥3 doses, and those with 2 doses when the first HPV vaccine dose was initiated at age <15 years and at least 5 months minus 4 days elapsed
between the first and second dose.
†
NIS-Teen implemented a revised adequate provider data definition in 2014 and retrospectively applied the revised definition to 2013 data. Estimates using a revised
definition might not be directly comparable.
§
NIS-Teen moved in 2018 to a single-sample frame.
¶
ACIP revised the recommended HPV vaccination schedule in late 2016. The schedule changed from a 3-dose to 2-dose series with appropriate spacing between
receipt of the first and second dose for immunocompetent adolescents initiating the series before the 15th birthday. Three doses are still recommended for adolescents
initiating the series at age ≥15 years. Because of the change in definition, the graph includes estimates for ≥3 doses of HPV during 2011–2015 and the HPV UTD
estimate for 2016–2020. Because HPV vaccination was recommended for males in 2011, coverage for all adolescents was not measured before that year.
years (69.1% in 2019 and 73.6% in 2020). An additional 2.4%
and 1.5% of adolescents initiated the series after this date in
2019 and 2020, respectively.
The second analysis evaluated adolescents in the 2020
NIS-Teen sample who had not received HPV vaccine before
March 1 and whose parent or guardian was interviewed on
or after that date. This cohort was compared with a similarly
constructed cohort using 2019 NIS-Teen data. Cumulative
daily HPV vaccination initiation estimates from March
through December for these cohorts were calculated using the
††††
Kaplan-Meier methods were used to calculate cumulative daily vaccination
estimates from March–December 2019 and from March–December 2020.
In 2019, 4,918 adolescents had not received a dose of HPV vaccine and
had not been interviewed as of March 1, 2019; 452 were vaccinated between
March–December 2019. In 2020, 4,527 adolescents had not received a
dose of HPV vaccine and had not been interviewed as of March 1, 2020;
282 were vaccinated between March–December 2020.
Kaplan-Meier method.
††††
Among the 4,918 adolescents who
had not received HPV vaccine as of March 1, 2019 (26.2%
of the total sample), 452 (15.0%) initiated the series by mid-
December 2019. Among the 4,527 adolescents who had not
received HPV vaccine as of March 1, 2020, (22.5% of total
sample), 282 (15.2%) initiated the series by mid-December
2020. HPV vaccination initiation in the 2020 cohort was
lower than that in the 2019 cohort by April. The difference
between the two cohorts was largest in August and September
(4.9 percentage points lower in 2020 in both months) but nar-
rowed in subsequent months and was no longer significant by
end of November (Supplementary Figure, https://stacks.cdc.
gov/view/cdc/109215).

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1187
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Estimated vaccination coverage with selected vaccines and doses among adolescents aged 13–17* years, by age at interview —
National Immunization Survey–Teen, United States, 2020
Vaccine
Age at interview (yrs), % (95% CI)
†
Total, % (95% CI)
†
13 14 15 16 17 2020 2019
(n = 4,276) (n = 4,173) (n = 3,998) (n = 4,028) (n = 3,688) (N = 20,163) (N = 18,788)
Tdap
§
≥1 dose 88.9 (87.0–90.6) 89.4 (87.1–91.3) 90.7 (88.7–92.5) 90.4 (88.3–92.1) 91.1 (88.7–93.0) 90.1 (89.2–90.9) 90.2 (89.2–91.1)
MenACWY
¶
≥1 dose 87.5 (85.3–89.4) 87.6 (85.0–89.8) 90.4 (88.6–92.0)** 89.1 (86.9–91.0) 92.3 (90.3–93.9)** 89.3 (88.4–90.2) 88.9 (88.0–89.8)
≥2 doses
††
NA NA NA NA 54.4 (51.2–57.5) 54.4 (51.2–57.5) 53.7 (49.9–57.4)
HPV
§§
vaccine
All adolescents
≥1 dose 69.4 (66.6–72.1) 72.3 (69.4–75.0) 77.6 (75.3–79.8)** 77.2 (74.7–79.6)** 79.0 (76.4–81.4)** 75.1 (73.9–76.2)
¶¶
71.5 (70.1–72.8)
HPV UTD*** 45.6 (42.7–48.5) 56.0 (53.0–58.9)** 61.9 (58.9–64.7)** 65.5 (62.6–68.2)** 64.5 (61.5–67.4)** 58.6 (57.3–60.0)
¶¶
54.2 (52.7–55.8)
Females
≥1 dose 71.3 (67.7–74.7) 72.9 (68.4–77.0) 78.1 (74.6–81.3)** 80.3 (76.3–83.8)** 83.5 (80.8–85.9)** 77.1 (75.4–78.7)
¶¶
73.2 (71.3–75.0)
HPV UTD 48.4 (44.3–52.5) 57.2 (52.6–61.7)** 63.7 (59.4–67.8)** 68.5 (64.0–72.6)** 70.4 (66.6–73.9)** 61.4 (59.5–63.3)
¶¶
56.8 (54.6–59.0)
Males
≥1 dose 67.5 (63.2–71.5) 71.7 (67.9–75.2) 77.1 (73.9–80.1)** 74.5 (71.1–77.6)** 74.8 (70.4–78.6)** 73.1 (71.5–74.8)
¶¶
69.8 (67.9–71.7)
HPV UTD 42.7 (38.6–46.9) 54.8 (50.9–58.6)** 60.0 (56.1–63.9)** 62.8 (58.9–66.4)** 59.0 (54.4–63.5)** 56.0 (54.1–57.8)
¶¶
51.8 (49.7–53.9)
MenB ≥1 dose
†††
NA NA NA NA 28.4 (25.5–31.5) 28.4 (25.5–31.5)
¶¶
21.8 (18.9–24.9)
MMR ≥2 doses 92.5 (90.7–94.0) 92.1 (90.3–93.5) 92.5 (90.4–94.2) 93.2 (91.5–94.7) 91.6 (89.2–93.5) 92.4 (91.6–93.2) 91.9 (90.8–92.8)
Hepatitis A vaccine
≥2 doses
§§§
86.5 (84.1–88.5) 84.9 (82.6–86.9) 81.5 (79.1–83.6)** 79.8 (77.5–81.8)** 77.7 (75.0–80.1)** 82.1 (81.1–83.1)
¶¶
77.1 (75.8–78.4)
Hepatitis B vaccine
≥3 doses
91.8 (89.8–93.4) 93.5 (92.1–94.8) 92.5 (90.7–94.0) 93.6 (92.0–94.8) 91.4 (89.1–93.3) 92.6 (91.8–93.3) 91.6 (90.6–92.6)
Varicella
History of varicella
¶¶¶
6.8 (5.4–8.5) 6.9 (5.7–8.3) 8.7 (7.1–10.6) 7.6 (6.4–9.1) 12.0 (9.7–14.8)** 8.4 (7.6–9.2) 9.1 (8.4–9.9)
No history of varicella disease
≥1 dose vaccine 96.2 (94.8–97.2) 95.9 (94.4–97.0) 95.3 (93.5–96.7) 95.3 (93.3–96.7) 95.2 (93.6–96.5) 95.6 (94.9–96.2) 95.2 (94.3–95.9)
≥2 doses vaccine 93.6 (92.0–95.0) 91.6 (89.6–93.2) 92.8 (90.6–94.5) 90.8 (88.3–92.9)** 90.5 (88.1–92.5)** 91.9 (91.0–92.7) 90.6 (89.5–91.7)
History of varicella or
received ≥2 doses
varicella vaccine
94.1 (92.6–95.3) 92.1 (90.3–93.6) 93.4 (91.4–95.0) 91.5 (89.2–93.4) 91.6 (89.5–93.4)** 92.6 (91.7–93.3) 91.5 (90.4–92.4)
Abbreviations: CI = confidence interval; HPV = human papillomavirus; MenACWY = quadrivalent meningococcal conjugate vaccine; MenB = serogroup B meningococcal
vaccine; MMR = measles, mumps, and rubella vaccine; NA = not applicable; NIS-Teen = National Immunization Survey–Teen; Tdap = tetanus toxoid, reduced diphtheria
toxoid, and acellular pertussis vaccine; UTD = up to date.
* Adolescents (20,163) in the 2020 NIS-Teen were born during January 2002–January 2008.
†
Estimates with 95% CI widths >20 might be unreliable.
§
Includes percentages receiving Tdap vaccine at age ≥10 years.
¶
Includes percentages receiving MenACWY or meningococcal-unknown type vaccine.
** Statistically significant difference (p<0.05) in estimated vaccination coverage by age: reference group was adolescents aged 13 years.
††
≥2 doses of MenACWY or meningococcal-unknown type vaccine. Calculated only among adolescents who were aged 17 years at interview. Does not include
adolescents who received 1 dose of MenACWY vaccine at age ≥16 years.
§§
HPV vaccine, nine-valent (9vHPV), quadrivalent (4vHPV), or bivalent (2vHPV). For ≥1 HPV dose measure and HPV-UTD measure, percentages are reported among
females and males combined (20,163) and among females only (9,576) and among males only (10,587).
¶¶
Statistically significant difference (p<0.05) compared with 2019 NIS-Teen estimates.
*** HPV UTD includes those with ≥3 doses, and those with 2 doses when the first HPV vaccine dose was initiated before age 15 years and there was at least 5 months
minus 4 days between the first and second dose. This update to the HPV recommendation occurred in December 2016.
†††
≥1 dose of MenB. Calculated only among adolescents who were aged 17 years at interview. Administered based on individual clinical decision.
§§§
In July 2020, ACIP revised recommendations for HepA vaccination to include catch-up vaccination for children and adolescents aged 2–18 years who have not
previously received HepA vaccine at any age. https://www.cdc.gov/mmwr/volumes/69/rr/rr6905a1.htm?s_cid
¶¶¶
By parent or guardian report or provider records.
Discussion
NIS-Teen 2020 data indicate that although ≥1 dose HPV
coverage and HPV UTD status continue to increase, they
remain lower than coverage with most other routinely recom-
mended vaccines. Improvements in HPV vaccination coverage
are crucial to lowering rates of HPV-attributable cancers in the
United States. Coverage with ≥1 dose of Tdap and MenACWY
vaccines remains high and stable, while coverage with ≥2 doses
of MenACWY remains low, indicating the need for increased
awareness of the importance of the booster dose.

Morbidity and Mortality Weekly Report
1188 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. Estimated vaccination coverage with selected vaccines and doses among adolescents aged 13–17* years, by metropolitan statistical
area
†
and by poverty level — National Immunization Survey–Teen, United States, 2020
Vaccine
MSA, % (95% CI)
§
Below poverty level, % (95% CI)
§
At or above poverty level, % (95% CI)
§
Non-MSA
MSA
nonprincipal
city
MSA
principal
city Non-MSA
MSA
nonprincipal
city
MSA
principal
city Non-MSA
MSA
nonprincipal
city
MSA
principal
city
(n = 3,678) (n = 8,409) (n = 8,076) (n = 631) (n = 865) (n = 1,352) (n = 2,938) (n = 7,246) (n = 6,420)
Tdap
¶
≥1 dose 90.7
(88.7–92.3)
90.6
(89.3–91.8)
89.3
(87.7–90.7)
93.1
(89.7–95.5)
89.0
(84.7–92.1)
89.6
(86.3–92.2)
89.8
(87.4–91.9)
91.1
(89.7–92.3)
89.2
(87.3–90.9)
MenACWY**
≥1 dose 85.7
(83.7–87.5)
††
89.4
(87.9–90.7)
90.2
(88.7–91.5)
86.1
(81.8–89.5)
††
87.2
(82.6–90.6)
91.6
(88.8–93.7)
85.6
(83.2–87.7)
††
90.2
(88.6–91.5)
89.4
(87.5–91.0)
≥2 doses
§§
50.1
(43.4–56.9)
58.5
(54.0–62.8)
††
50.6
(45.2–56.1)
47.4
(33.5–61.7)
47.6
(33.0–62.7)
48.6
(35.8–61.7)
50.2
(42.3–58.0)
61.2
(56.6–65.6)
††
50.2
(44.1–56.4)
HPV
¶¶
vaccine
All adolescents
≥1 dose 68.0
(65.3–70.6)
††
74.2
(72.5–75.9)
††
77.8
(75.8–79.6)
73.6
(67.8–78.7)
††
83.6
(79.5–87.0)
85.7
(82.0–88.7)
64.9
(61.7–67.9)
††
73.1
(71.3–74.9)
††
76.2
(74.0–78.3)
HPV UTD
***
49.2
(46.3–52.1)
††
59.1
(57.2–61.0)
60.4
(58.2–62.6)
56.7
(50.3–62.9)
63.8
(58.1–69.2)
64.4
(59.2–69.3)
46.0
(42.9–49.3)
††
58.4
(56.4–60.4)
59.8
(57.4–62.2)
Females
≥1 dose
67.8
(63.7–71.7)
††
76.7
(74.5–78.8)
79.8
(76.9–82.4)
75.2
(66.4–82.2)
††
84.4
(78.9–88.6)
87.2
(82.0–91.0)
63.6
(58.6–68.2)
††
75.7
(73.3–78.0)
78.8
(75.7–81.7)
HPV UTD 50.3
(46.0–54.6)
††
62.2
(59.6–64.7)
63.2
(59.9–66.4)
56.9
(47.6–65.8)
65.3
(56.8–72.9)
66.0
(58.2–73.0)
46.8
(42.0–51.6)
††
61.9
(59.1–64.5)
63.5
(60.0–67.0)
Males
≥1 dose 68.1
(64.6–71.5)
††
71.9
(69.3–74.4)
††
75.8
(73.2–78.3)
71.6
(63.7–78.4)
††
82.9
(76.5–87.8)
84.3
(78.8–88.6)
66.1
(61.9–70.0)
††
70.7
(68.0–73.3)
73.7
(70.5–76.6)
HPV UTD 48.1
(44.3–52.0)
††
56.2
(53.4–58.9)
57.8
(54.8–60.7)
56.4
(47.8–64.7)
62.5
(54.5–69.8)
62.9
(55.8–69.4)
45.4
(41.2–49.7)
††
55.2
(52.2–58.1)
56.2
(52.8–59.5)
MMR ≥2 doses
92.8
(91.0–94.2)
92.4
(91.2–93.5)
92.3
(90.9–93.5)
93.6
(89.4–96.2)
89.5
(83.8–93.3)
90.8
(86.2–94.0)
92.3
(90.2–94.0)
92.9
(91.6–93.9)
92.4
(90.9–93.6)
Hepatitis A
vaccine
≥2 doses
†††
76.2
(73.7–78.5)
††
82.0
(80.6–83.4)
83.6
(81.9–85.2)
80.4
(75.0–84.9)
82.1
(77.1–86.3)
83.0
(78.1–87.0)
74.4
(71.5–77.0)
††
81.8
(80.2–83.3)
83.6
(81.7–85.3)
Hepatitis B
vaccine
≥3 doses
92.4
(90.6–93.9)
92.9
(91.7–93.9)
92.3
(90.9–93.5)
92.8
(89.0–95.4)
91.0
(86.3–94.2)
89.9
(85.5–93.2)
92.0
(89.8–93.8)
93.1
(91.9–94.1)
92.9
(91.5–94.1)
See table footnotes on the next page.
Disparities in vaccination coverage by MSA and poverty level
persist. Among adolescents living at or above the poverty level,
those in non-MSAs had lower HPV UTD status and coverage
with ≥2 doses of HepA than adolescents in MSA principal cit-
ies. Further investigation is needed to understand this disparity
and more generally, the relationship between socioeconomic
level, geographic location, barriers to vaccination such as vacci-
nation access, and vaccine confidence. Persons living below the
§§§§
Children aged ≤18 years who are Medicaid-eligible, uninsured, or American
Indian or Alaska Native (as defined by the Indian Health Care Improvement
Act) are eligible to receive vaccines from providers through the Vaccines
for Children (VFC) program. Children categorized as “underinsured”
because their health plans do not include coverage for recommended
vaccinations are eligible to receive VFC vaccines if they are served by a rural
health clinic or federally qualified health center or under an approved
deputization agreement. https://www.cdc.gov/vaccines/programs/vfc/
providers/eligibility.html
poverty level might have better access to the VFC program,
§§§§
which provides vaccines to children whose parents or guard-
ians otherwise might not be able to afford them. Adolescents
living below the poverty level have previously been shown to
have higher HPV vaccine coverage (2–4).
Although HPV vaccination continues to increase in the
United States, and coverage for most other routine vaccinations
remains high and stable, the COVID-19 pandemic threatens
these achievements. An analysis of immunization information
systems data from 10 U.S. jurisdictions during March–May
2020 compared with the same period in 2018 and 2019 iden-
tified a substantial decrease in the number of vaccine doses
administered to children and adolescents in 2020. Increases
in doses administered were noted during June–September
2020 but did not appear sufficient to offset the decline during

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1189
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. (Continued) Estimated vaccination coverage with selected vaccines and doses among adolescents aged 13–17* years, by metropolitan
statistical area
†
and by poverty level — National Immunization Survey–Teen, United States, 2020
Vaccine
MSA, % (95% CI)
§
Below poverty level, % (95% CI)
§
At or above poverty level, % (95% CI)
§
Non-MSA
MSA
nonprincipal
city
MSA
principal
city Non-MSA
MSA
nonprincipal
city
MSA
principal
city Non-MSA
MSA
nonprincipal
city
MSA
principal
city
(n = 3,678) (n = 8,409) (n = 8,076) (n = 631) (n = 865) (n = 1,352) (n = 2,938) (n = 7,246) (n = 6,420)
Varicella
History of
varicella
§§§
10.1
(8.6–11.8)
8.2
(7.2–9.4)
8.0
(6.9–9.4)
9.8
(6.9–13.6)
13.3
(9.4–18.5)
9.3
(6.4–13.3)
10.3
(8.6–12.3)
††
7.2
(6.2–8.4)
7.8
(6.5–9.3)
No history of varicella disease
≥1 dose vaccine 96.1
(94.6–97.1)
95.8
(94.8–96.6)
95.3
(94.1–96.2)
95.9
(91.9–97.9)
96.9
(94.6–98.2)
94.0
(90.0–96.4)
96.1
(94.4–97.3)
95.5
(94.3–96.4)
95.5
(94.2–96.5)
≥2 doses vaccine 92.5
(90.7–94.0)
92.0
(90.6–93.2)
91.6
(90.1–92.9)
94.2
(90.1–96.6)
87.9
(81.2–92.4)
90.7
(85.7–94.0)
91.7
(89.4–93.5)
92.4
(91.0–93.5)
91.6
(90.0–93.0)
History of
varicella or
received
≥2 doses VAR
93.2
(91.6–94.6)
92.7
(91.4–93.8)
92.3
(90.9–93.5)
94.7
(91.0–97.0)
89.5
(83.6–93.4)
91.5
(87.0–94.6)
92.5
(90.5–94.1)
92.9
(91.6–94.0)
92.2
(90.7–93.5)
Abbreviations: CI=confidence interval; HPV=human papillomavirus; MenACWY=quadrivalent meningococcal conjugate vaccine; MMR=measles, mumps, and
rubella vaccine; MSA=metropolitan statistical area; NIS-Teen = National Immunization Survey–Teen; Tdap=tetanus toxoid, reduced diphtheria toxoid, and acellular
pertussis vaccine; UTD=up-to-date; VAR= varicella vaccine.
* Adolescents (20,163) in the 2020 NIS-Teen were born during January 2002–January 2008.
†
MSA status was determined based on household-reported county of residence and was grouped into three categories: MSA principal city, MSA nonprincipal city,
and non-MSA. MSA and principal city were as defined by the U.S. Census Bureau https://www.census.gov/programs-surveys/metro-micro.html). Non-MSA areas
include urban populations not located within an MSA as well as completely rural areas.
§
Estimates with 95% CI widths >20 might not be reliable.
¶
Includes percentages receiving Tdap vaccine at age ≥10 years.
** Includes percentages receiving MenACWY and meningococcal-unknown type vaccine.
††
Statistically significant difference (p<0.05) in estimated vaccination coverage by metropolitan statistical area; referent group was adolescents living in MSA principal
city areas.
§§
≥2 doses of MenACWY or meningococcal-unknown type vaccine. Calculated only among adolescents who were aged 17 years at interview. Does not include
adolescents who received 1 dose of MenACWY vaccine at age ≥16 years.
¶¶
HPV vaccine, nine-valent (9vHPV), quadrivalent (4vHPV), or bivalent (2vHPV)in females and males combined.
*** HPV UTD includes those with ≥3 doses, and those with 2 doses when the first HPV vaccine dose was initiated before age 15 years and there was at least 5 months
minus 4 days between the first and second dose. This update to the HPV recommendation occurred in December 2016.
†††
In July 2020, ACIP revised recommendations for HepA vaccination to include catch-up vaccination for children and adolescents aged 2–18 years who have not
previously received HepA vaccine at any age. https://www.cdc.gov/mmwr/volumes/69/rr/rr6905a1.htm?s_cid
§§§
By parent or guardian report or provider records.
March–May 2020 (5). Analysis of adolescents in the 2019 and
2020 NIS-Teen data who were aged ≥13 years and had not
initiated HPV vaccination as of March 1 showed lower series
initiation initially from April through the end of October in
2020 compared with 2019; however, initiation of the HPV
series in 2019 and 2020 was similar by November–December.
Although this is encouraging, the NIS-Teen data cannot
yet be used to assess the potential impact of the pandemic
on adolescents who were due to receive vaccinations at age
11–12 years. As adolescents aged 11–12 years who were due
to receive routine vaccinations during the pandemic age into
the NIS-Teen survey sample (13–17 years), the full impact of
the COVID-19 pandemic can be assessed.
The findings in this report are subject to at least three
limitations. First, the household response rate was 20.7%,
and 45.2% of respondents had adequate provider data. Low
survey response rates can increase potential biases if survey
participants differ from nonrespondents (6). Second, bias in
estimates might remain after adjustment for household and
provider nonresponse and phoneless households. A recent
survey error assessment indicated that NIS-Teen estimates
might underestimate true coverage, with the largest under-
estimation for Tdap vaccine (−5.3 percentage points).
¶¶¶¶
Little evidence exists of a change in survey accuracy between
2019 and 2020.***** Finally, opportunity is limited to assess
the effect of the pandemic on routine coverage using 2020
¶¶¶¶
An assessment of validity of the 2019 NIS-Teen estimates has been reported
(https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-TEEN-
PUF19-DUG.pdf). NIS-Teen vaccination coverage estimates tended to be
slightly low compared with true values derived after adjusting for
noncoverage, nonresponse, and vaccination underascertainment, reaching
up to 5.3 percentage points too low for Tdap. This was primarily attributed
to underascertainment of vaccinations by the NIS provider record check.
The validity of estimates did not change from 2018 to 2019.
***** https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/pubs-
presentations/NIS-teen-vac-coverage-estimates-2020-tables.html#table-03

Morbidity and Mortality Weekly Report
1190 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
Summary
What is already known about this topic?
Tetanus, diphtheria, and acellular pertussis (Tdap), meningococ-
cal conjugate (MenACWY), and human papillomavirus (HPV)
vaccines are routinely recommended for adolescents.
What is added by this report?
In 2020, adolescent coverage with Tdap and the first dose of
MenACWY remained high and continued to improve for HPV
vaccines, with some disparities. Adolescents living outside a
metropolitan statistical area (MSA) had lower vaccination coverage
compared with adolescents living in MSA principal cities.
What are the implications for public health?
Results from the 2020 National Immunization Survey–Teen
reflect adolescent vaccination coverage before the COVID-19
pandemic. Efforts to reach adolescents whose routine medical
care has been affected by the pandemic are necessary to
protect adolescents and communities from vaccine-preventable
diseases and outbreaks.
NIS-Teen data; because many vaccines are recommended for
children aged 11–12 years, most adolescents aged 13–17 years
received their routine vaccinations before the pandemic started.
Health care providers should review patient vaccination
records and administer any vaccines or doses that are due.
Children and adolescents aged 12–17 years are also eligible
(those aged 16–17 years as of December 11, 2020 and those
aged 12–15 years as of May 10, 2021) for a COVID-19 vac-
cine, which may be administered with other vaccines at the
same visit (7). Ensuring that routine vaccination is maintained
and that adolescents catch up on any missed doses is essential to
protecting persons and communities from vaccine-preventable
diseases and outbreaks.
Corresponding author: Cassandra Pingali, [email protected]v.
1
Immunization Services Division, National Center for Immunization and
Respiratory Diseases, CDC;
2
Division of Viral Diseases, National Center for
Immunization and Respiratory Diseases, CDC;
3
Leidos Health, Atlanta,
Georgia;
4
Division of Bacterial Diseases, National Center for Immunization
and Respiratory Diseases, CDC.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. No potential conflicts of interest were disclosed.
References
1. Wodi AP, Ault K, Hunter P, McNally V, Szilagyi PG, Bernstein H. Advisory
Committee on Immunization Practices recommended immunization
schedule for children and adolescents aged 18 years or younger—United
States, 2021. MMWR Morb Mortal Wkly Rep 2021;70:189–92.
PMID:33571172 https://doi.org/10.15585/mmwr.mm7006a1
2. Henry KA, Swiecki-Sikora AL, Stroup AM, Warner EL, Kepka D. Area-
based socioeconomic factors and human papillomavirus (HPV) vaccination
among teen boys in the United States. BMC Public Health 2017;18:19.
PMID:28709420 https://doi.org/10.1186/s12889-017-4567-2
3. Swiecki-Sikora AL, Henry KA, Kepka D. HPV vaccination coverage
among US teens across the rural-urban continuum. J Rural Health
2019;35:506–17. PMID:30703854 https://doi.org/10.1111/jrh.12353
4. Elam-Evans LD, Yankey D, Singleton JA, et al. National, regional, state,
and selected local area vaccination coverage among adolescents aged
13–17 years—United States, 2019. MMWR Morb Mortal Wkly Rep
2020;69:1109–16. PMID:32817598 https://doi.org/10.15585/mmwr.
mm6933a1
5. Murthy BP, Zell E, Kirtland K, et al. Impact of the COVID-19 pandemic
on administration of selected routine childhood and adolescent
vaccinations—10 U.S. jurisdictions, March–September 2020. MMWR
Morb Mortal Wkly Rep 2021;70:840–5. PMID:34111058 https://doi.
org/10.15585/mmwr.mm7023a2
6. Pew Research Center. What low response rates mean for
telephone surveys. Washington, DC: Pew Research Center;
2017. https://www.pewresearch.org/methods/2017/05/15/
what-low-response-rates-mean-for-telephone-surveys/
7. CDC. COVID-19 vaccines for children and teens. Atlanta, GA: US
Department of Health and Human Services, CDC; 2021. https://www.cdc.
gov/coronavirus/2019-ncov/vaccines/recommendations/adolescents.html

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1191
US Department of Health and Human Services/Centers for Disease Control and Prevention
Evaluation of Syndromic Surveillance Data for Studying Harmful
Algal Bloom-Associated Illnesses — United States, 2017–2019
Amy M. Lavery, PhD
1
; Lorraine C. Backer, PhD
1
; Virginia A. Roberts, MSPH
2
; Jourdan DeVies, MS
3
; Johnni Daniel, DHSc
1
Harmful algal and cyanobacterial blooms (harmful algal
blooms) are large colonies of algae or cyanobacteria that can
harm humans, animals, and the environment (1–3). The num-
ber of algal blooms has been increasing in the United States,
augmented by increasing water temperatures and nutrients in
water from industry and agricultural run-off (4,5). The extent
to which harmful algal bloom exposures cause human illness or
long-term health effects is unknown. As the number of blooms
increases annually, the likelihood of negative health outcomes
(e.g., respiratory or gastrointestinal illness) from exposure also
increases (4,5). To explore the utility of syndromic surveillance
data for studying health effects from harmful algal bloom expo-
sures, CDC queried emergency department (ED) visit data
from the National Syndromic Surveillance Program (NSSP)
for harmful algal bloom exposure–associated administrative
discharge diagnosis codes and chief complaint text terms
related to harmful algal bloom exposure (6). A total of 321
harmful algal bloom-associated ED visits were identified during
January 1, 2017–December 31, 2019. An increase in harm-
ful algal bloom–associated ED visits occurred during warmer
months (June–October), consistent with seasonal fluctuations
of blooms and recent publications (6,7). Although syndromic
surveillance data are helpful for understanding harmful algal
bloom–associated ED visits in the United States, exposures
were documented infrequently with discharge diagnosis codes;
67% of harmful algal bloom–associated ED visits were iden-
tified through querying chief complaint text. Improving the
documentation of harmful algal bloom exposures in medical
records would further benefit future health studies.
NSSP is a collaboration among CDC, state, and local
health departments, and academic and private sector partners
which captures data electronically from EDs throughout the
country. As of the end of the study period (December 2019),
the national database represented approximately 70% of all
ED visits in the United States. Data are queried by creating
Boolean search terms of diagnostic codes and chief complaint
text. Chief complaint text terms are also used to categorize
visits into many broad, medically similar syndromes using
prebuilt algorithms.
For the current analysis, a query was created that comprises
main terms from the chief complaint (e.g., red tide, algae)
along with discharge diagnostic codes associated with expo-
sure to harmful algal blooms (International Classification of
Diseases, Tenth Revision, Clinical Modification [ICD-CM-10])
codes and their corresponding Systematized Nomenclature
of Medicine [SNOMED]* Clinical Terms codes). The final
query was reviewed using the NSSP query development tool.
†
Records identified by this query are defined as harmful algal
bloom-associated ED visits. To exclude ED visits associated
with the ingestion of contaminated seafood, relevant keywords
such as “shellfish” or “ciguatera poisoning” and corresponding
ICD-CM-10 codes (e.g., ciguatera poisoning, ICD-CM-10
code T61.0), were omitted from the query. Basic demographic
information for patients with harmful algal bloom–associated
ED visits was summarized by frequency and percentage. The
number of identified harmful algal bloom–associated ED vis-
its during 2017–2019 was described by U.S. Department of
Health and Human Services region and visualized using a time
series graph. Because the number of facilities reporting to NSSP
has increased since 2017, regional and time series comparisons
were shown as a percentage of total ED visits within NSSP.
The frequencies with which various syndrome categories
§
were
recorded during the harmful algal bloom-associated ED visits
were examined. Variables were created to indicate whether an
ED visit was related to neurologic, gastrointestinal, respiratory,
or dermatologic conditions.
¶
This activity was reviewed by
* http://www.snomed.org/snomed-ct/why-snomed-ct
†
The NSSP Chief Complaint Query Validation data source contains chief
complaint and discharge diagnosis codes only; to help protect anonymity, it
does not include any demographic data. This data subset helps users to iteratively
develop queries with inclusion and exclusion terms to capture only the records
of interest. Some NSSP sites do not contribute data to this data source. The
final query included the following ICD-10-CM codes: T65.82, toxic effect
harmful algae and algae toxins; Z77.121, contact with and suspected exposure
to harmful algae and algae toxins; SNOMED codes: 137512, 240914003,
10076437, 10076441, 402161005, 702986006, and 81034007; and main
terms related to algae and red tide. International Classification of Diseases, Ninth
Edition (ICD-9) codes were not included because ICD-10-CM codes for HAB
exposure were implemented in October 2015 and were similar, but more
descriptive than the ICD-9 codes for HAB exposure. Other terms related to
HAB exposure, such as “cyanobacteria” and “hab,” did not identify additional
records and were not included in the final query. The final query did not include
ICD-10-CM codes for HAB exposures through seafood or shellfish poisonings.
§
An automated algorithm codes standard symptom categories and subcategories
based on text in the chief complaint.
¶
Neurologic conditions include altered mental status, such as dizziness,
drowsiness, and muscle weakness; gastrointestinal conditions such as abdominal
pain, diarrhea, gastrointestinal bleeding, loss of appetite, nausea, and vomiting;
respiratory conditions such as acute bronchitis, chest congestion, difficulty
breathing, sore throat, influenza-like illness, nasal congestion, otitis media,
shortness of breath, upper respiratory infection, wheezing; and dermatologic
conditions (e.g., rash).

Morbidity and Mortality Weekly Report
1192 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
CDC and was conducted consistent with applicable federal
law and CDC policy.**
A total of 321 harmful algal bloom–associated ED visits were
identified during January 1, 2017–December 31, 2019. Among
these visits, 106 (33%) were identified through ICD-CM-10
codes only; the addition of chief complaint text key terms to
the query identified an additional 215 visits. Harmful algal
bloom–associated ED visits increased in the summer months
(June–October) in all 3 years (Figure). A notable peak occurred
in October 2018, corresponding with a large-scale red tide
event in the Gulf of Mexico during August–November 2018;
of the 197 ED visits occurring during July-November 2018,
73% occurred in Region 4 (southeastern United States).
Harmful algal bloom–associated ED visits occurred primar-
ily among patients aged 18–44 years (37%) and 45–64 years
** 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d);
5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
(30%) (Table 1); the majority (59%) occurred among females.
The largest number of harmful algal bloom–associated ED
visits was identified in Region 4 (31.1%). The most frequent
syndrome category was respiratory (41%), followed by gastro-
intestinal (14%), neurologic (10%), and dermatologic (8%)
(Table 2).
Discussion
This analysis identified approximately 300 harmful algal
bloom–associated ED visits during 2017–2019. ED visits
increased during the warmer months, consistent with seasonal
patterns of harmful algal blooms in the environment, with a
notable peak in 2018. Syndrome categories recorded for ED
visits were consistent with harmful algal bloom exposures
through inhalation (e.g., respiratory and neurologic), ingestion
(e.g., gastrointestinal), or skin contact (e.g., dermatologic) (5).
Most ED visits were identified through the chief complaint
text rather than through the use of ICD-10-CM codes. These
FIGURE. Harmful algal bloom exposure–associated emergency department visits among all emergency department visits, by month — National
Syndromic Surveillance Program, United States, 2017–2019*
0.0000
0.0001
0.0002
0.0003
0.0004
0.0005
0.0006
0.0007
0.0008
0.0009
100.0000
Jan Mar May Jul Sep Nov Jan Mar May Jul Sep Nov Jan Mar May Jul Sep Nov
2017 2018 2019
Percentage of ED visits due to harmful algal blooms
Year
This spike corresponds with
a large-scale red tide event
in the Gulf of Mexico during
August–November 2018.
* Percentage of all emergency department visits in the National Syndromic Surveillance Program was utilized to account for the increasing number of facilities
contributing data to the National Syndromic Surveillance Program.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1193
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Demographic characteristics of patients with harmful algal
bloom-associated emergency department visits (n = 321) — National
Syndromic Surveillance Program, United States, 2017–2019
Characteristic No. (%)
Age group (yrs)
0–4 19 (5.9)
5–17 35 (10.9)
18–44 118 (36.8)
45–64 96 (29.9)
≥65 50 (15.6)
Unknown 3 (0.9)
Sex
Female 190 (59.2)
Male 131 (40.8)
HHS Region*
,†
1 13 (9.7)
2 13 (4.9)
3 11 (4.1)
4 213 (31.1)
5 29 (6.6)
6 8 (4.1)
7 5 (5.3)
8 7 (12.9)
9 11 (7.6)
10 11 (13.7)
Abbreviation: HHS=U.S. Department of Health and Human Services.
* https://www.hhs.gov/about/agencies/iea/regional-offices/index.html
†
Percentages for HHS regions are adjusted for the total number of emergency
department visits during the time periods to account for the increasing number
of facilities reporting to NSSP since 2017.
results corroborate an earlier analysis using a commercial claims
data set, which identified few records with harmful algal bloom
exposure ICD-10-CM codes (8). Searching the chief complaint
text in NSSP more than doubled the number of harmful algal
bloom–associated visits, compared with the number that would
have been identified by searching on ICD-10-CM codes only.
The peak in ED visits during 2018 occurred primarily within
Region 4, corresponding to a large-scale red tide event in the
Gulf of Mexico that persisted during June 2018–November
2018 (9). The occurrence of this peak at the time of a red tide
event might explain the higher frequency of chief complaints
associated with respiratory symptoms because red tide has
been linked to respiratory health outcomes (2,3). Presumably,
these types of large-scale events might cause providers to ask
patients about recent harmful algal bloom exposures or cause
patients to mention them.
The NSSP query development tool made it possible to review
a sample of the full chief complaint text without linking to
other visit data, which helped to protect patient anonymity.
Several chief complaints (six) used terms such as, “patient
denies red tide exposure.” The final query was adjusted to
exclude these records; however, this finding implies that provid-
ers might have been asking patients if they had been exposed to
red tide, or patients might have mentioned that they had not
been on the beach or exposed to red tide before their ED visit.
TABLE 2. Primary syndrome categories associated with harmful algal
bloom exposure used among 321 harmful algal bloom-associated
emergency department visits
Syndrome type No. (%)*
Respiratory
†
133 (41.4)
Gastrointestinal
§
44 (13.7)
Neurologic
¶
33 (10.3)
Dermatologic** 27 (8.4)
* Records could contain multiple syndromes. Percentages might not sum to
100% because of missing values or listings of other syndrome types that
were not included for this analysis.
†
Respiratory symptoms consist of acute bronchitis, chest congestion, cough,
difficulty breathing, sore throat, influenza-like illness, nasal congestion, otitis
media, shortness of breath, upper respiratory infection, or wheezing.
§
Gastrointestinal symptoms consist of abdominal pain, diarrhea,
gastrointestinal bleeding, loss of appetite, nausea, or vomiting.
¶
Neurologic symptoms consist of altered mental status, dizziness, drowsiness,
headache, or muscle weakness.
** Dermatologic symptoms consist only of rash.
Increasing awareness so that more patients know to mention
harmful algal bloom exposure and more physicians know to
ask about harmful algal blooms would enhance understanding
of harmful algal bloom–associated ED visits.
The findings in this report are subject to at least two limi-
tations. First, some records might have been misclassified or
miscoded. For example, the query development tool identified
some records with a chief complaint that seemed unrelated to
harmful algal bloom exposure (e.g., meningitis exposure or
vaginal problems) despite the use of the Z77.121 harmful algal
bloom exposure ICD-10-CM code. In addition, it is unknown
what occurred during the ED visit between when the chief
complaint was assigned at triage and when the final diagnosis
was determined. Some patients might have described a harm-
ful algal bloom exposure, but medical personnel might have
ruled it out as the primary reason for diagnosis. Second, NSSP
undercounts the number of harmful algal bloom–associated
ED visits that resulted from environmental exposures because
1) only 70% of ED visits nationally are included within the
data set, and 2) ICD-10-CM codes are from billing data and
codes for harmful algal bloom exposures might not be included
if they do not affect reimbursement. Despite these limitations,
however, these analyses provide information of how often
exposure to a harmful algal bloom is documented during ED
visits through diagnostic codes and chief complaints.
These findings provide information about how harmful
algal bloom exposure can be identified through syndromic
surveillance ED visit data and potentially used to identify
the extent of illness from harmful algal bloom exposure in
the United States. As the frequency and geographic extent
of harmful algal blooms increase, it is important for health
care providers to discuss and document harmful algal bloom
exposures and health effects during medical visits to ensure
proper patient treatment and help patients understand how

Morbidity and Mortality Weekly Report
1194 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
Summary
What is already known about this topic?
Harmful algal and cyanobacterial blooms are large colonies of
algae or cyanobacteria that can harm humans, animals, and
the environment.
What is added by this report?
National syndromic surveillance data identified 321 emergency
department visits related to harmful algal bloom exposure
during 2017–2019. Frequency of these visits was highest during
warmer months.
What are the implications for public health practice?
Syndromic surveillance data are useful for studying the extent
of harmful algal bloom–associated illness. Increasing awareness
so that more patients know to mention harmful algal bloom
exposures and more physicians know to ask about them could
improve documentation of health effects and enable further
use of health records for health studies.
to prevent exposure in the future. As access to information
from electronic medical records for research improves, better
documentation of harmful bloom exposures and illnesses can
help support a more accurate assessment of their acute public
health impact. With better documentation, electronic health
record systems with longitudinal data could potentially pro-
vide data for monitoring long-term health effects from these
exposures, the extent of which are largely unknown.
Acknowledgments
Kathleen Hartnett, Aaron Kite-Powell, Praveena Jayanthi, Division
of Health Informatics and Surveillance, Center for Surveillance,
Epidemiology, and Laboratory Services, CDC; Andrea Winquist,
Division of Environmental Health Science and Practice, National
Center for Environmental Health, CDC.
Corresponding author: Amy M. Lavery, alaver[email protected].
1
Division of Environmental Health Science and Practice, National Center for
Environmental Health, CDC;
2
Division of Foodborne, Waterborne, and
Environmental Diseases, National Center for Emerging and Zoonotic Infectious
Diseases, CDC;
3
Division of Health Informatics and Surveillance, Center for
Surveillance, Epidemiology, and Laboratory Services, Centers for Disease
Control and Prevention.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. No potential conflicts of interest were disclosed.
References
1. National Ocean Service. Harmful algal blooms. Silver Spring, MD: US
Department of Commerce, National Oceanic and Atmospheric
Administration, National Ocean Service; 2021. https://oceanservice.noaa.
gov/hazards/hab/
2. Backer LC, Fleming LE, Rowan A, et al. Recreational exposure to
aerosolized brevetoxins during Florida red tide events. Harmful Algae
2003;2:19–28. https://doi.org/10.1016/S1568-9883(03)00005-2
3. Kirkpatrick B, Fleming LE, Backer LC, et al. Environmental exposures
to Florida red tides: effects on emergency room respiratory diagnoses
admissions. Harmful Algae 2006;5:526–33. PMID:20357898 https://
doi.org/10.1016/j.hal.2005.09.004
4. Environmental Protection Agency. Causes of CyanoHABs. Washington,
DC: Environmental Protection Agency; 2021. https://www.epa.gov/
cyanohabs/causes-cyanohabs
5. CDC. Harmful algal bloom (HAB)-associated illness: causes and
ecosystem impacts. Atlanta, GA: US Department of Health and Human
Services, CDC; 2021. https://www.cdc.gov/habs/environment.html
6. CDC. National Syndromic Surveillance Program (NSSP): syndromic
data critical to COVID-19. Atlanta, GA: US Department of Health and
Human Services, CDC; 2021. https://www.cdc.gov/nssp/index.html
7. Roberts VA, Vigar M, Backer L, et al. Surveillance for harmful algal bloom
events and associated human and animal illnesses—one health harmful
algal bloom system, United States, 2016–2018. MMWR Morb Mortal
Wkly Rep 2020;69:1889–94. PMID:33332289 https://doi.org/10.15585/
mmwr.mm6950a2
8. Lavery AM, Backer LC, Daniel J. Evaluation of electronic health records
to monitor illness from harmful algal bloom exposure in the United States.
J Environ Health 2021;83.9:8-14. https://www.neha.org/sites/default/
files/jeh/JEH5.21-Feature-Evaluation-Electronic-Health-Records.pdf
9. National Ocean Service. Fall 2018 red tide event that affected Florida and
the Gulf Coast. Silver Spring, MD; US Department of Commerce, National
Oceanic and Atmospheric Administration, National Ocean Service; 2021.
https://oceanservice.noaa.gov/hazards/hab/florida-2018.html

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1195
US Department of Health and Human Services/Centers for Disease Control and Prevention
Multiple Variants of SARS-CoV-2 in a University Outbreak After Spring Break —
Chicago, Illinois, March–May 2021
Kate Doyle, MPH
1
; Richard A. Teran, PhD
1,2
; Jennita Reefhuis, PhD
3
; Janna L. Kerins, VMD
1
; Xueting Qiu, PhD
1
; Stefan J. Green, PhD
4
;
Hyeree Choi, MPH
1
; Sabrina A. Madni, MPH
3,5
; Nazia Kamal, PhD
6
; Emily Landon, MD
7
; Reynald Christopher Albert, MHA
1
; Massimo Pacilli, MPH
1
;
Laura E. Furtado, MS
4
; Mary K. Hayden, MD
4
; Kevin J. Kunstman
4
; Cindy Bethel
7
; Lauren Megger
7
; Marielle J. Fricchione, MD
1,
*; Isaac Ghinai, MBBS
1,2,
*
To prevent transmission of SARS-CoV-2, the virus that
causes COVID-19, colleges and universities have implemented
multiple strategies including testing, isolation, quarantine,
contact tracing, masking, and vaccination. In April 2021,
the Chicago Department of Public Health (CDPH) was
notified of a large cluster of students with COVID-19 at an
urban university after spring break. A total of 158 cases of
COVID-19 were diagnosed among undergraduate students
during March 15–May 3, 2021; the majority (114; 72.2%)
lived in on-campus dormitories. CDPH evaluated the role of
travel and social connections, as well as the potential impact
of SARS-CoV-2 variants, on transmission. Among 140
infected students who were interviewed, 89 (63.6%) reported
recent travel outside Chicago during spring break, and 57
(40.7%) reported indoor social exposures. At the time of the
outbreak, undergraduate-aged persons were largely ineligible
for vaccination in Chicago; only three of the students with
COVID-19 (1.9%) were fully vaccinated. Whole genome
sequencing (WGS) of 104 specimens revealed multiple distinct
SARS-CoV-2 lineages, suggesting several nearly simultaneous
introductions. Most specimens (66; 63.5%) were B.1.1.222, a
lineage not widely detected in Chicago before or after this out-
break. These results demonstrate the potential for COVID-19
outbreaks on university campuses after widespread student
travel during breaks, at the beginning of new school terms,
and when students participate in indoor social gatherings. To
prevent SARS-CoV-2 transmission, colleges and universities
should encourage COVID-19 vaccination; discourage unvacci-
nated students from travel, including during university breaks;
implement serial COVID-19 screening among unvaccinated
persons after university breaks; encourage masking; and imple-
ment universal serial testing for students based on community
transmission levels.
University Prevention Measures
In spring 2021, approximately 2,100 students were living
on the campus of an urban university in Chicago, Illinois. In
* These authors contributed equally to this report.
response to the COVID-19 pandemic, the university imple-
mented numerous prevention strategies.
†
Students living on-
and off-campus were required to report positive SARS-CoV-2
test results to the university. Students living in the dormitories
were required to receive testing for SARS-CoV-2 every week
(serial screening); testing was offered for free by the university.
§
During March 20–29, 2021, university activities, including
classes, paused for spring break, and the university recom-
mended that students avoid all travel during this period;
dormitories remained open. After the break, students who
lived on campus were advised to stay in their dormitories for
1 week, and all classes were held remotely.
¶
In addition to
regular serial screening, students who lived in dormitories were
required to receive testing for SARS-CoV-2 before resuming
in-person learning.
Investigation and Response
On April 7, 2021, the university notified CDPH of 37 stu-
dents with positive SARS-CoV-2 test results detected through
serial screening conducted during March 29–April 5, 2021.
In response to this cluster of COVID-19 cases, the university
implemented a stay-at-home order for students living on cam-
pus (requiring students to stay in their dormitories), held all
classes remotely, and prohibited gatherings. During the stay-
at-home order, the university modified the screening schedule
to require testing for students living on campus twice during
the first 10 days of the order. In consultation with CDPH,
after additional testing found few cases, the university lifted
the order after 14 days.
A case was defined as receipt of a positive SARS-CoV-2
test result by an undergraduate student living on or near the
†
For the 2020–21 academic year, dormitory capacities were reduced, bedrooms
were single-occupancy, and numerous changes to physical infrastructure were
made. All students were required to sign a health agreement and pledge to avoid
social gatherings. The university maintained separate housing space for students
with positive SARS-CoV-2 test results; these students were required to follow
isolation procedures.
§
Real-time reverse transcription–polymerase chain reaction testing was performed
on anterior nasal swab specimens collected by trained medical assistants.
¶
Students were permitted to leave their dormitories to take walks, buy food, or
pick up meals from the dining halls.

Morbidity and Mortality Weekly Report
1196 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
university campus during March 15–May 18, 2021.** For all
students with COVID-19, the university provided information
on residence (on-campus dormitory or off-campus), age, gen-
der, and positive specimen collection date. CDPH conducted
interviews to collect information on demographic characteris-
tics, clinical signs or symptoms, travel history, social activities,
attendance at social gatherings, and close contacts. Diagnostic
testing history and results were extracted from state surveillance
and vaccination records from immunization registry systems.
Available specimens were sequenced and assigned a lineage.
††
Similar sequences (differing by fewer than five nucleotides)
were assumed to represent a single viral introduction.
§§
To
** The investigation period began 2 weeks before the start of spring break and
ended 2 weeks after the last positive SARS-CoV-2 test result for an
undergraduate student. Any positive test result among undergraduate students
who lived on campus or in Chicago was evaluated for inclusion. Graduate
students and staff members with COVID-19 were not included in this
outbreak case definition. Assessment of cases among these populations
indicated very limited or no interaction with undergraduate students who
lived on or very near campus.
††
Available SARS-CoV-2 positive specimens were submitted to CDPH’s
Regional Innovative Public Health Laboratory for whole genome sequencing
using the Swift Amplicon SARS-CoV-2 Panel (Swift Biosciences) and deep
sequencing on an Illumina instrument. Viral lineages were assigned using the
Phylogenetic Assignment of Named Global Outbreak Lineages (PANGOLIN)
tool (version v3.0.2; Rambaut Laboratory). Nucleotide differences were
assessed with IQ-TREE.
§§
Among the specimens of B.1.1.222 lineage, the majority of sequences were
genetically similar (within two nucleotides). Although there is no standard
genomic definition of sequences linked by transmission, this level of similarity,
together with the lack of detection of similar contemporaneous specimens in
Chicago, is likely consistent with one viral introduction.
identify possible geographic sources of importations, outbreak
lineages were compared with all contemporaneous sequences
of the same lineage available on the Global Initiative on
Sharing All Influenza Data (GISAID) platform. Descriptive
and social network analyses were completed using R (ver-
sion 4.1.0; R Foundation) and MicrobeTrace (version 0.7.0;
CDC), respectively. This activity was reviewed by CDC and
was conducted consistent with applicable federal law and
CDC policy.
¶¶
A total of 158 COVID-19 cases were identified among
undergraduate students (Figure 1), including 76 (48.1%) in
women; the median age of students with COVID-19 was
19.4 years (interquartile range=18.9–20.3 years) (Table). A
total of 114 (72.2%) students with COVID-19 lived in dor-
mitories (Supplementary Table, https://stacks.cdc.gov/view/
cdc/109260); the rest lived off-campus but near the university.
Among the 158 students with COVID-19, 140 (88.6%)
were interviewed, among whom 127 (90.7%) reported at least
one COVID-19 symptom (Table). Two were evaluated in an
emergency department after diagnosis; no infected student was
hospitalized or died. One student with COVID-19 had a pre-
vious laboratory-confirmed diagnosis of COVID-19 >90 days
before the infection was identified during the investigation
period. Among all interviewed students with COVID-19, 93
(66.4%) were unvaccinated, and 43 (30.7%) were partially
vaccinated (i.e., received 1 dose of a 2-dose COVID-19 vaccine
¶¶
45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d);
5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
FIGURE 1. Date of onset* and viral lineage among undergraduate students with COVID-19 (n = 158) — Chicago, Illinois, March–April 2021
0
5
10
15
20
No. of COVID-19 cases
Date
B.1.1.222
B.1.1.7
Not sequenced
Other lineage
Spring break period
CDPH begins investigation
15 16 17 18 19 20 21 22
Mar Apr
23 24 25 26 27 28 29 30 31 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29
Post–spring break
stay-at-home
advisory
Stay-at-home order in place
Stay-at-home
order rescinded
Abbreviation: CDPH = Chicago Department of Public Health.
* Or date of specimen collection for asymptomatic and presymptomatic persons. One specimen was collected and tested in May, but the date of symptom onset for
the student was in April.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1197
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE. Characteristics of undergraduate students with COVID-19
(n = 158) — Chicago, Illinois, March–May 2021
Characteristic
(no. with available information) No. (%)
Demographics (158)
Female 76 (48.1)
Median age, yrs (IQR) 19.4 (18.9–20.2)
Residence (158)
Dormitory A 35 (22.2)
Dormitory B 32 (20.3)
Dormitory C 31 (19.6)
Dormitory D 7 (4.4)
Dormitory E 5 (3.2)
Dormitory F 4 (2.5)
Off-campus 44 (27.8)
Previous COVID-19 diagnosis
>90 days before test date*
1 (0.6)
Interviewed (140)
Symptomatic 127 (90.7)
Provided at least one contact name 88 (62.9)
Reported indoor social exposure 57 (40.7)
Reported party exposure 3 (2.1)
Reported travel 89 (63.6)
Vaccination (140)
Reported not vaccinated 93 (66.4)
Reported partially vaccinated 43 (30.7)
Reported fully vaccinated
†
3 (2.1)
Travel destinations (89)
Florida 20 (22.5)
California 11 (12.4)
New York 11 (12.4)
Colorado 5 (5.6)
Within Illinois 3 (3.4)
Other U.S. states 32 (36.0)
International 6 (6.7)
Purpose of travel (89)
Vacation away from home 43 (48.3)
Visiting home 23 (25.8)
Moving to campus 3 (3.4)
Unknown 20 (22.5)
Lineage (104)
B.1.1.222 66 (63.5)
B.1.1.7 22 (21.2)
P. 1 9 (8.7)
B.1.526 3 (2.9)
B.1.526.1 1 (1.0)
B.1.526.2 1 (1.0)
B.1.1 1 (1.0)
B.1.429 1 (1.0)
Abbreviation: IQR=interquartile range.
* Previous diagnosis of COVID-19 was laboratory-confirmed.
†
Vaccination information was collected by self-report and verified, when
possible, with the state immunization registry. The three persons who reported
full vaccination could not be verified because vaccinations were administered
out of state (two) and as part of a clinical trial (one).
series or completed a vaccine series <14 days before diagnosis).
Three (1.9%) students with COVID-19 reported being fully
vaccinated; two of these students experienced symptoms.
The majority (88; 62.9%) of students with COVID-19 pro-
vided the name of at least one other student with COVID-19
with whom they had had contact in the 2 weeks preceding
Summary
What is already known about this topic?
SARS-CoV-2 transmission on college and university campuses
can occur when unvaccinated students return to campus after
travel or attend social gatherings.
What is added by this report?
After spring break 2021, COVID-19 cases increased rapidly at a
Chicago university despite mitigation measures. Interviews
indicated that the majority of cases occurred in unvaccinated
persons with a history of recent travel. Sequencing corrobo-
rated multiple introductions to campus and demonstrated that
even a single importation can result in many cases.
What are the implications for public health practice?
To mitigate SARS-CoV-2 transmission, colleges and universities
can encourage COVID-19 vaccination; discourage unvaccinated
students from traveling, including during university breaks;
implement serial screening after university breaks; test based
on community transmission; and encourage masking.
symptom onset or test date. Fifty-seven (40.7%) students
with COVID-19 described unmasked indoor exposures to
other students at small gatherings, meals, or while studying.
Although the university was aware of several large gatherings,
only three infected students (2.1%) reported having attended a
party. A network diagram was constructed to show social con-
nections, residence, travel, and viral lineage (Figure 2). Based
on interview data, 25 groups of socially connected students
with COVID-19 (clusters) were identified; the median cluster
size was two, and the maximum was 45. Several social groups
included multiple dormitories.
Overall, 89 (63.6%) interviewed students with COVID-19
reported travel outside Chicago during spring break. Fourteen
students traveled with at least one other infected student in five
different travel groups. Destinations included seven different
countries and 23 U.S. states; the most commonly visited states
were California, Colorado, Florida, and New York (Table).
The most commonly reported reason for travel was vacation
(43; 48.3%).
Residual specimens were available for 120 (75.9%)
infected students, 104 (86.7%) of which were successfully
sequenced. Sequences were assigned nine different lineages,
mostly B.1.1.222 (66; 63.5%), followed by B.1.1.7 (Alpha)
(22; 21.2%) (Table) (Supplementary Figure, https://stacks.cdc.
gov/view/cdc/109259). All B.1.1.222 sequences differed by
fewer than five nucleotides and likely represent a single source
introduction. When compared with sequences in GISAID, the
B.1.1.222 sequences in this outbreak were most closely related
to specimens from California. Eight of the 66 students (12.1%)
infected with the SARS-CoV-2 B.1.1.222 lineage had a his-
tory of travel to California. In Dormitory A, 25 of 35 (71.4%)

Morbidity and Mortality Weekly Report
1198 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 2. Social networks among undergraduate students with COVID-19 (n = 158), by residence and viral lineage — Chicago, Illinois,
March–May 2021
Dormitory A
O campus
Dormitory B
Dormitory C
Dormitory D
Dormitory E
Dormitory F
Reported travel Housing link
Social linkNo reported travel
Unknown travel
B.1.1.222
B.1.1.7
Not sequenced
Other lineage
specimens from infected students were sequenced, and 24 of 25
(96.0%) were confirmed as the B.1.1.222 lineage (Figure 2).
Among B.1.1.7 (Alpha) specimens, 10 groups of sequences dif-
fered by five or more nucleotides, indicating multiple separate
importations; groups ranged in size from one to five students.
B.1.1.7 was circulating widely in Chicago and elsewhere in the
United States at the time of this outbreak. Among the students
who traveled together, some travel groups had the same lineage
(though students reported additional close contact on campus),
while other groups included several lineages. Specimens from
all three fully vaccinated students were available; however, only
one (from a symptomatic student) was successfully sequenced
as a B.1.1.222 lineage.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1199
US Department of Health and Human Services/Centers for Disease Control and Prevention
Discussion
Previous reports have described outbreaks of COVID-19
among university students with complex social networks
and social exposures (1–5). In this outbreak, 158 cases of
COVID-19 were identified after many unvaccinated students
traveled during a university break, despite university policies
advising against travel. Subsequent on-campus gatherings led to
further transmission within and across social networks, includ-
ing between dormitories. Notably, this outbreak occurred
immediately before expansion of eligibility for vaccination in
Chicago; undergraduate-aged persons were largely ineligible
for vaccination before April 19, 2021.***
WGS identified several lineages and multiple distinct
introductions of SARS-CoV-2 that were possibly driven by
student travel. Phylogenetic analyses illustrated gaps in the
social network; for example, several students with no reported
social connections were infected with nearly identical strains
of B.1.1.222, a lineage not widely identified in Chicago before
or after this outbreak.
†††
Transmission likely occurred among
students without known social connections or through unde-
tected cases associated with the outbreak, although these links
cannot be confirmed with available case interview data.
The findings in this report are subject to at least four limita-
tions. First, some students with COVID-19 refused interviews,
omitted critical details, or provided false and conflicting infor-
mation, such as denying travel when other students indicated
that they had traveled together. This reticence limited the
ability to thoroughly assess social networks and transmission
chains. Second, serial screening was mandatory only for stu-
dents living on-campus; students living off-campus might have
had COVID-19 but did not receive testing during the outbreak
period. Given potentially undiagnosed infections, the magni-
tude of the outbreak might have been greater than described.
Third, not all SARS-CoV-2 specimens could be sequenced;
additional viral introductions or transmission chains might
have been missed. Finally, because publicly available sequence
data include only a subset of all viruses, the source of viral
introductions could not be definitively identified.
These findings support existing CDC recommendations for
the control of COVID-19 in colleges and universities; these
recommendations are especially important given the rapid
spread of the B.1.617.2 (Delta) variant of concern.
§§§
Serial
*** https://www.chicago.gov/city/en/sites/covid19-vaccine/home/vaccine-
distribution-phases.html
†††
Only one other B.1.1.222 sequence from a specimen collected in 2021 in
Chicago was available on GISAID (out of 674 Chicago sequences from 2021
not associated with this outbreak). This sequence, from a specimen collected
3 months before this outbreak, differed by more than five nucleotides from
the largely homogenous sequences observed in this outbreak.
§§§
https://www.cdc.gov/coronavirus/2019-ncov/community/colleges-
universities/considerations.html
testing successfully detected an outbreak among university
undergraduates; isolation of students with COVID-19, contact
tracing, and university-wide prevention measures contributed
to reductions in transmission. Nevertheless, unvaccinated
persons traveling during a university break and subsequent
socializing among students resulted in multiple clusters of
COVID-19 before vaccines were widely offered to undergradu-
ate-aged persons in Chicago. Vaccination is the leading preven-
tion strategy to protect persons from COVID-19, and colleges
and universities can benefit from encouraging vaccination for
all students, faculty, and staff members. In settings where not
everyone is fully vaccinated or where students have contact with
community members who are not fully vaccinated, colleges
and universities can encourage unvaccinated students to refrain
from travel; implement serial screening testing for unvaccinated
students, faculty, and staff members after university breaks; test
for SARS-CoV-2 based on community transmission levels;
encourage masking indoors; and make free, voluntary testing
readily available, including for fully vaccinated persons who
are experiencing COVID-19 symptoms.
¶¶¶
Acknowledgments
Francis Ambrosio, Mario Arias, Kelly Arndt, Carla Barrios, Fatima
Saifi, Chicago Department of Public Health case investigators;
university COVID response team; CDC MicrobeTrace team;
undergraduate students who participated in the investigation.
Corresponding author: Richard A. Teran, [email protected].
1
Chicago Department of Public Health, Chicago, Illinois;
2
Epidemic
Intelligence Service, CDC;
3
Division of Birth Defects and Infant Disorders,
National Center on Birth Defects and Developmental Disabilities, CDC;
4
Rush
University Medical Center, Chicago, Illinois;
5
4ES Corporation, San Antonio,
Texas;
6
Division of Preparedness and Emerging Infections, National Center
for Emerging and Zoonotic Infectious Diseases, CDC;
7
University of Chicago,
Chicago, Illinois.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. Mary K. Hayden reports participation on a clinical
adjudication panel for Sanofi related to investigational COVID-19
vaccines. No other potential conflicts of interest were disclosed.
References
1. Lewis M, Sanchez R, Auerbach S, et al. COVID-19 outbreak among
college students after a spring break trip to Mexico—Austin, Texas,
March 26–April 5, 2020. MMWR Morb Mortal Wkly Rep 2020;69:830–5.
PMID:32614814 https://doi.org/10.15585/mmwr.mm6926e1
2. Wilson E, Donovan CV, Campbell M, et al. Multiple COVID-19 clusters
on a university campus—North Carolina, August 2020. MMWR Morb
Mortal Wkly Rep 2020;69:1416–8. PMID:33001871 https://doi.
org/10.15585/mmwr.mm6939e3
¶¶¶
https://www.cdc.gov/coronavirus/2019-ncov/community/colleges-
universities/considerations.html#section3
Morbidity and Mortality Weekly Report
1200 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
3. Teran R, Ghinai I, Gretsch S, et al. COVID-19 outbreak among a
university’s men’s and women’s soccer teams—Chicago, Illinois, July–
August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1591–4. https://
doi.org/10.15585/mmwr.mm6943e5
4. Vang KE, Krow-Lucal ER, James AE, et al. Participation in fraternity and
sorority activities and the spread of COVID-19 among residential
university communities—Arkansas, August 21–September 5, 2020.
MMWR Morb Mortal Wkly Rep 2021;70:20–3. PMID:33411698
https://doi.org/10.15585/mmwr.mm7001a5
5. Fox MD, Bailey DC, Seamon MD, Miranda M. Response to a COVID-19
outbreak on a university campus—Indiana, August 2020. MMWR Morb
Mortal Wkly Rep 2021;70:118–22. PMID:33507894 https://doi.
org/10.15585/mmwr.mm7004a3

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1201
US Department of Health and Human Services/Centers for Disease Control and Prevention
Screening Programs for SARS-CoV-2 Infections on a University Campus —
Austin, Texas, September 30–November 30, 2020
Kayleigh J. Nerhood
1
; Emily R. James
1
; Allen Hardin, MS
2
; James E. Bray, MD
2
; Terrance S. Hines, MD
3
; Amy E. Young, MD
1
; Darlene Bhavnani, PhD
1
Colleges and universities in the United States have relied
on various measures during the COVID-19 pandemic to
prevent transmission of SARS-CoV-2, the virus that causes
COVID-19, including implementing testing programs (1–3).
These programs have permitted a safer return to campus for
students by identifying infected persons and temporarily isolat-
ing them from the campus population (2,3). The University
of Texas at Austin (UT Austin) implemented COVID-19
prevention measures in Fall 2020* including the following
testing programs: clinic-based diagnostic testing, voluntary
community screening, and targeted screening (testing of spe-
cific student populations in situations of increased transmission
risk). During September 30–November 30, 2020, UT Austin
students participated in tests for SARS-CoV-2, which resulted
in the detection of 401 unique student cases of COVID-19
from among 32,401 tests conducted.
†
Among students who
participated in one targeted screening program for students
attending campus events, 18 (37.5%) of 48 infected students
were asymptomatic at the time of their positive test result
compared with 45 (23%) of 195 students identified through
community testing and nine (5.8%) of 158 students identified
through clinic-based testing. Targeted screening also identified
a different population of students than did clinic-based and
community testing programs. Infected students tested through
targeted screening were more likely to be non-Hispanic White
persons (chi square=20.42; p<0.03), less likely to engage in
public health measures, and more likely to have had interac-
tions in settings where the risk for SARS-CoV-2 transmis-
sion is higher, such as restaurants, gyms, and residence halls.
In addition to clinic-based SARS-CoV-2 testing at colleges
and universities, complementary testing programs such as
community and targeted screening might enhance efforts to
identify and control SARS-CoV-2 transmission, especially
among asymptomatic persons and disproportionately affected
populations that might not otherwise be reached.
During September 30–November 30, 2020, UT Austin
employed the following SARS-CoV-2 testing programs:
1) clinic-based diagnostic testing administered by University
Health Services for persons who were symptomatic or reported
* https://protect.utexas.edu/
†
A COVID-19 case was defined as a positive SARS-CoV-2 nucleic acid
amplification test or antigen test result.
exposure to SARS-CoV-2 (clinic-based testing); 2) Proactive
Community Testing, which involved voluntary screening of
asymptomatic persons offered at several fixed or rotating sites
on-and-off campus (community testing); and 3) targeted
screening of specific student populations in situations of
increased transmission risk. One targeted screening program
focused on Big Ticket holders, students with season tickets to
athletic events. These events are large gatherings that might
involve several SARS-CoV-2 infection risk factors such as
several hours of possible exposure, the potential for crowding,
and behaviors such as singing and shouting.
§
Students were
tested up to 3 days before each event. Either a negative test
result or proof of previous SARS-CoV-2 infection 14–90 days
before the event was required for entry. Community testing and
targeted screening programs were provided to students at no
cost; clinic-based tests were billed to students’ insurance. Cases
were identified through clinic-based testing using SARS-CoV-2
nucleic acid amplification tests (NAATs), including reverse
transcription–polymerase chain reaction (RT-PCR) or isother-
mal NAAT (ID NOW [Abbott] or Aptima SARS-CoV-2 Assay
[Hologic]). Community testing used a Clinical Laboratory
Improvement Amendments (CLIA)-certified RT-PCR test
performed at a UT laboratory, and testing for Big Ticket
holders used an antigen test (Sofia SARS Antigen Fluorescent
Immunoassay [Quidel Corporation])
¶
or UT’s CLIA-certified
RT-PCR test. Test results were reported to Dell Medical School
at UT Austin, which was delegated by Austin Public Health to
conduct contact tracing. Contact tracers interviewed infected
persons to identify close contacts** during their infectious
period,
††
and collected exposure details, including dates,
proximity, location, duration of exposure, and mask use.
§
https://www.cdc.gov/coronavirus/2019-ncov/community/large-events/
considerations-for-events-gatherings.html
¶
https://www.fda.gov/media/137884/download
** Close contact was defined as being within 6 ft of a person with laboratory-
confirmed or probable COVID-19 infection for a cumulative total of ≥15 minutes
during a 24-hour period; or having physical contact with; or sharing living spaces
such as bedrooms, bathrooms, or kitchens. https://www.cdc.gov/coronavirus/2019-
ncov/php/contact-tracing/contact-tracing-plan/appendix.html
††
The infectious period was estimated to begin 2 days before symptom onset
and end ≥10 days after symptom onset or positive test result, as long as other
symptoms (except loss of taste or smell) were improving and the patient had
been fever-free for 24 hours without fever-reducing medication, according to
CDC guidance. https://www.cdc.gov/coronavirus/2019-ncov/php/contact-
tracing/contact-tracing-plan/investigating-covid-19-case.html

Morbidity and Mortality Weekly Report
1202 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
Characteristics, symptom status, isolation practices, and case
investigation outcomes among students with COVID-19 were
assessed; statistical comparisons among cases identified by the
different testing programs were performed using chi square
tests or one-way ANOVA in Python (version 3.7.9; Python
Software Foundation) using the SciPy statistical package (ver-
sion 1.5.4; Python Software Foundation); p values <0.05 were
considered statistically significant. This study was reviewed
by a UT Institutional Review Board and deemed to not be
human subjects research. This activity was reviewed by CDC
and conducted consistent with applicable federal law and
CDC policy.
§§
Among 32,401 tests of UT Austin students, 401 unique
COVID-19 cases were identified (Table 1); 3,044 tests were
§§
45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C.
Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
done through clinic-based testing, 25,042 through community
testing, and 4,314 through testing of Big Ticket holders.
Among one targeted screening program for Big Ticket holders,
75% of infected students self-identified as non-Hispanic
White persons, compared with 48.7% of infected students
detected by community testing and 58.9% of infected students
detected by clinic-based testing (chi square=20.42; p<0.03).
The proportion of non-Hispanic White students identified
by each of the three testing programs was higher than that
reported for the overall UT Austin student population
¶¶
(38.9%; chi square= 177; p<0.001). UT contact tracers
interviewed 85.5% of all infected persons. Among Big Ticket
holders, 75% of infected persons were interviewed, 20.8% were
unreachable by phone, and 4.2% stated they were unwilling to
¶¶
https://www.utexas.edu/about/facts-and-figures
TABLE 1. Demographic characteristics, symptom status, isolation practices, and case investigation outcomes among students with COVID-19,
by testing program — University of Texas at Austin, September 30–November 30, 2020
Characteristic
(no. with available information)
No. (%)
Total
Testing program
Big Ticket holder* Community Clinic-based
Students in testing programs 401 (100) 48 (12.0) 195 (48.6) 158 (39.4)
Age, yrs, median (range) 20 (18–29) 19.5 (18–22) 20 (18–28) 21 (18–29)
Sex (401)
Male 187 (46.6) 19 (39.6) 86 (44.1) 82 (51.9)
Female 213 (53.1) 29 (60.4) 108 (55.4) 76 (48.1)
Unknown 1 (0.2) 0 (—) 1 (0.5) 0 (—)
Race/Ethnicity (401)
White, non-Hispanic 224 (55.9) 36 (75.0) 95 (48.7) 93 (58.9)
Black, non-Hispanic 14 (3.5) 0 (—) 7 (3.6) 7 (4.4)
Asian, non-Hispanic 37 (9.2) 2 (4.2) 21 (10.8) 14 (8.9)
White, Hispanic 89 (22.2) 5 (10.4) 56 (28.7) 28 (17.7)
Multiracial 8 (2.0) 0 (—) 3 (1.5) 5 (3.2)
Unknown 29 (7.2) 5 (10.4) 13 (6.7) 11 (6.9)
Outcomes of COVID-19 case investigations (401)
Interviewed 343 (85.5) 36 (75.0) 171 (87.7) 136 (86.1)
Unable to interview 53 (13.2) 10 (20.8) 22 (11.3) 21 (13.3)
Unwilling to participate 5 (1.2) 2 (4.2) 2 (1.0) 1 (0.6)
Symptom status
Symptomatic 284 (70.8) 22 (45.8) 129 (66.2) 133 (84.2)
Asymptomatic 72 (18.0) 18 (37.5) 45 (23.1) 9 (5.7)
Unknown 45 (11.2) 8 (16.7) 21 (10.7) 16 (10.1)
Patient isolation (343)
†
Yes 317 (92.4) 29 (80.6) 156 (91.2) 132 (97.1)
No 23 (6.7) 5 (13.9) 14 (8.2) 4 (2.9)
Unknown 3 (0.9) 2 (5.6) 1 (0.6) 0 (—)
Specimen collection relative to symptom onset
§
(274)
Before symptom onset 28 (10.2) 3 (15.0) 18 (14.2) 7 (5.5)
On or after symptom onset 246 (89.8) 17 (85.0) 109 (85.8) 120 (94.5)
Start of isolation relative to symptom onset
§
(274)
Before symptom onset 42 (15.3) 0 (—) 15 (11.8) 27 (21.3)
On or after symptom onset 203 (74.1) 13 (65.0) 98 (77.2) 92 (72.4)
Unknown 29 (10.6) 7 (35.0) 14 (11.0) 8 (6.3)
* Screening targeted to students who held season tickets to athletic events.
†
Population limited to persons who were interviewed.
§
Population limited to persons who were interviewed and symptomatic.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1203
US Department of Health and Human Services/Centers for Disease Control and Prevention
participate in the interview, a larger proportion of refusals than
for community testing (1.0%) and clinic-based testing (0.6%).
Approximately 38% of cases among Big Ticket holders
occurred in persons who were asymptomatic at the time of their
positive test results, compared with 23% identified through
community testing and 6% through clinic-based testing
(chi square=35; p<0.001). Higher proportions of infected
students from the Big Ticket and community testing programs
were tested before symptom onset (15.0% and 14.2%, respec-
tively) compared with clinic-based testing (5.5%); however,
these differences were not statistically significant. Infected
persons detected through testing of Big Ticket holders were
less likely to have isolated after receiving a positive result (80%)
than were those identified through community (91.2%) and
clinic-based testing (97.1%).
Among 195 cases detected through community testing and
48 through testing of Big Ticket holders, 120 (61.5%) and
35 (72.9%) persons, respectively had no previous engagement
with community testing (Table 2). Among 40 asymptomatic
infected persons who had no previous community testing his-
tory, the testing program for Big Ticket holders identified a
higher proportion of asymptomatic cases than did community
testing (31.4% versus 24.2%; chi square=7.53; p = 0.02).
A similar average number of close contacts was reported by
infected persons identified from testing of Big Ticket holders
(2.6 per person), community testing (3.1), and clinic-based
testing (2.7) (p = 0.5). The most frequently reported exposure
location among all testing programs was household (44%),
defined as a shared living space (including a shared room or
suite in a residence hall) (Table 3). The second most common
exposure location identified through community and clinic-
based testing was private residence or apartment visits (24%
and 29%, respectively). In contrast, restaurants (22%) and
residence halls (16%) were the next most common exposure
locations among infected persons identified through testing
for Big Ticket holders. These persons also reported a higher
proportion of exposures in fitness or recreational facilities
(6%) than did persons identified through community testing
(3%) and clinic-based testing (1%), and a lower proportion
of exposures outdoors (2% versus 13% and 6%, respectively;
chi square=145; p<0.001). Across all programs, most expo-
sures were characterized by one or both students not wearing
TABLE 2. Symptom status* of student COVID-19 cases detected by community testing and testing for Big Ticket holders,
†
stratified by previous
history with community testing — University of Texas at Austin, September 30–November 30, 2020
Symptom status
No. (%)
Total
N = 243
History of community testing
No
n = 155
Yes
§
n = 88
Community
n = 120
Big Ticket holder
¶
n = 35
Community
n = 75
Big Ticket holder
n = 13
Asymptomatic 63 (25.9) 29 (24.2) 11 (31.4) 16 (21.3) 7 (53.8)
Symptomatic 151 (62.1) 76 (63.3) 17 (48.6) 53 (70.7) 5 (38.5)
Unknown 29 (11.9) 15 (12.5) 7 (20.0) 6 (8.0) 1 (7.7)
* Symptom status reported at time of case investigation.
†
Excluding cases detected by the University Health Services clinic-based testing.
§
Infected persons had at least one COVID-19 test via community testing at any time before their positive result and during the study period.
¶
Students who held season tickets to athletic events.
TABLE 3. Location of exposure* among persons with COVID-19
†
and their contacts, by testing program — University of Texas at Austin,
September 30–November 30, 2020
Location
Total
N = 1,147
Testing program, no. (%)
Big Ticket holder
§
n = 123
Community
n = 603
Clinic-based
n = 421
Household 502 (44) 42 (34) 250 (41) 210 (50)
Restaurant 74 (6) 27 (22) 34 (6) 13 (3)
Residence hall visit 53 (5) 20 (16) 25 (4) 8 (2)
Private residence visit 292 (25) 17 (14) 145 (24) 130 (31)
Fitness or recreational facility 32 (3) 7 (6) 20 (3) 5 (1)
Outdoor 105 (9) 2 (2) 77 (13) 26 (6)
Other 89 (8) 8 (7) 52 (9) 29 (7)
* If an infected person and a close contact interacted in multiple locations, contact tracers chose the most likely transmission site based on duration, proximity,
ventilation, and mask use.
†
Population limited to persons who were interviewed and named close contacts.
§
Students who held season tickets to athletic events.

Morbidity and Mortality Weekly Report
1204 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
a mask (91.4% of Big Ticket holders and 87.9% of those who
received community and clinic-based testing) (chi square=1.1;
p = 0.3). Contact tracers provided counseling to both infected
persons and close contacts on appropriate mask use to prevent
future exposures or reinfection.
Discussion
Clinic-based diagnostic testing is a valuable tool to detect
SARS-CoV-2 infection, particularly among symptomatic
persons; however, complementary testing programs might
enhance case detection (4). At UT Austin, one targeted screen-
ing program (conducted before vaccine availability) that tested
Big Ticket holders identified a significantly higher proportion
of asymptomatic persons than did clinic-based diagnostic test-
ing at University Health Services (as expected), and voluntary
screening through Proactive Community Testing. This targeted
testing program resulted in the identification of potential
asymptomatic spreaders, who might not have been detected
through clinic-based or community testing (5).
Targeted screening of Big Ticket holders identified a different
population from those identified by community and clinic-
based testing: students who were predominantly non-Hispanic
White and less likely to participate in voluntary public health
prevention strategies including community testing, early
isolation, and contact tracing. These Big Ticket holders also
had more exposures in restaurants, a documented risk factor
for SARS-CoV-2 infection (6), and in fitness or recreational
facilities, locations of several large outbreaks (7). They also
interacted more within residence halls, which include shared
facilities and social areas; risks for transmission in these set-
tings might be similar to those experienced in long-term care
facilities (1,8,9).
The findings of this study are subject to at least six limi-
tations. First, this study analyzed only one targeted testing
program among students aged 18–29 years. Assessment of
other targeted programs to include a broader age range might
alter these findings. Second, both antigen tests and NAATs
were used in testing of Big Ticket holders with different
turnaround times for results (<2 hours for antigen tests and
24–48 hours for NAATs), which might have affected infected
persons’ isolation timing and number of close contacts during
their infectious period. Differences in NAAT and antigen test
sensitivity might have also affected case ascertainment, with
antigen tests potentially missing contagious persons and NAAT
potentially detecting persons no longer infectious (10). Antigen
tests were not confirmed with NAATs, because rapid results
were required to exclude potentially infectious persons from
next-day events. Third, symptom status was self-reported and
recorded at the time of the interview; therefore, the number of
Summary
What is already known about this topic?
University testing programs have permitted a safer return of
students to campus by identifying persons with COVID-19 and
temporarily isolating them from the campus population.
What is added by this report?
Targeted screening identified 48 cases of COVID-19 during
September–November 2020, 18 (38%) of which were in
asymptomatic persons. This population of infected students
was demographically different from those identified through
other testing programs, more risk-tolerant, and less willing to
participate in public health prevention activities.
What are the implications for public health practice?
In addition to clinic-based diagnostic SARS-CoV-2 testing at
colleges and universities, a complementary strategy of commu-
nity and targeted screening programs might enhance efforts to
identify and control transmission of COVID-19.
asymptomatic cases could have been overestimated. However,
targeted screening would have still succeeded in identifying
presymptomatic cases. Fourth, symptoms caused by allergies,
stress, or other infectious diseases might have been incorrectly
attributed to COVID-19, inflating the number of symptomatic
cases, particularly among those from clinic-based testing. Fifth,
whether symptoms that started the day of the test began before
or after the test is not known, which might underestimate the
proportion of students who were tested before symptom onset.
Finally, the higher proportion of infected Big Ticket holders
who were unavailable or unwilling to participate in contact
tracing compared with the other testing program groups, might
have affected comparisons of symptom status, isolation, and
exposures to close contacts.
Screening tests are an important part of risk-reduction strate-
gies on college and university campuses and in other congregate
settings. Targeted testing in this university effort facilitated
reaching and identifying infected persons who might not
have been detected through other testing measures. Therefore,
targeted testing might be used as a complement to diagnostic
and voluntary community screening measures on college and
university campuses, particularly in high-risk or large gatherings
such as university athletic events or graduation ceremonies.
However, if antigen tests are used for asymptomatic screening,
confirmatory NAATs of positive results should be considered
if the likelihood of SARS-CoV-2 infection is low, such as if the
person has no known exposure (10). Further research on targeted
testing in other potential high-risk settings such as residence halls
is warranted, especially if a large proportion of these persons are
unvaccinated, or as variants of SARS-CoV-2 emerge.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1205
US Department of Health and Human Services/Centers for Disease Control and Prevention
Acknowledgments
Daniel Iken, Jessica Klima, Luke Klima, Jennifer Sarchet-Morgan,
Ta-Shina Williams, Carol Xia, contact tracing staff members and
volunteers, UT Health Austin and University Health Services,
University of Texas at Austin; Dell Medical School, University of
Texas at Austin and UT Health Austin leadership; staff members
of University Health Services, University of Texas at Austin; staff
members of University of Texas at Austin Athletics.
Corresponding author: Kayleigh Nerhood, [email protected].
1
Dell Medical School, University of Texas at Austin;
2
University of Texas at
Austin Athletics;
3
University Health Services, University of Texas at Austin.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of
potential conflicts of interest. Amy E. Young reports receipt of
honoraria from the American College of Obstetrics and Gynecology,
and travel support from the American Board of Obstetrics and
Gynecology. No other potential conflicts of interest were disclosed.
References
1. Wilson E, Donovan CV, Campbell M, et al. Multiple COVID-19 clusters
on a university campus—North Carolina, August 2020. MMWR Morb
Mortal Wkly Rep 2020;69:1416–8. PMID:33001871 https://doi.
org/10.15585/mmwr.mm6939e3
2. Fox MD, Bailey DC, Seamon MD, Miranda ML. Response to a
COVID-19 outbreak on a university campus—Indiana, August 2020.
MMWR Morb Mortal Wkly Rep 2021;70:118–22. PMID:33507894
https://doi.org/10.15585/mmwr.mm7004a3
3. Denny TN, Andrews L, Bonsignori M, et al. Implementation of a pooled
surveillance testing program for asymptomatic SARS-CoV-2 infections
on a college campus—Duke University, Durham, North Carolina,
August 2–October 11, 2020. MMWR Morb Mortal Wkly Rep
2020;69:1743–7. PMID:33211678 https://doi.org/10.15585/mmwr.
mm6946e1
4. Paltiel AD, Zheng A, Walensky RP. Assessment of SARS-CoV-2 screening
strategies to permit the safe reopening of college campuses in the United
States. JAMA Netw Open 2020;3:e2016818. PMID:32735339 https://
doi.org/10.1001/jamanetworkopen.2020.16818
5. Buitrago-Garcia D, Egli-Gany D, Counotte MJ, et al. Occurrence and
transmission potential of asymptomatic and presymptomatic
SARS-CoV-2 infections: a living systematic review and meta-analysis.
PLoS Med 2020;17:e1003346. PMID:32960881 https://doi.
org/10.1371/journal.pmed.1003346
6. Fisher KA, Tenforde MW, Feldstein LR, et al.; IVY Network Investigators;
CDC COVID-19 Response Team. Community and close contact
exposures associated with COVID-19 among symptomatic adults
≥18 years in 11 outpatient health care facilities—United States, July
2020. MMWR Morb Mortal Wkly Rep 2020;69:1258–64.
PMID:32915165 https://doi.org/10.15585/mmwr.mm6936a5
7. Lendacki FR, Teran RA, Gretsch S, Fricchione MJ, Kerins JL. COVID-19
outbreak among attendees of an exercise facility—Chicago, Illinois,
August–September 2020. MMWR Morb Mortal Wkly Rep
2021;70:321–5. PMID:33661859 https://doi.org/10.15585/mmwr.
mm7009e2
8. Lewis M, Sanchez R, Auerbach S, et al. COVID-19 outbreak among
college students after a spring break trip to Mexico—Austin, Texas,
March 26–April 5, 2020. MMWR Morb Mortal Wkly Rep
2020;69:830–5. PMID:32614814 https://doi.org/10.15585/mmwr.
mm6926e1
9. Kimball A, Hatfield KM, Arons M, et al.; Public Health – Seattle &
King County; CDC COVID-19 Investigation Team. Asymptomatic
and presymptomatic SARS-CoV-2 infections in residents of a long-term
care skilled nursing facility—King County, Washington, March 2020.
MMWR Morb Mortal Wkly Rep 2020;69:377–81. PMID:32240128
https://doi.org/10.15585/mmwr.mm6913e1
10. CDC. Interim guidance for antigen testing for SARS-CoV-2. Atlanta,
GA: US Department of Health and Human Services, CDC; 2020.
https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antigen-
tests-guidelines.html

Morbidity and Mortality Weekly Report
1206 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
COVID-19 Vaccination Coverage Among Adolescents Aged 12–17 Years —
United States, December 14, 2020–July 31, 2021
Bhavini Patel Murthy, MD
1,2
; Elizabeth Zell, MStat
1,2,3
; Ryan Saelee, MPH
1,2
; Neil Murthy, MD
1,2
; Lu Meng, PhD
2
; Seth Meador, MPH
1,2
;
Kirsten Reed, MPH
2
; Lauren Shaw, MS
1,2
; Lynn Gibbs-Scharf, MPH
1,2
; A.D. McNaghten, PhD
2
; Anita Patel, PharmD
2
; Shannon Stokley, DrPH
1,2
;
Stephen Flores, PhD
2
; Jonathan S. Yoder, MPH
2
; Carla L. Black, PhD
1,2
; LaTreace Q. Harris, MPH
1,2
On August 27, 2021, this report was posted as an MMWR Early
Release on the MMWR website (https://www.cdc.gov/mmwr).
Although severe COVID-19 illness and hospitalization are
more common among adults, these outcomes can occur in ado-
lescents (1). Nearly one third of adolescents aged 12–17 years
hospitalized with COVID-19 during March 2020–April 2021
required intensive care, and 5% of those hospitalized required
endotracheal intubation and mechanical ventilation (2). On
December 11, 2020, the Food and Drug Administration
(FDA) issued Emergency Use Authorization (EUA) of the
Pfizer-BioNTech COVID-19 vaccine for adolescents aged
16–17 years; on May 10, 2021, the EUA was expanded to
include adolescents aged 12–15 years; and on August 23,
2021, FDA granted approval of the vaccine for persons aged
≥16 years. To assess progress in adolescent COVID-19 vac-
cination in the United States, CDC assessed coverage with
≥1 dose* and completion of the 2-dose vaccination series
†
among adolescents aged 12–17 years using vaccine administra-
tion data for 49 U.S. states (all except Idaho) and the District
of Columbia (DC) during December 14, 2020–July 31,
2021. As of July 31, 2021, COVID-19 vaccination coverage
among U.S. adolescents aged 12–17 years was 42.4% for
≥1 dose and 31.9% for series completion. Vaccination coverage
with ≥1 dose varied by state (range=20.2% [Mississippi] to
70.1% [Vermont]) and for series completion (range=10.7%
* Receipt of ≥1 COVID-19 vaccine dose is defined as having received either ≥1
of the 2 Pfizer-BioNTech or Moderna vaccine doses, or a single dose of the
Janssen (Johnson & Johnson) vaccine. As of August 17, 2021, only the Pfizer-
BioNTech vaccine had been authorized for use among adolescents aged
12–17 years. Moderna and Janssen COVID-19 vaccines were not authorized
under emergency use for this age group during December 14, 2020–July 31,
2021. However, doses of these vaccines administered to persons aged 12–17 years
were included in this analysis. During February 27, 2021–July 31, 2021, a total
of 21,919 adolescents aged 12–17 years were reported to have received 1 dose
of the Janssen COVID-19 vaccine. During December 14, 2021–July 31, 2021,
a total of 27,226 adolescents aged 12–17 years were reported to have received
only the first dose of the Moderna COVID-19 vaccine; 66,032 adolescents
aged 12–17 years were reported to have received both doses of the Moderna
COVID-19 vaccine; 2,190 were reported to have received Pfizer-BioNTech for
the first dose but Moderna for the second dose; and 5,726 were reported to
receive Moderna for the first dose but Pfizer-BioNTech for the second dose.
†
Series completion was defined as receipt of either both doses of the Pfizer-
BioNTech or Moderna vaccines, including those that might have received
mismatched products between the first and second dose (i.e., Pfizer-BioNTech
for the first dose and Moderna for the second dose or vice versa) or a single
dose of the Janssen vaccine.
[Mississippi] to 60.3% [Vermont]). By age group, 36.0%,
40.9%, and 50.6% of adolescents aged 12–13, 14–15, and
16–17 years, respectively, received ≥1 dose; 25.4%, 30.5%, and
40.3%, respectively, completed the vaccine series. Improving
vaccination coverage and implementing COVID-19 preven-
tion strategies are crucial to reduce COVID-19–associated
morbidity and mortality among adolescents and to facilitate
safer reopening of schools for in-person learning.
Data on COVID-19 vaccine administration in the
United States are reported to CDC by jurisdictions, pharma-
cies, and federal entities through immunization information
systems (IISs),
§
the Vaccine Administration Management
System (VAMS),
¶
or direct data submission.** Adolescents
aged 12–17 years with valid residence in one of 49 states or
DC who received ≥1 dose of a COVID-19 vaccine during
December 14, 2020–July 31, 2021, and whose data were
reported to CDC by August 11, 2021, were included in this
analysis.
††
COVID-19 vaccine doses administered to persons
residing in Idaho were excluded because the state has data-
sharing restrictions on information reported to CDC.
Receipt of ≥1 COVID-19 vaccine dose and series completion
among adolescents aged 12–17 years was calculated overall
and stratified by age (12–13, 14–15, and 16–17 years), sex,
and jurisdiction (49 states and DC). As of August 17, 2021,
only the Pfizer-BioNTech vaccine had been authorized for
use among adolescents aged 12–17 years in the United States.
Moderna and Janssen (Johnson & Johnson) COVID-19 vac-
cines were not authorized under emergency use for this age
group during the analysis period; however, for reasons that are
§
IISs are confidential, computerized, population-based systems that collect and
consolidate vaccination data from providers in 64 public health jurisdictions
and can be used to track administered vaccines and measure vaccination
coverage. The 64 IIS jurisdictions comprise the 50 U.S. states, eight U.S.
territories and freely associated states (Puerto Rico, U.S. Virgin Islands,
American Samoa, Commonwealth of the Northern Mariana Islands, Guam,
Marshall Islands, Palau, and the Federated States of Micronesia), and six local
jurisdictions (Chicago, IL; Houston, TX; San Antonio, TX; Philadelphia, PA;
New York City, NY; and Washington, DC).
¶
https://www.cdc.gov/vaccines/covid-19/reporting/vams/program-information.html
** https://www.cdc.gov/vaccines/covid-19/reporting/overview/IT-systems.html
††
Providers are required to document vaccination in their medical records within
24 hours of administration and submit these data to their jurisdiction’s IIS
within 72 hours of administration.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1207
US Department of Health and Human Services/Centers for Disease Control and Prevention
not known, many adolescents were reported to have received
these vaccines, and doses administered to adolescents were
included in this analysis. Vaccination coverage by race and
ethnicity was not calculated because of high rates of missing
data. Population size by age group and sex was obtained from
the U.S. Census Bureau’s 2019 Population Estimates Program
(3). Second dose completion was calculated among adolescents
who received ≥1 dose of a 2-dose COVID-19 vaccination
series and for whom sufficient time to receive a second dose
during the analysis period had elapsed.
§§
Among adolescents
who received the first dose of a 2-dose COVID-19 vaccination
series, the proportions of adolescents who had already received
the second dose, of those who had not received the second
dose but were still within the recommended time interval to
receive the second dose, and of those who had not received
and were overdue for the second dose were calculated. Tests
for statistical significance were not conducted because these
data are reflective of the U.S. population (excluding Idaho)
and were not based on population samples. All analyses were
conducted using SAS software (version 9.4; SAS Institute). This
activity was reviewed by CDC and was conducted consistent
with applicable federal law and CDC policy.
¶¶
As of July 31, 2021, 42.4% of adolescents aged 12–17 years
had received ≥1 dose of a COVID-19 vaccine (Table 1),
and 31.9% had completed the vaccination series (Table 2).
Adolescent COVID-19 vaccination coverage with ≥1 dose varied
by state (range=20.2% [Mississippi] to 70.1% [Vermont]), as it
did for series completion (range=10.7% [Mississippi] to 60.3%
[Vermont]), with higher vaccination coverage in the Northeast
and on the West Coast and lower vaccination coverage in the
South (Figure). Coverage was higher among adolescents aged
16–17 years (50.6% for ≥1 dose; 40.3% for series completion)
than among those aged 12–13 years (36.0% for ≥1 dose; 25.4%
for series completion) and 14–15 years (40.9% for ≥1 dose;
30.5% for series completion). Vaccination coverage was similar
among males and females across all age groups.
Overall, 86.8% of adolescents aged 12–17 years who
received the first dose of a 2-dose COVID-19 vaccination
§§
Although the recommended interval between doses is 21 days for the Pfizer-
BioNTech vaccine, adolescents whose second doses were administered as early
as 17 days after the first dose or >21 days after the first dose were considered
to have completed the vaccination series. As of August 17, 2021, the Moderna
COVID-19 vaccine had not been authorized for use among adolescents.
However, the interval between the 2 Moderna COVID-19 vaccine doses was
assessed in the analysis. Although the recommended interval between doses
is 28 days for the Moderna vaccine, second doses received as early as 24 days
after the first dose or >28 days after the first dose were considered to complete
the vaccine series.
¶¶
45 C.F.R. part 46.102(l)(2); 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d);
5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
series*** received the second dose within the recommended
interval. A total of 2.4% had not received the second dose but
were within the allowable interval, and 10.8% were overdue
for the second dose (i.e., >42 days since receipt of the first
dose) (Supplementary Table, https://stacks.cdc.gov/view/
cdc/109000).
Discussion
Among all U.S. adolescents aged 12–17 years who received
the first dose of a 2-dose COVID-19 vaccine series, the vast
majority received the second dose, indicating high adherence
to completing the COVID-19 vaccine series. However, as of
July 31, 2021, only 42.4% of adolescents had received ≥1 dose
of a COVID-19 vaccine, and fewer than one third (31.9%) had
completed the vaccination series. Further, vaccination cover-
age varied widely by state, with those in the Northeast and on
the West Coast reporting the highest COVID-19 vaccination
coverage among adolescents. Vaccination coverage also varied
widely by age group, with reported coverage higher among
those aged 16–17 years compared with those aged 12–15 years.
This is likely because the older age group has been vaccine-
eligible for a longer period (i.e., since December 2020).
After the start of the COVID-19 pandemic, many schools
shifted to virtual or hybrid learning. Because in-person
learning fosters social and emotional development,
†††
safely
returning to schools for in-person learning remains a goal.
However, given the rapid emergence and spread of the highly
transmissible B.1.617.2 (Delta) variant of SARS-CoV-2, the
virus that causes COVID-19, and the increase in cases and
hospitalizations among children and adolescents (1), ensur-
ing high adolescent vaccination coverage is crucial to a safer
return to the classroom. Unvaccinated or undervaccinated
adolescents can become ill with COVID-19 and spread the
SARS-CoV-2 virus in schools, and by extension, in local com-
munities, placing other populations at risk. School systems can
consider implementing layered prevention strategies consistent
with CDC’s guidance for COVID-19 prevention in schools,
including universal indoor masking regardless of vaccination
status, improving ventilation, screening testing, physical dis-
tancing where feasible, and contact tracing in combination
with quarantine and isolation. As the 2021–22 school year
begins, concerted public health efforts are needed to increase
*** Among persons who received their first dose on or before July 6, 2021, for
Pfizer-BioNTech (i.e., >25 days between the first dose and July 31, 2021)
or June 29, 2021, for Moderna (i.e., >32 days between the first dose and
July 31, 2021). Percentages might not sum to 100% because persons who
were not yet due for the second dose were excluded from this analysis.
†††
https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/
k-12-guidance.html#anchor_1625661937509

Morbidity and Mortality Weekly Report
1208 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. Receipt of ≥1 COVID-19 vaccine dose by adolescents aged 12–17 years,* by age group and sex
†
— United States,
§
December 14, 2020–July 31, 2021
Jurisdiction
Age group and sex, no. (%)
12–17 yrs 12–13 yrs 14–15 yrs 16–17 yrs
Total Female Male Total Female Male Total Female Male Total Female Male
United States 10,677,934
(42.4)
5,425,265
(44.1)
5,216,450
(40.5)
3,094,245
(36.0)
1,543,152
(36.8)
1,541,710
(35.0)
3,454,771
(40.9)
1,750,329
(42.2)
1,693,216
(39.5)
4,128,918
(50.6)
2,131,784
(53.9)
1,981,524
(47.1)
Alabama 77,773
(20.6)
40,050
(22.4)
37,692
(19.0)
127,065
(17.5)
11,189
(18.7)
11,094
(16.5)
25,257
(19.6)
12,996
(20.3)
12,256
(18.9)
30,221
(24.8)
15,865
(28.7)
14,342
(21.6)
Alaska 23,706
(46.4)
11,621
(50.6)
11,788
(41.9)
14,859
(46.0)
3,279
(38.2)
3,480
(55.5)
7,627
(37.0)
3,755
(42.5)
3,789
(32.1)
9,241
(59.2)
4,587
(82.9)
4,519
(44.8)
Arizona 224,638
(38.9)
114,136
(40.9)
109,744
(36.8)
201,971
(32.3)
32,501
(32.7)
32,543
(31.7)
72,338
(37.3)
36,750
(38.9)
35,297
(35.5)
87,023
(48.1)
44,885
(52.7)
41,904
(43.7)
Arkansas 73,861
(30.3)
37,256
(31.6)
35,813
(28.6)
80,882
(25.0)
9,905
(24.7)
10,097
(24.8)
24,873
(31.2)
12,407
(30.4)
12,209
(31.5)
28,754
(34.7)
14,944
(40.3)
13,507
(29.5)
California 1,642,427
(53.2)
836,970
(55.5)
801,906
(50.8)
1,054,889
(44.3)
233,673
(45.3)
232,862
(43.2)
541,389
(52.3)
275,356
(54.7)
264,914
(49.9)
633,560
(63.6)
327,941
(67.2)
304,130
(59.8)
Colorado 222,780
(50.3)
113,015
(53.3)
109,520
(47.6)
147,908
(45.0)
33,118
(48.3)
33,343
(42.0)
73,879
(48.7)
37,316
(51.5)
36,481
(46.1)
82,383
(57.6)
42,581
(59.8)
39,696
(55.3)
Connecticut 166,941
(62.3)
84,333
(64.6)
82,242
(59.9)
87,364
(55.1)
23,935
(55.1)
24,047
(54.7)
53,242
(58.7)
27,015
(62.4)
26,116
(55.1)
65,592
(72.9)
33,383
(76.0)
32,079
(69.7)
Delaware 32,169
(45.2)
16,559
(49.0)
15,560
(41.6)
21,190
(44.0)
4,614
(50.5)
4,698
(39.0)
10,526
(37.8)
5,428
(34.9)
5,080
(41.2)
12,319
(55.7)
6,517
(71.3)
5,782
(44.6)
District of
Columbia
17,256
(52.3)
8,872
(53.3)
8,325
(50.9)
11,514
(49.8)
2,965
(56.6)
2,741
(43.7)
5,356
(46.0)
2,700
(38.3)
2,637
(57.5)
6,168
(62.6)
3,207
(73.4)
2,947
(53.7)
Florida 558,957
(37.6)
286,050
(39.4)
272,548
(35.9)
514,351
(31.0)
80,517
(32.9)
78,894
(29.3)
183,765
(37.2)
93,750
(37.6)
89,911
(36.8)
215,683
(45.3)
111,783
(48.4)
103,743
(42.3)
Georgia 271,600
(30.7)
138,608
(32.6)
132,222
(28.8)
307,972
(25.5)
39,194
(26.1)
39,086
(24.8)
87,107
(29.1)
44,308
(30.9)
42,597
(27.3)
105,965
(38.3)
55,106
(41.8)
50,539
(34.9)
Hawaii 60,457
(63.7)
30,251
(67.7)
30,035
(59.8)
33,044
(52.3)
8,501
(54.1)
8,725
(50.4)
19,774
(64.0)
9,869
(74.0)
9,857
(56.0)
23,409
(75.7)
11,881
(76.0)
11,453
(74.8)
Illinois 527,953
(53.2)
268,107
(54.1)
257,707
(52.0)
331,413
(45.4)
75,084
(44.8)
74,889
(45.7)
175,184
(52.1)
88,684
(52.1)
85,790
(51.7)
202,272
(62.4)
104,339
(65.9)
97,028
(58.5)
Indiana 164,717
(29.8)
84,039
(31.5)
79,638
(28.0)
194,055
(24.6)
23,834
(25.1)
23,786
(24.0)
52,778
(29.8)
26,775
(31.6)
25,704
(27.9)
64,144
(35.4)
33,430
(38.2)
30,148
(32.2)
Iowa 88,317
(36.7)
45,436
(38.6)
42,643
(34.8)
83,053
(31.8)
13,341
(32.8)
13,058
(30.8)
28,451
(36.9)
14,440
(36.2)
13,970
(37.5)
33,421
(41.6)
17,655
(47.3)
15,615
(36.4)
Kansas 88,601
(36.4)
45,509
(38.0)
42,995
(34.9)
84,150
(31.6)
13,211
(30.7)
13,352
(32.5)
27,907
(34.8)
14,328
(40.8)
13,557
(30.1)
34,100
(43.3)
17,970
(43.1)
16,086
(43.3)
Kentucky 115,204
(32.7)
59,363
(34.5)
55,723
(31.0)
122,071
(27.8)
17,009
(27.7)
16,927
(27.9)
37,571
(33.0)
19,163
(35.5)
18,375
(30.6)
43,680
(37.6)
23,191
(40.7)
20,421
(34.4)
Louisiana 81,272
(21.9)
41,478
(23.4)
39,560
(20.3)
131,531
(17.7)
11,736
(19.3)
11,536
(16.3)
26,369
(21.6)
13,273
(22.2)
13,019
(20.9)
31,616
(26.7)
16,469
(29.1)
15,005
(24.4)
Maine 48,729
(55.1)
24,474
(59.0)
23,874
(50.9)
27,699
(53.3)
7,247
(64.3)
7,370
(44.9)
16,031
(52.4)
8,004
(54.5)
7,858
(49.4)
17,937
(59.6)
9,223
(59.6)
8,646
(59.2)
Maryland 263,433
(56.3)
132,880
(57.8)
130,206
(54.7)
163,386
(49.1)
39,948
(51.2)
40,174
(47.1)
84,806
(53.6)
42,484
(52.7)
42,206
(54.4)
98,420
(67.4)
50,448
(70.9)
47,826
(63.8)
Massachusetts 319,741
(65.7)
161,726
(68.5)
157,494
(62.9)
158,110
(59.9)
47,185
(62.7)
47,336
(57.1)
105,067
(65.2)
53,176
(64.4)
51,711
(65.7)
120,042
(71.7)
61,365
(78.3)
58,447
(65.7)
Michigan 273,071
(36.0)
139,194
(38.1)
133,776
(34.1)
254,314
(30.6)
39,045
(31.8)
38,746
(29.5)
86,078
(34.7)
43,910
(36.8)
42,132
(32.7)
109,164
(42.7)
56,239
(45.5)
52,898
(40.0)
Minnesota 198,287
(44.3)
101,571
(45.8)
95,698
(42.4)
149,301
(40.8)
30,696
(39.3)
30,025
(42.1)
60,068
(38.7)
30,610
(40.9)
29,257
(36.4)
77,289
(54.1)
40,265
(58.4)
36,416
(49.3)
Mississippi 49,940
(20.2)
25,444
(21.0)
24,454
(19.3)
86,695
(16.7)
7,162
(17.7)
7,272
(15.7)
16,559
(21.4)
8,298
(20.3)
8,245
(22.7)
18,931
(22.6)
9,984
(25.0)
8,937
(20.4)
Missouri 152,486
(32.4)
77,515
(33.0)
74,807
(31.7)
158,781
(28.9)
22,844
(29.3)
23,025
(28.5)
49,384
(31.0)
25,006
(31.7)
24,325
(30.2)
57,185
(37.5)
29,665
(38.0)
27,457
(37.0)
Montana 23,962
(30.3)
12,105
(31.5)
11,683
(28.8)
25,348
(28.9)
3,579
(28.1)
3,669
(29.1)
7,428
(28.9)
3,730
(28.5)
3,638
(28.9)
9,209
(32.9)
4,796
(38.0)
4,376
(28.5)
Nebraska 62,131
(39.2)
31,723
(39.8)
30,292
(38.5)
56,881
(33.1)
9,447
(31.5)
9,343
(34.7)
19,599
(37.1)
9,928
(40.0)
9,649
(34.5)
23,719
(48.7)
12,348
(49.6)
11,300
(47.5)
Nevada 89,835
(37.2)
46,021
(37.7)
43,775
(36.6)
85,434
(29.8)
12,717
(30.8)
12,723
(28.8)
29,148
(36.3)
14,933
(34.9)
14,202
(37.8)
35,241
(46.5)
18,371
(48.4)
16,850
(44.6)
New Hampshire 48,188
(49.5)
24,264
(49.9)
23,250
(47.7)
34,943
(38.1)
6,575
(38.3)
6,609
(37.2)
15,129
(51.1)
7,567
(47.1)
7,332
(54.2)
19,747
(60.1)
10,122
(65.7)
9,309
(53.3)
New Jersey 357,267
(52.5)
180,504
(54.7)
175,521
(50.0)
232,003
(43.8)
50,304
(42.3)
51,137
(45.2)
113,832
(50.9)
57,509
(54.3)
55,960
(47.5)
141,702
(62.9)
72,691
(69.2)
68,424
(56.9)
New Mexico 92,891
(55.1)
46,824
(55.5)
44,864
(53.1)
57,115
(49.5)
13,992
(49.8)
13,800
(47.6)
29,505
(50.9)
14,745
(49.8)
14,367
(50.7)
35,137
(65.5)
18,087
(68.0)
16,697
(61.6)
New York 651,562
(46.6)
328,743
(48.5)
319,985
(44.5)
471,237
(39.3)
91,375
(39.4)
93,069
(38.9)
205,664
(44.3)
103,529
(46.5)
101,489
(42.0)
260,904
(56.6)
133,839
(60.1)
125,427
(52.6)
North Carolina 288,722
(35.4)
147,723
(35.7)
139,514
(34.8)
280,592
(29.4)
41,310
(28.5)
40,939
(30.1)
95,543
(35.3)
48,666
(35.0)
46,473
(35.3)
110,577
(42.0)
57,747
(44.3)
52,102
(39.1)
See table footnotes on the next page.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1209
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 1. (Continued) Receipt of ≥1 COVID-19 vaccine dose by adolescents aged 12–17 years,* by age group and sex
†
— United States,
§
December 14, 2020–July 31, 2021
Jurisdiction
Age group and sex, no. (%)
12–17 yrs 12–13 yrs 14–15 yrs 16–17 yrs
Total Female Male Total Female Male Total Female Male Total Female Male
North Dakota 13,910
(26.3)
7,084
(25.4)
6,613
(26.5)
18,993
(20.2)
1,888
(20.4)
1,894
(19.5)
4,533
(27.4)
2,290
(24.1)
2,175
(30.8)
5,535
(32.0)
2,906
(31.8)
2,544
(31.3)
Ohio 284,374
(31.9)
145,410
(33.8)
138,167
(29.9)
300,214
(27.1)
40,975
(28.2)
40,302
(26.0)
89,895
(29.9)
45,960
(31.6)
43,719
(28.2)
113,035
(38.8)
58,475
(42.1)
54,146
(35.5)
Oklahoma 92,409
(29.1)
47,313
(31.4)
44,973
(27.1)
113,915
(23.4)
13,242
(25.7)
13,346
(21.4)
29,283
(29.1)
15,020
(30.0)
14,228
(28.2)
36,505
(35.5)
19,051
(38.7)
17,399
(32.5)
Oregon 147,476
(49.3)
74,896
(49.7)
72,231
(48.8)
100,819
(43.5)
21,971
(44.0)
21,828
(42.9)
48,739
(48.1)
24,714
(47.6)
23,927
(48.3)
54,859
(56.8)
28,211
(57.6)
26,476
(55.5)
Pennsylvania 437,303
(47.7)
219,211
(48.7)
209,686
(44.8)
308,332
(41.3)
62,448
(41.8)
62,623
(39.4)
140,842
(45.2)
70,283
(46.6)
67,547
(42.1)
168,972
(56.7)
86,480
(57.7)
79,516
(53.7)
Rhode Island 42,660
(55.4)
21,683
(60.8)
20,919
(50.6)
25,863
(48.2)
6,167
(45.7)
6,290
(50.9)
13,645
(51.2)
7,024
(61.9)
6,595
(43.1)
16,544
(67.4)
8,492
(78.4)
8,034
(58.6)
South Carolina 100,830
(25.8)
51,820
(26.7)
48,946
(24.9)
135,830
(19.9)
13,591
(20.5)
13,384
(19.2)
33,001
(24.6)
17,005
(25.3)
15,977
(23.9)
40,842
(33.7)
21,224
(34.9)
19,585
(32.5)
South Dakota 24,848
(34.4)
12,468
(34.6)
11,989
(33.1)
24,483
(30.1)
3,612
(32.6)
3,661
(27.3)
8,051
(30.9)
4,073
(29.1)
3,850
(31.9)
9,439
(43.5)
4,783
(43.5)
4,478
(41.8)
Tennessee 126,159
(24.3)
65,267
(26.1)
60,591
(22.6)
185,246
(19.6)
18,164
(20.1)
18,156
(19.2)
40,295
(24.0)
20,848
(24.2)
19,407
(23.8)
49,495
(29.9)
26,255
(35.8)
23,028
(24.9)
Texas 1,028,789
(40.6)
521,461
(42.2)
506,643
(39.0)
854,580
(34.6)
147,957
(35.6)
147,505
(33.6)
330,444
(38.5)
167,302
(39.9)
162,971
(37.1)
402,745
(49.1)
206,202
(51.6)
196,167
(46.6)
Utah 129,559
(41.9)
65,495
(43.8)
63,818
(40.0)
106,783
(34.6)
18,393
(34.5)
18,549
(34.7)
39,977
(38.8)
20,029
(41.4)
19,925
(36.5)
52,615
(53.1)
27,073
(56.6)
25,344
(49.3)
Vermont 28,904
(70.1)
14,332
(74.4)
14,474
(65.9)
11,732
(75.0)
4,306
(83.5)
4,464
(67.9)
9,454
(70.3)
4,790
(91.7)
4,627
(56.3)
10,649
(66.3)
5,236
(58.9)
5,383
(75.1)
Virginia 342,958
(53.7)
173,904
(56.1)
168,793
(51.3)
222,929
(45.3)
50,509
(46.5)
50,461
(44.1)
113,259
(53.0)
57,040
(54.8)
56,153
(51.2)
128,655
(63.6)
66,355
(68.2)
62,179
(59.2)
Washington 296,782
(53.1)
149,501
(53.6)
145,592
(52.0)
192,800
(48.7)
46,631
(49.0)
46,691
(47.8)
95,740
(50.0)
47,895
(48.3)
47,255
(51.2)
107,187
(61.3)
54,975
(64.9)
51,646
(57.3)
West Virginia 38,159
(30.2)
19,127
(31.5)
18,459
(28.2)
44,298
(23.8)
5,126
(24.7)
5,263
(22.3)
12,061
(30.2)
6,090
(32.4)
5,782
(27.3)
15,564
(37.1)
7,911
(37.2)
7,414
(35.8)
Wisconsin 174,211
(39.9)
88,947
(41.5)
84,996
(38.2)
142,836
(35.8)
25,720
(38.3)
25,427
(33.6)
55,260
(36.8)
28,010
(37.0)
27,178
(36.4)
67,750
(47.1)
35,217
(49.2)
32,391
(44.9)
Wyoming 9,729
(20.4)
4,982
(21.7)
4,706
(19.0)
18,337
(15.8)
1,420
(16.5)
1,471
(15.2)
3,058
(20.9)
1,548
(19.9)
1,497
(21.8)
3,772
(25.7)
2,014
(30.8)
1,738
(21.4)
* Receipt of ≥1 COVID-19 vaccine dose is defined either as receiving at least one of the 2 doses of the Pfizer-BioNTech or Moderna vaccines or a single dose of the Janssen (Johnson & Johnson)
vaccine. As of August 17, 2021, only the Pfizer-BioNTech vaccine had been authorized for use among adolescents aged 12–17 years. Moderna and Janssen COVID-19 vaccines were not
authorized under emergency use for this age group during the analysis period; however, these vaccinations were included in this analysis.
†
Fewer than 0.5% of the records were missing information on sex.
§
COVID-19 vaccine doses administered to adolescents residing in Idaho were excluded because the state has data-sharing restrictions on information reported to CDC.
COVID-19 vaccination coverage among adolescents in addi-
tion to implementing COVID-19 prevention strategies based
on community transmission.
Public health practitioners can use various measures to
increase adolescent COVID-19 vaccination coverage. Building
on lessons from the public-private partnership between
CDC and retail pharmacies in the Federal Retail Pharmacy
Partnership
§§§
regarding vaccination clinics offered for selected
population groups at different times throughout the response
(4), local public health agencies and pharmacies could partner
with school districts and school systems to provide COVID-19
vaccinations to students at schools. Vaccine administration on
site at schools is an effective, evidence-based intervention that
improves childhood and adolescent vaccination rates for rou-
tinely recommended vaccines (5). State and local governments,
§§§
https://www.cdc.gov/vaccines/covid-19/retail-pharmacy-program/index.html
school administrators, community leaders, health care pro-
fessionals, and public health practitioners can facilitate safer
return to schools and improve equity among sociodemographic
groups by prioritizing COVID-19 vaccination among adoles-
cents and incorporating on-site school vaccinations for eligible
students (6,7). In addition, on-site vaccination clinics might
also be planned in coordination with other school-based vac-
cination programs, such as those for seasonal influenza and
routine adolescent vaccination.
Concerted outreach can help inform adolescents and their
parents about the importance of COVID-19 vaccination.
Effective outreach with tailored communication could help
improve vaccine confidence, acceptance, and coverage among
adolescents and their parents. In a recent report, only 56%
of parents of unvaccinated adolescents aged 12–17 years
expressed intent for their adolescent to receive a COVID-19
vaccine (8). Given that parental vaccination status is a marker

Morbidity and Mortality Weekly Report
1210 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. COVID-19 vaccination coverage among adolescents aged 12–17 years who completed the vaccine series,* by age group and sex
†
—
United States,
§
December 14, 2020–July 31, 2021
Jurisdiction
Age group and sex, no. (%)
12–17 yrs 12–13 yrs 14–15 yrs 16–17 yrs
Total Female Male Total Female Male Total Female Male Total Female Male
United States 8,045,685
(31.9)
4,117,404
(33.5)
3,905,344
(30.3)
2,183,597
(25.4)
1,093,057
(26.0)
1,085,039
(24.7)
2,570,498
(30.5)
1,311,724
(31.6)
1,251,765
(29.2)
3,291,590
(40.3)
1,712,623
(43.3)
1,568,540
(37.3)
Alabama 40,925
(10.8)
21,303
(11.9)
19,606
(9.9)
10,360
(8.2)
5,234
(8.7)
5,118
(7.6)
12,421
(9.6)
6,452
(10.1)
5,969
(9.2)
18,144
(14.9)
9,617
(17.4)
8,519
(12.8)
Alaska 18,394
(36.0)
9,066
(39.5)
9,148
(32.5)
4,947
(33.3)
2,384
(27.7)
2,522
(40.2)
5,678
(27.5)
2,778
(31.4)
2,847
(24.1)
7,769
(49.7)
3,904
(70.6)
3,779
(37.4)
Arizona 167,297
(29.0)
85,471
(30.6)
81,203
(27.3)
44,661
(22.1)
22,273
(22.4)
22,209
(21.7)
52,639
(27.1)
26,854
(28.4)
25,546
(25.7)
69,997
(38.7)
36,344
(42.6)
33,448
(34.9)
Arkansas 41,891
(17.2)
21,742
(18.4)
19,956
(15.9)
10,494
(13.0)
5,259
(13.1)
5,194
(12.7)
13,552
(17.0)
6,945
(17.0)
6,551
(16.9)
17,845
(21.5)
9,538
(25.7)
8,211
(17.9)
California 1,271,593
(41.2)
652,802
(43.3)
616,318
(39.0)
344,509
(32.7)
172,803
(33.5)
171,083
(31.7)
416,508
(40.3)
213,322
(42.4)
202,396
(38.1)
510,576
(51.2)
266,677
(54.6)
242,839
(47.7)
Colorado 185,447
(41.9)
94,420
(44.5)
90,901
(39.5)
52,056
(35.2)
25,885
(37.8)
26,150
(32.9)
61,301
(40.4)
31,074
(42.9)
30,191
(38.2)
72,090
(50.4)
37,461
(52.6)
34,560
(48.1)
Connecticut 136,730
(51.0)
69,481
(53.2)
66,983
(48.8)
36,973
(42.3)
18,513
(42.6)
18,368
(41.8)
43,625
(48.1)
22,287
(51.5)
21,253
(44.8)
56,132
(62.4)
28,681
(65.3)
27,362
(59.5)
Delaware 25,675
(36.1)
13,313
(39.4)
12,334
(33.0)
7,027
(33.2)
3,496
(38.2)
3,524
(29.3)
8,378
(30.1)
4,378
(28.2)
3,990
(32.3)
10,270
(46.4)
5,439
(59.5)
4,820
(37.2)
District of
Columbia
11,239
(34.1)
5,818
(34.9)
5,393
(33.0)
3,574
(31.0)
1,847
(35.2)
1,716
(27.4)
3,607
(31.0)
1,849
(26.2)
1,748
(38.1)
4,058
(41.2)
2,122
(48.6)
1,929
(35.1)
Florida 377,443
(25.4)
194,735
(26.8)
182,570
(24.0)
98,344
(19.1)
49,892
(20.4)
48,418
(18.0)
120,847
(24.5)
62,121
(24.9)
58,694
(24.0)
158,252
(33.2)
82,722
(35.8)
75,458
(30.7)
Georgia 166,329
(18.8)
85,830
(20.2)
80,219
(17.5)
41,215
(13.4)
20,691
(13.8)
20,437
(13.0)
48,426
(16.2)
24,922
(17.4)
23,455
(15.0)
76,688
(27.7)
40,217
(30.5)
36,327
(25.1)
Hawaii 35,203
(37.1)
17,549
(39.3)
17,546
(34.9)
9,931
(30.1)
4,831
(30.7)
5,072
(29.3)
11,450
(37.0)
5,705
(42.8)
5,715
(32.5)
13,822
(44.7)
7,013
(44.9)
6,759
(44.2)
Illinois 348,478
(35.1)
179,085
(36.1)
168,328
(33.9)
95,818
(28.9)
48,301
(28.8)
47,255
(28.8)
113,863
(33.9)
58,356
(34.3)
55,143
(33.2)
138,797
(42.8)
72,428
(45.8)
65,930
(39.7)
Indiana 131,406
(23.8)
67,329
(25.2)
63,257
(22.2)
35,025
(18.0)
17,450
(18.4)
17,450
(17.6)
41,394
(23.4)
21,124
(24.9)
20,030
(21.7)
54,987
(30.4)
28,755
(32.8)
25,777
(27.6)
Iowa 70,809
(29.4)
36,654
(31.1)
34,002
(27.7)
19,670
(23.7)
9,953
(24.5)
9,692
(22.8)
22,623
(29.3)
11,540
(28.9)
11,059
(29.7)
28,516
(35.5)
15,161
(40.6)
13,251
(30.9)
Kansas 61,300
(25.2)
31,698
(26.4)
29,559
(24.0)
16,594
(19.7)
8,240
(19.2)
8,339
(20.3)
18,868
(23.5)
9,778
(27.8)
9,082
(20.2)
25,838
(32.8)
13,680
(32.8)
12,138
(32.7)
Kentucky 81,664
(23.2)
42,709
(24.8)
38,895
(21.6)
22,107
(18.1)
11,199
(18.2)
10,903
(18.0)
26,034
(22.8)
13,521
(25.1)
12,500
(20.8)
33,523
(28.8)
17,989
(31.6)
15,492
(26.1)
Louisiana 46,411
(12.5)
24,126
(13.6)
22,181
(11.4)
11,607
(8.8)
5,905
(9.7)
5,695
(8.0)
13,932
(11.4)
7,128
(11.9)
6,772
(10.9)
20,872
(17.6)
11,093
(19.6)
9,714
(15.8)
Maine 42,857
(48.5)
21,496
(51.9)
21,044
(44.8)
12,259
(44.3)
5,993
(53.1)
6,149
(37.4)
14,157
(46.2)
7,069
(48.1)
6,953
(43.7)
16,441
(54.7)
8,434
(54.5)
7,942
(54.4)
Maryland 218,233
(46.7)
110,698
(48.2)
107,376
(45.1)
62,420
(38.2)
31,169
(39.9)
31,214
(36.6)
70,372
(44.5)
35,469
(44.0)
34,851
(44.9)
85,441
(58.5)
44,060
(61.9)
41,311
(55.1)
Massachusetts 263,919
(54.2)
134,332
(56.9)
129,099
(51.5)
74,471
(47.1)
37,267
(49.5)
37,081
(44.7)
86,063
(53.4)
43,839
(53.1)
42,066
(53.5)
103,385
(61.8)
53,226
(67.9)
49,952
(56.2)
Michigan 229,551
(30.3)
117,541
(32.1)
111,939
(28.5)
61,506
(24.2)
30,932
(25.2)
30,548
(23.3)
72,163
(29.1)
36,968
(31.0)
35,175
(27.3)
95,882
(37.5)
49,641
(40.2)
46,216
(34.9)
Minnesota 174,700
(39.0)
89,821
(40.5)
84,347
(37.4)
50,776
(34.0)
25,668
(32.9)
25,006
(35.1)
56,104
(36.1)
28,844
(38.5)
27,156
(33.8)
67,820
(47.4)
35,309
(51.2)
32,185
(43.5)
Mississippi 26,576
(10.7)
13,709
(11.3)
12,846
(10.2)
6,393
(7.4)
3,182
(7.9)
3,204
(6.9)
8,134
(10.5)
4,094
(10.0)
4,033
(11.1)
12,049
(14.4)
6,433
(16.1)
5,609
(12.8)
Missouri 104,029
(22.1)
53,410
(22.7)
50,568
(21.4)
28,825
(18.2)
14,385
(18.5)
14,432
(17.8)
32,843
(20.6)
16,854
(21.4)
15,979
(19.8)
42,361
(27.8)
22,171
(28.4)
20,157
(27.1)
Montana 18,046
(22.8)
9,197
(23.9)
8,794
(21.7)
5,167
(20.4)
2,551
(20.0)
2,598
(20.6)
5,430
(21.2)
2,784
(21.3)
2,626
(20.9)
7,449
(26.6)
3,862
(30.6)
3,570
(23.2)
Nebraska 48,472
(30.6)
25,035
(31.4)
23,394
(29.8)
13,509
(23.7)
6,854
(22.9)
6,647
(24.7)
15,152
(28.7)
7,759
(31.3)
7,384
(26.4)
19,811
(40.7)
10,422
(41.9)
9,363
(39.4)
Nevada 55,558
(23.0)
28,686
(23.5)
26,854
(22.5)
14,043
(16.4)
7,011
(17.0)
7,030
(15.9)
17,412
(21.7)
8,995
(21.0)
8,411
(22.4)
24,103
(31.8)
12,680
(33.4)
11,413
(30.2)
New Hampshire 39,480
(40.5)
19,952
(41.0)
18,996
(38.9)
10,267
(29.4)
5,083
(29.6)
5,094
(28.7)
12,290
(41.5)
6,173
(38.4)
5,945
(43.9)
16,923
(51.5)
8,696
(56.4)
7,957
(45.5)
New Jersey 289,682
(42.5)
146,961
(44.6)
141,715
(40.3)
77,253
(33.3)
38,290
(32.2)
38,734
(34.3)
92,001
(41.1)
46,666
(44.1)
45,052
(38.2)
120,428
(53.4)
62,005
(59.0)
57,929
(48.2)
New Mexico 72,669
(43.1)
37,085
(44.0)
35,178
(41.7)
20,417
(35.7)
10,265
(36.5)
10,012
(34.5)
22,917
(39.6)
11,613
(39.2)
11,184
(39.5)
29,335
(54.6)
15,207
(57.2)
13,982
(51.6)
New York 537,956
(38.5)
272,326
(40.2)
263,665
(36.6)
143,966
(30.6)
71,259
(30.7)
72,385
(30.2)
169,430
(36.5)
85,566
(38.4)
83,440
(34.5)
224,560
(48.7)
115,501
(51.9)
107,840
(45.2)
See table footnotes on the next page.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1211
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE 2. (Continued) COVID-19 vaccination coverage among adolescents aged 12–17 years who completed the vaccine series,* by age group
and sex
†
— United States,
§
December 14, 2020–July 31, 2021
Jurisdiction
Age group and sex, no. (%)
12–17 yrs 12–13 yrs 14–15 yrs 16–17 yrs
Total Female Male Total Female Male Total Female Male Total Female Male
North Carolina 210,162
(25.8)
108,311
(26.2)
100,839
(25.2)
55,824
(19.9)
28,001
(19.3)
27,612
(20.3)
68,736
(25.4)
35,229
(25.3)
33,228
(25.2)
85,602
(32.5)
45,081
(34.6)
39,999
(30.0)
North Dakota 10,254
(19.4)
5,257
(18.9)
4,842
(19.4)
2,516
(13.2)
1,259
(13.6)
1,219
(12.5)
3,234
(19.5)
1,628
(17.2)
1,556
(22.1)
4,504
(26.1)
2,370
(26.0)
2,067
(25.4)
Ohio 239,023
(26.8)
122,890
(28.6)
115,636
(25.0)
63,374
(21.1)
32,046
(22.0)
31,238
(20.2)
74,684
(24.8)
38,484
(26.4)
36,083
(23.3)
100,965
(34.7)
52,360
(37.7)
48,315
(31.7)
Oklahoma 61,250
(19.3)
31,546
(20.9)
29,633
(17.8)
15,691
(13.8)
7,764
(15.0)
7,913
(12.7)
18,709
(18.6)
9,633
(19.2)
9,056
(18.0)
26,850
(26.1)
14,149
(28.8)
12,664
(23.7)
Oregon 126,346
(42.3)
64,593
(42.8)
61,618
(41.6)
36,145
(35.9)
18,188
(36.4)
17,937
(35.3)
41,459
(40.9)
21,114
(40.7)
20,319
(41.0)
48,742
(50.4)
25,291
(51.7)
23,362
(49.0)
Pennsylvania 303,836
(33.1)
153,011
(34.0)
145,168
(31.0)
84,516
(27.4)
41,529
(27.8)
41,414
(26.0)
98,297
(31.6)
49,226
(32.6)
47,005
(29.3)
121,023
(40.6)
62,256
(41.5)
56,749
(38.3)
Rhode Island 35,520
(46.1)
18,100
(50.7)
17,380
(42.0)
9,733
(37.6)
4,786
(35.4)
4,938
(40.0)
11,386
(42.7)
5,862
(51.6)
5,508
(36.0)
14,401
(58.7)
7,452
(68.8)
6,934
(50.6)
South Carolina 72,130
(18.4)
37,476
(19.3)
34,621
(17.6)
17,802
(13.1)
8,967
(13.5)
8,831
(12.7)
22,947
(17.1)
11,939
(17.7)
10,996
(16.4)
31,381
(25.9)
16,570
(27.3)
14,794
(24.5)
South Dakota 16,383
(22.7)
8,318
(23.1)
7,813
(21.6)
4,264
(17.4)
2,113
(19.1)
2,108
(15.7)
5,037
(19.3)
2,585
(18.5)
2,374
(19.7)
7,082
(32.6)
3,620
(32.9)
3,331
(31.1)
Tennessee 87,019
(16.8)
45,491
(18.2)
41,307
(15.4)
22,260
(12.0)
11,200
(12.4)
11,035
(11.6)
26,342
(15.7)
13,724
(15.9)
12,597
(15.4)
38,417
(23.2)
20,567
(28.0)
17,675
(19.1)
Texas 718,918
(28.4)
369,600
(29.9)
348,945
(26.9)
193,523
(22.6)
97,354
(23.4)
96,096
(21.9)
225,520
(26.2)
115,724
(27.6)
109,695
(24.9)
299,875
(36.5)
156,522
(39.1)
143,154
(34.0)
Utah 96,759
(31.3)
49,212
(32.9)
47,466
(29.8)
25,119
(23.5)
12,578
(23.6)
12,530
(23.4)
29,095
(28.3)
14,641
(30.3)
14,449
(26.4)
42,545
(42.9)
21,993
(46.0)
20,487
(39.9)
Vermont 24,881
(60.3)
12,395
(64.3)
12,437
(56.6)
7,388
(63.0)
3,657
(70.9)
3,720
(56.6)
8,118
(60.4)
4,095
(78.4)
4,006
(48.8)
9,375
(58.4)
4,643
(52.2)
4,711
(65.7)
Virginia 283,385
(44.3)
144,360
(46.6)
138,878
(42.2)
79,268
(35.6)
39,685
(36.5)
39,546
(34.6)
93,389
(43.7)
47,282
(45.5)
46,077
(42.0)
110,728
(54.7)
57,393
(59.0)
53,255
(50.7)
Washington 245,243
(43.9)
124,122
(44.5)
119,901
(42.8)
73,427
(38.1)
36,514
(38.4)
36,573
(37.4)
79,630
(41.6)
40,075
(40.4)
39,149
(42.5)
92,186
(52.7)
47,533
(56.1)
44,179
(49.0)
West Virginia 27,203
(21.6)
13,567
(22.3)
13,174
(20.1)
6,953
(15.7)
3,372
(16.3)
3,453
(14.6)
8,505
(21.3)
4,299
(22.9)
4,066
(19.2)
11,745
(28.0)
5,896
(27.7)
5,655
(27.3)
Wisconsin 140,545
(32.2)
72,235
(33.7)
68,167
(30.6)
37,736
(26.4)
19,067
(28.4)
18,641
(24.6)
43,634
(29.0)
22,269
(29.4)
21,335
(28.6)
59,175
(41.2)
30,899
(43.1)
28,191
(39.1)
Wyoming 6,866
(14.4)
3,540
(15.4)
3,305
(13.4)
1,874
(10.2)
912
(10.6)
956
(9.8)
2,162
(14.8)
1,088
(14.0)
1,070
(15.6)
2,830
(19.3)
1,540
(23.6)
1,279
(15.7)
* Vaccine series completion was defined as receiving either both doses of the Pfizer-BioNTech or Moderna vaccines, including mismatched products between the first and second dose (i.e.,
Pfizer-BioNTech for the first dose and Moderna for the second dose or vice versa) or a single dose for the Janssen (Johnson & Johnson) vaccine. As of August 17, 2021, only the Pfizer-
BioNTech vaccine had been authorized for use among adolescents aged 12–17 years. Moderna and Janssen COVID-19 vaccines were not authorized under emergency use for this age
group during the analysis period; however, these vaccinations were included in this analysis.
†
Fewer than 0.5% of the records were missing information on sex.
§
COVID-19 vaccine doses administered to adolescents residing in Idaho were excluded because the state has data-sharing restrictions on information reported to CDC.
for adolescent vaccination status,
¶¶¶
vaccine hesitancy or anti-
vaccination sentiments among parents might directly lead to
missed opportunities to vaccinate adolescents (9). Among ado-
lescents and their parents who were surveyed about their intent
to receive a COVID-19 vaccine, many reported that having
more information about the safety and efficacy of COVID-19
vaccines would increase their likelihood of receiving a vaccine
(8). Public health practitioners can use multimodal outreach
efforts involving a variety of traditional and social media
platforms to engage adolescents and their parents to improve
vaccination acceptance and coverage. Further, state and local
governments can consider strategies that encourage receipt
by adolescents of all vaccines recommended by the Advisory
¶¶¶
https://www.kff.org/coronavirus-covid-19/poll-finding/
kff-covid-19-vaccine-monitor-parents-and-the-pandemic
Committee on Immunization Practices, especially given the
declines in routine childhood and adolescent vaccinations
during the pandemic (10).
The findings in this report are subject to at least five limita-
tions. First, vaccination coverage rates were aggregated and
analyzed only at the state level. Calculating coverage at more
specific levels (e.g., by county or urban-rural classification)
could potentially identify geographic areas with low vaccina-
tion coverage rates. Second, because Idaho was excluded from
the analysis, the findings are not representative of the entire
United States. Third, adolescents who received COVID-19
vaccines from different entities that used different methods
for submitting data (e.g., if the first dose was administered at
a pharmacy and the second dose was given at a mass vaccina-
tion site) might not have their first and second doses linked,

Morbidity and Mortality Weekly Report
1212 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE. Percentage of adolescents aged 12–17 years who
completed the COVID-19 vaccination series*
,†
— United States,
§
December 14, 2020–July 31, 2021
DC
>50.0
40.1–50.0
30.1–40.0
20.1–30.0
≤20.0
Not available
Abbreviation: DC = District of Columbia.
* As of August 17, 2021, only the Pfizer-BioNTech vaccine had been authorized
for use among adolescents aged 12–17 years. Moderna and Janssen (Johnson &
Johnson) COVID-19 vaccines were not authorized under emergency use for this
age group during the analysis period; however, many adolescents had
documentation of receipt of these vaccines. Thus, these vaccine doses were
included in this analysis if they were administered to adolescents aged 12–17 years.
†
Series completion was defined as receipt of either both doses of the Pfizer-
BioNTech or Moderna vaccines, including those who might have received
mismatched products between the first and second dose (i.e., Pfizer-BioNTech
for the first dose and Moderna for the second dose or vice versa) or a single dose
of the Janssen vaccine.
§
COVID-19 vaccine doses administered to adolescents residing in Idaho were
excluded because the state has data-sharing restrictions on information reported
to CDC.
which could have led to underestimation of the percentage of
adolescents who completed the vaccination series. Fourth, if
an adolescent had inadvertently received a different recipient
ID when receiving their second dose, first and second doses
could not be linked. Finally, vaccination coverage could not
be calculated on the basis of race and ethnicity because of
incomplete reporting.
An estimated 2 million COVID-19 cases and approximately
300 associated deaths have been reported among children aged
5–17 years since the start of the COVID-19 pandemic (1). As
persons in younger age groups become eligible for COVID-19
vaccination, public health practitioners, health care profession-
als, school administrators, and state and local governments can
use evidence-based practices to decrease barriers to vaccination
and increase confidence in COVID-19 vaccines, which can help
facilitate the safer return to in-person learning at schools and ulti-
mately reduce COVID-19–associated morbidity and mortality.
Summary
What is already known about this topic?
Although more common among adults, severe COVID-19 illness
and hospitalization occur among adolescents.
What is added by this report?
As of July 31, 2021, coverage with ≥1 dose of COVID-19 vaccine
among adolescents aged 12–17 years was 42%, and 32% had
completed the series. Series completion rates varied widely by
state, ranging from 11% to 60%, and was 25% for adolescents
aged 12–13 years, 30% for those aged 14–15 years, and 40% for
those aged 16–17 years.
What are the implications for public health practice?
Improving adolescent COVID-19 vaccination coverage is crucial
to reduce COVID-19–associated morbidity and mortality among
adolescents and can help facilitate safer reopening of schools
for in-person learning.
Acknowledgments
COVID-19 Vaccine Task Force; U.S. Department of Defense;
immunization program managers, immunization information system
managers, and other staff members of the immunization programs in
the 64 jurisdictions and five federal entities who provided these data.
Corresponding author: Bhavini Patel Murthy, [email protected].
1
Immunization Services Division, National Center for Immunization and
Respiratory Diseases, CDC;
2
CDC COVID-19 Response Team;
3
Stat-Epi
Associates, Inc., Ponte Vedra Beach, Florida.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. No potential conflicts of interest were disclosed.
References
1. CDC. COVID data tracker. Atlanta, GA: US Department of Human
Services, CDC; 2021. Accessed July 17, 2021. https://covid.cdc.gov/
covid-data-tracker
2. Havers FP, Whitaker M, Self JL, et al.; COVID-NET Surveillance
Team. Hospitalization of adolescents aged 12–17 years with laboratory-
confirmed COVID-19—COVID-NET, 14 states, March 1, 2020–
April 24, 2021. MMWR Morb Mortal Wkly Rep 2021;70:851–7.
PMID:34111061 https://doi.org/10.15585/mmwr.mm7023e1
3. US Census Bureau. Population and housing unit estimates. Washington,
DC: US Department of Commerce, US Census Bureau; 2021. Accessed
April 7, 2021. https://www.census.gov/programs-surveys/popest.html
4. Gharpure R, Guo A, Bishnoi CK, et al. Early COVID-19 first-dose
vaccination coverage among residents and staff members of skilled
nursing facilities participating in the pharmacy partnership for long-term
care program—United States, December 2020–January 2021. MMWR
Morb Mortal Wkly Rep 2021;70:178–82. PMID:33539332 https://
doi.org/10.15585/mmwr.mm7005e2
5. Community Preventive Services Task Force. The guide to community
preventive services: vaccination programs: schools and organized child
care centers. Atlanta, GA: US Department of Health and Human
Services, CDC, Community Preventive Services Task Force; 2021.
Accessed July 17, 2021. https://www.thecommunityguide.org/findings/
vaccination-programs-schools-and-organized-child-care-centers
Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1213
US Department of Health and Human Services/Centers for Disease Control and Prevention
6. CDC. Considerations for planning school-located vaccination clinics.
Atlanta, GA: US Department of Human Services, CDC; 2021. Accessed
July 27, 2021. https://www.cdc.gov/vaccines/covid-19/planning/school-
located-clinics.html
7. Oster E, Jack R, Halloran C, et al. Disparities in learning mode access
among K–12 students during the COVID-19 pandemic, by race/
ethnicity, geography, and grade level—United States, September 2020–
April 2021. MMWR Morb Mortal Wkly Rep 2021;70:953–8.
PMID:34197363 https://doi.org/10.15585/mmwr.mm7026e2
8. Scherer AM, Gedlinske AM, Parker AM, et al. Acceptability of adolescent
COVID-19 vaccination among adolescents and parents of adolescents—
United States, April 15–23, 2021. MMWR Morb Mortal Wkly Rep
2021;70:997–1003. PMID:34264908 https://doi.org/10.15585/mmwr.
mm7028e1
9. Morgan L, Schwartz JL, Sisti DA. COVID-19 vaccination of minors
without parental consent: respecting emerging autonomy and advancing
public health. JAMA Pediatr 2021. Epub July 12, 2021. PMID:34251411
https://doi.org/10.1001/jamapediatrics.2021.1855
10. Murthy BP, Zell E, Kirtland K, et al. Impact of the COVID-19 pandemic
on administration of selected routine childhood and adolescent
vaccinations—10 U.S. jurisdictions, March–September 2020. MMWR
Morb Mortal Wkly Rep 2021;70:840–5. PMID:34111058 https://doi.
org/10.15585/mmwr.mm7023a2

Morbidity and Mortality Weekly Report
1214 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
Outbreak Associated with SARS-CoV-2 B.1.617.2 (Delta) Variant in an
Elementary School — Marin County, California, May–June 2021
Tracy Lam-Hine, MBA
1,2
; Stephen A. McCurdy, MD
1,3
; Lisa Santora, MD
1
; Lael Duncan, MD
1
; Russell Corbett-Detig, PhD
4
;
Beatrix Kapusinszky, PhD
5
; Matthew Willis, MD
1
On August 27, 2021, this report was posted as an MMWR Early
Release on the MMWR website (https://www.cdc.gov/mmwr).
On May 25, 2021, the Marin County Department of Public
Health (MCPH) was notified by an elementary school that
on May 23, an unvaccinated teacher had reported receiving
a positive test result for SARS-CoV-2, the virus that causes
COVID-19. The teacher reported becoming symptomatic on
May 19, but continued to work for 2 days before receiving
a test on May 21. On occasion during this time, the teacher
read aloud unmasked to the class despite school requirements
to mask while indoors. Beginning May 23, additional cases of
COVID-19 were reported among other staff members, students,
parents, and siblings connected to the school. To characterize
the outbreak, on May 26, MCPH initiated case investigation
and contact tracing that included whole genome sequencing
(WGS) of available specimens. A total of 27 cases were identified,
including that of the teacher. During May 23–26, among the
teacher’s 24 students, 22 students, all ineligible for vaccination
because of age, received testing for SARS-CoV-2; 12 received
positive test results. The attack rate in the two rows seated clos-
est to the teacher’s desk was 80% (eight of 10) and was 28%
(four of 14) in the three back rows (Fisher’s exact test; p = 0.036).
During May 24–June 1, six of 18 students in a separate grade at
the school, all also too young for vaccination, received positive
SARS-CoV-2 test results. Eight additional cases were also identi-
fied, all in parents and siblings of students in these two grades.
Among these additional cases, three were in persons fully vac-
cinated in accordance with CDC recommendations (1). Among
the 27 total cases, 22 (81%) persons reported symptoms; the most
frequently reported symptoms were fever (41%), cough (33%),
headache (26%), and sore throat (26%). WGS of all 18 available
specimens identified the B.1.617.2 (Delta) variant. Vaccines are
effective against the Delta variant (2), but risk of transmission
remains elevated among unvaccinated persons in schools without
strict adherence to prevention strategies. In addition to vaccina-
tion for eligible persons, strict adherence to nonpharmaceutical
prevention strategies, including masking, routine testing, facility
ventilation, and staying home when symptomatic, are important
to ensure safe in-person learning in schools (3).
Investigation and Findings
The outbreak location was an elementary school in Marin
County, California, which serves 205 students in prekindergarten
through eighth grade and has 24 staff members. Each grade
includes 20 to 25 students in single classrooms. Other than two
teachers, one of whom was the index patient, all school staff
members were vaccinated (verified in California’s Immunization
Registry). The index patient became symptomatic on May 19
with nasal congestion and fatigue. This teacher reported attending
social events during May 13–16 but did not report any known
COVID-19 exposures and attributed symptoms to allergies. The
teacher continued working during May 17–21, subsequently
experiencing cough, subjective fever, and headache. The school
required teachers and students to mask while indoors; interviews
with parents of infected students suggested that students’ adher-
ence to masking and distancing guidelines in line with CDC
recommendations (3) was high in class. However, the teacher was
reportedly unmasked on occasions when reading aloud in class.
On May 23, the teacher notified the school that they received a
positive result for a SARS-CoV-2 test performed on May 21 and
self-isolated until May 30. The teacher did not receive a second
COVID-19 test, but reported fully recovering during isolation.
The index patient’s students began experiencing symptoms
on May 22. During May 23–26, among 24 students in this
grade, 22 were tested. A COVID-19 case was defined as a
positive SARS-CoV-2 reverse transcription–polymerase chain
reaction (RT-PCR) or antigen test result.* Twelve (55%) of the
22 students received a positive test result, including eight who
experienced symptom onset during May 22–26. Throughout
this period, all desks were separated by 6 ft. Students were
seated in five rows; the attack rate in the two rows seated
closest to the teacher’s desk was 80% (eight of 10) and was
28% (four of 14) in the three back rows (Fisher’s exact test;
p = 0.036) (Figure 1).
On May 22, students in a another classroom, who dif-
fered in age by 3 years from the students in the class with the
index case and who were also ineligible for vaccination began
to experience symptoms. The two classrooms were separated by
a large outdoor courtyard with lunch tables that were blocked
off from use with yellow tape. All classrooms had portable
* https://cdn.ymaws.com/www.cste.org/resource/resmgr/ps/
positionstatement2020/Interim-20-ID-02_COVID-19.pdf
Please note: This report has been corrected.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1215
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 1. Classroom layout and seating chart for 24 students in index patient’s class, by SARS-CoV-2 testing date, result or status, and
symptoms — Marin County, California, May–June 2021
Teacher’s desk
Symptomatic May 19
Positive May 21
(index patient)
Symptomatic May 23
Positive May 26
Symptomatic May 24
Positive May 25
Symptomatic May 24
Positive May 25
Symptomatic May 22
Positive May 23
Symptomatic May 24
Positive May 24
Symptomatic May 23
Positive May 24
Positive May 24
Symptomatic May 26
Positive May 26
Positive May 24
Positive May 26
Positive May 26
Symptomatic
(date unknown)
Positive May 26
Negative May 26
Negative May 26
Negative May 26
Symptomatic case Asymptomatic case Negative test result No testing
Negative May 26
Negative May 26 Negative May 26
Negative
May
25
Negative May 26
No testing
(Empty seat)
No testing
Air lter
Classroom door
(left open)
Board in front of classroom
Windows (left open)
Windows (left open)
Negative May 26
Negative May 26
6 ft 6 ft 6 ft 6 ft
6 ft
6 ft
6 ft
6 ft
high-efficiency particulate air filters and doors and windows
were left open. Fourteen of 18 students in this separate grade
received testing; six tests had positive results. Investigation
revealed that one student in this grade hosted a sleepover on
May 21 with two classmates from the same grade. All three of
these students experienced symptoms after the sleepover and
received positive SARS-CoV-2 test results. Among infected
students in this class, test dates ranged from May 24 to June 1;
symptom onset occurred during May 22–31.
In addition to the documented infections in the two initial
grades, cases were identified in one student each from four
other grades. Three patients were symptomatic; dates for test-
ing were May 30 or June 2. These four students were siblings
of three students with cases in the index patient’s class, and
exposure was assumed to have occurred in their respective
homes. In addition to the teacher and 22 infected students,
four parents of students with cases were also infected, for a
total of 27 cases (23 confirmed by RT-PCR and four by anti-
gen testing) (Figure 2). Among the five infected adults, one

Morbidity and Mortality Weekly Report
1216 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 2. Timeline of SARS-CoV-2 illness onset* after onset in the index patient (A) and presumed transmission
†
pathway (B) among students,
siblings, and parents, relative to onset in the index patient — Marin County, California, May 2021
0 5 10
No. of days since onset in index patient
No. of cases
15 20
0
0
1
2
3
4
5
6
7
8
5
A
B
10 15 20
Index patient
Case in index patient’s class
Case in other aected class
Sibling of infected student in index patient’s class
Parent of infected student in other aected class
Parent of infected student in index patient’s class
Symptom onset in index patient: day 0
Sleepover event: day 2
Presumed exposure pathway
* Symptom onset date or specimen collection date, if asymptomatic.
†
Presumed transmission based on phylogenetic and epidemiologic analyses.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1217
US Department of Health and Human Services/Centers for Disease Control and Prevention
parent and the teacher were unvaccinated; the others were fully
vaccinated. The vaccinated adults and one unvaccinated adult
were symptomatic with fever, chills, cough, headache, and loss
of smell. No other school staff members reported becoming ill.
No persons infected in this outbreak were hospitalized. This
activity was reviewed by Marin County and was conducted
consistent with applicable law.
Public Health Response
On May 26 and June 2, MCPH held testing events at the
school as part of outbreak control. During these 2 days, 231
persons were tested, including 194 of 205 students, 21 of
24 staff members and teachers, and 16 parents and siblings
of students. The California Department of Public Health
assisted with guidance, application of additional prevention
strategies, and on-site testing. Community contacts and all
students and staff members were encouraged to participate.
Specimens for WGS were collected during May 26–June 12;
all 18 positive specimens with detectable virus (cycle threshold
value <32) were sequenced using ClearDx instruments (Clear
Laboratories), Oxford Nanopore MinION sequencing tech-
nology, and SARS-CoV-2 ARTIC V3 protocol for amplicon
sequencing.
†
Consensus genome assembly was performed in
Terra using Titan Clear Laboratories workflow.
§
All sequences
generated were classified as the Delta variant. A phylogenetic
tree was constructed using the UShER pipeline and visual-
ized using Auspice.us
¶
(4) (Figure 3). Eleven sequences were
genetically indistinguishable from one another; seven sequences
contained additional single nucleotide variations. Among the
indistinguishable specimens, six were from students of the
index patient, four were from students in the separate grade,
and one was from a sibling of a student in the index patient’s
class, suggesting that infections occurring in the two grades
likely were part of the same outbreak. The epidemiologic link
between the two grades remains unknown but is thought to
be interaction at the school. Five additional related sequences
from community cases (in two adults and three children) were
later identified, including three more genetically indistinguish-
able sequences. One was from an adult with specimen collec-
tion 1 day before symptom onset in the index patient. Case
investigation records did not establish an epidemiologic link
between these five community cases and the school outbreak.
Following the outbreak, infected persons were isolated for
10 days after onset of symptoms (or positive test date for
asymptomatic cases). All students with known exposure to an
infected person quarantined at home for 10 days following their
†
https://www.protocols.io/view/ncov-2019-sequencing-protocol-bbmuik6w
§
https://public-health-viral-genomics-theiagen.readthedocs.io/en/latest/titan_
workflows.html
¶
https://auspice.us
last known contact. Unvaccinated household and community
contacts were directed to quarantine for 10 days following their
last known exposure to an infected person, with the option to
leave quarantine after 7 days if they remained asymptomatic
and received a negative test result from a specimen collected
on day 5 of quarantine or later. The two affected classrooms
were closed and sanitized during May 21–30 and May 24–
June 2, respectively.
Discussion
This outbreak of COVID-19 that originated with an unvac-
cinated teacher highlights the importance of vaccinating
school staff members who are in close indoor contact with
children ineligible for vaccination as schools reopen. The
outbreak’s attack rate highlights the Delta variant’s increased
transmissibility**and potential for rapid spread, especially in
unvaccinated populations such as schoolchildren too young
for vaccination. However, transmission to community contacts
appeared lower than that of some previously reported Delta
variant outbreaks (5). Further transmission might have been
prevented by high levels of community vaccination; at the
time of this outbreak, approximately 72% of eligible persons
in the city where the school is located were fully vaccinated.
††
These findings support evidence that the current COVID-19
vaccines with Food and Drug Administration approval or
Emergency Use Authorization are effective against the Delta
variant; however, transmission risk remains elevated among
unvaccinated persons in schools. In addition to vaccination
of eligible persons, implementation of and strict adherence
to multipronged nonpharmaceutical prevention strategies
including proper masking, routine testing, ventilation, and
staying home while symptomatic are important to ensure safe
school instruction.
The findings in this study are subject to at least three limita-
tions. First, the teacher’s specimen was unavailable for WGS,
which prevented phylogenetic identification of the outbreak’s
index patient. Second, testing for parents and siblings was
self-directed and took place mostly outside the school setting,
which could have led to underascertainment of cases. Finally,
challenges in testing acceptance among possible contacts from
outside the school led to difficulty in characterizing the out-
break’s actual spread into the community, as is evidenced by
later discovery of additional community cases with sequences
indistinguishable from those in the school outbreak.
Ineligibility because of age and lack of vaccination contribute
to persistent elevated risk for outbreaks in schools, especially as
new SARS-CoV-2 variants emerge. However, implementation
** https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-info.html
(accessed August 10, 2021)
††
https://coronavirus.marinhhs.org/ (accessed August 10, 2021)
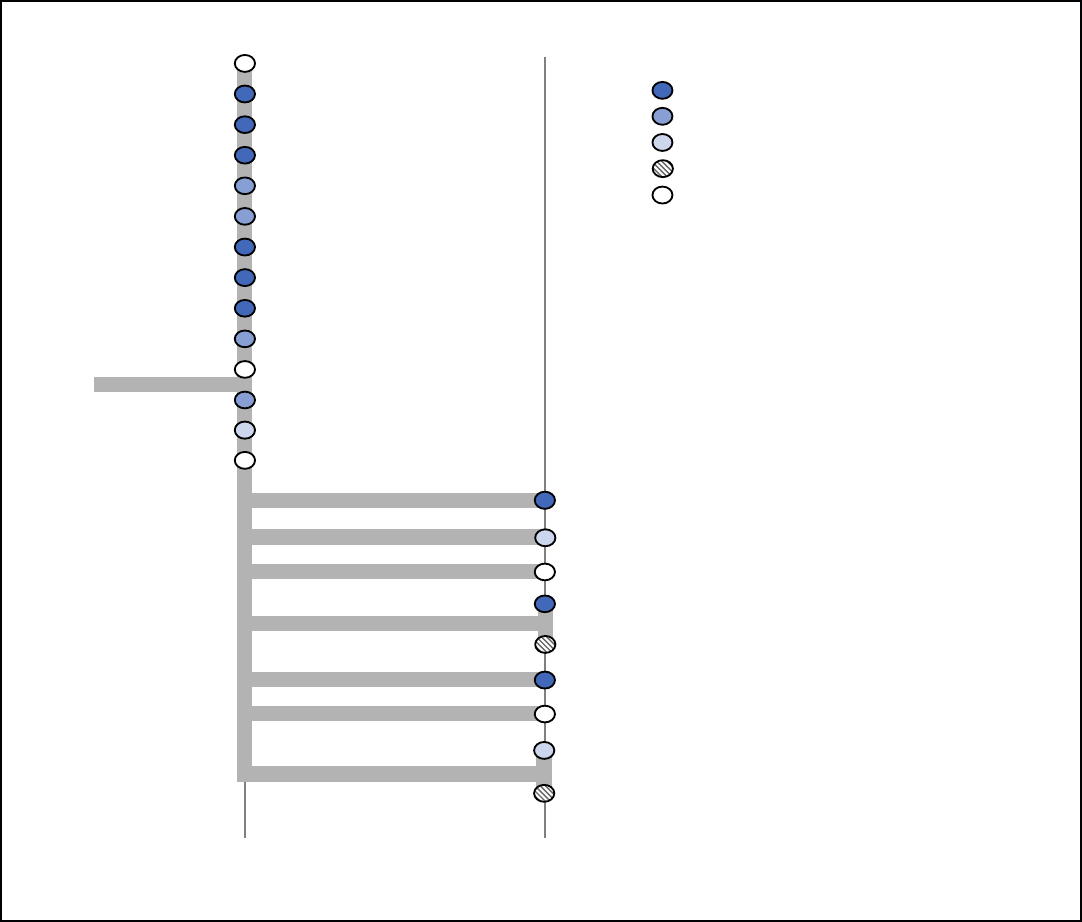
Morbidity and Mortality Weekly Report
1218 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 3. Phylogenetic tree*
,†
of SARS-CoV-2 whole genome sequences and specimen collection dates
§
from a COVID-19 outbreak in an
elementary school
¶
— Marin County, California, May–June 2021
May 18
May 26
May 26
May 26
May 26
May 26
May 27
May 27
May 27
May 27
May 27
May 29
May 30
Jun 8
C1009T
A29083G
G14428T
C27641T
G23501T
A22034G
A3712G
A28750T
SNVs
34 35
May 26
May 26
May 26
May 26
Jun 1
May 27
May 29
Jun 2
Jun 12
Case in index patient’s class
Case in other aected class
Sibling of infected student in index patient’s class
Parent of infected student in index patient’s class
No identied link
Abbreviations: SNV = single nucleotide variant; WGS = whole genome sequencing.
* Phylogenetic tree was created with UShER, which uses the Fitch–Sankoff algorithm (a maximum parsimony-based phylogenetic placement approach). https://doi.
org/10.1038/s41588-021-00862-7
†
Specimen for the index patient was not available for WGS and is not included on the phylogenetic tree.
§
Dates in this diagram reflect the collection date for specimens that underwent WGS; thus dates might differ from those reported in the text for persons whose initial
specimens were discarded.
¶
Branches are labeled with SNVs; cases (circles) are color-coded to indicate social relationship within the outbreak and labeled with the collection date for the specimen
that was sequenced. Vertical lines represent genetically identical viruses; horizontal lines represent genetic descendants with additional SNVs. All sequenced
specimens are classified as the SARS-CoV-2 B.1.617.2 (Delta) variant.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1219
US Department of Health and Human Services/Centers for Disease Control and Prevention
Summary
What is already known about this topic?
The SARS-CoV-2 B.1.617.2 (Delta) variant is highly transmissible.
Prevention guidance in schools varies by jurisdiction.
What is added by this report?
During May 23–June 12, 2021, 26 laboratory-confirmed
COVID-19 cases occurred among Marin County, California,
elementary school students and their contacts following
exposure to an unvaccinated infected teacher. The attack rate in
one affected classroom was 50%; risk correlated with seating
proximity to the teacher.
What are the implications for public health practice?
Vaccines are effective against the Delta variant, but transmis-
sion risk remains elevated among unvaccinated persons in
schools. In addition to vaccination, strict adherence to multiple
nonpharmaceutical prevention strategies, including masking,
are important to ensure safe school instruction.
of multiple prevention strategies within schools can mitigate this
risk. The rapid transmission and vaccine breakthrough infections
in this outbreak might have resulted from the schoolchildren’s
vulnerability because of ineligibility for vaccination, coupled
with the high transmissibility of the Delta variant. New evidence
of the Delta variant’s high transmissibility, even among fully vac-
cinated persons (6,7), supports recommendations for universal
masking in schools
§§
(1). Further application of nonpharmaceu-
tical prevention strategies, including routine testing, ventilation,
and staying home while symptomatic, are also important for
protecting the health of schoolchildren ineligible for vaccination
because of their age (3). In addition, phylogenetic analysis can
help to clarify transmission patterns and characterize outbreak
progression. Capacity-building efforts offered by regional and
state laboratories enabled more sophisticated analysis at the local
level; such efforts might be useful as vaccination rates increase,
new variants emerge, and outbreaks become more localized.
§§
https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/COVID-19/K-12-
Guidance-2021-22-School-Year.aspx (accessed August 2, 2021)
Acknowledgments
COVID-19 Case and Contact Investigation Unit, Marin County
Public Health; Naomi Bardach, Kathleen Harriman, Carol Glaser,
Erica Pan, California Department of Public Health; John Oeltmann,
Patrick Moonan, CDC; Teionna Cunningham, Napa-Solano-Yolo-
Marin-Mendocino Public Health Laboratory; Patrick Ayescue,
Allison Black, Chan Zuckerberg BioHub.
Corresponding author: Tracy Lam-Hine, tlam-hine@marincounty.org.
1
County of Marin Department of Health and Human Services, San Rafael,
California;
2
UC Berkeley School of Public Health, University of California,
Berkeley, California;
3
UC Davis School of Medicine, University of California,
Sacramento, California;
4
Baskin School of Engineering, University of California,
Santa Cruz, California;
5
Napa-Solano-Yolo-Marin-Mendocino County Public
Health Laboratory, Fairfield, California.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. Lael Duncan reports Pfizer and Moderna stock
ownership. No other potential conflicts of interest were disclosed.
References
1. CDC. COVID-19: when you’ve been fully vaccinated: how to protect
yourself and others. Atlanta, GA: US Department of Health and Human
Services, CDC; 2021. Accessed July 27, 2021. https://www.cdc.gov/
coronavirus/2019-ncov/vaccines/fully-vaccinated.html
2. Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of
Covid-19 vaccines against the B.1.617.2 (Delta) Variant. N Engl J
Med 2021;385:585–94. PMID:34289274 https://doi.org/10.1056/
NEJMoa2108891
3. CDC. COVID-19: guidance for COVID-19 prevention in K-12 schools.
Atlanta, GA: US Department of Health and Human Services, CDC;
2021. Accessed August 5, 2021. https://www.cdc.gov/coronavirus/2019-
ncov/community/schools-childcare/k-12-guidance.html
4. Turakhia Y, Thornlow B, Hinrichs AS, et al. Ultrafast Sample placement
on Existing tRees (UShER) enables real-time phylogenetics for the
SARS-CoV-2 pandemic. Nat Genet 2021;53:809–16. PMID:33972780
https://doi.org/10.1038/s41588-021-00862-7
5. Dougherty K, Mannell M, Naqvi O, Matson D, Stone J. SARS-CoV-2
B.1.617.2 (Delta) variant COVID-19 outbreak associated with a
gymnastics facility—Oklahoma, April–May 2021. MMWR Morb Mortal
Wkly Rep 2021;70:1004–7. PMID:34264910 https://doi.org/10.15585/
mmwr.mm7028e2
6. Brown CM, Vostok J, Johnson H, et al. Outbreak of SARS-CoV-2
infections, including COVID-19 vaccine breakthrough infections,
associated with large public gatherings—Barnstable County, Massachusetts,
July 2021. MMWR Morb Mortal Wkly Rep 2021;70:1059–62.
PMID:34351882 https://doi.org/10.15585/mmwr.mm7031e2
7. Israeli Ministry of Health. Explanation about the effectiveness of the
vaccine for coronavirus in Israel. Jerusalem, Israel: Israel Ministry of
Health; 2021. Accessed July 29, 2021. https://www.gov.il/en/departments/
news/06072021-04

Morbidity and Mortality Weekly Report
1220 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
COVID-19 Case Rates in Transitional Kindergarten Through Grade 12 Schools and in
the Community — Los Angeles County, California, September 2020–March 2021
Sherry Yin, MPH
1
; Kaitlin Barnes, MBA
2
; Rebecca Fisher, MPH
1
; Dawn Terashita, MD
1
; Andrea A. Kim, PhD
1
On August 27, 2021, this report was posted as an MMWR Early
Release on the MMWR website (https://www.cdc.gov/mmwr).
In-person instruction during the COVID-19 pandemic con-
cerns educators, unions, parents, students, and public health
officials as they plan to create a safe and supportive learning
environment for children and adolescents (1). Los Angeles
County (LAC), the nation’s largest county, has an estimated
population of 10 million, including 1.7 million children and
adolescents aged 5–17 years (2). LAC school districts moved
to remote learning for some or all students in transitional
kindergarten* through grade 12 (TK–12) schools during the
2020–21 school year (3). Schools that provided in-person
instruction were required by LAC Health Officer orders to
implement prevention measures such as symptom screening,
masking, physical distancing, cohorting, and contact tracing
(4). This analysis compares COVID-19 case rates in TK–12
schools among students and staff members who attended
school in person with LAC case rates during September 2020–
March 2021.
LAC schools are required to report all laboratory-confirmed
COVID-19 cases in persons who were on campus during their
incubation or infectious period to the LAC Department of
Public Health (DPH).
†
School-associated cases were defined
as cases among students and staff members who were on
campus for any length of time from 14 days before symp-
tom onset or testing (whichever was earlier) until isolation.
Cases among students and staff members who participated
exclusively in online learning or worked remotely were not
considered school-associated cases. DPH and the LAC Office
of Education also collected information from the county’s 80
public school districts on the estimated number of students
and staff members routinely on campus each month during
September 2020–March 2021. Monthly attendance was pro-
rated based on when schools opened and ranged from 2,738
* Transitional kindergarten is a public school program serving to bridge preschool
and kindergarten.
†
During the observation period, school districts recommended diagnostic testing
for students and staff members to identify persons with active infection based on
symptoms and exposure. In addition to mandatory laboratory or provider
reporting of positive COVID-19 nucleic acid amplification test (NAAT) and
antigen test results, schools also notified DPH of cases occurring on campus.
Schools relied on staff members, students, parents and guardians, and testing
programs where available to inform them of cases and worked with DPH to
identify and provide testing for close contacts on campus. The Los Angeles Unified
School District (largest of the 80 school districts in the county) implemented a
screening testing program using NAATs for staff members and students on campus
beginning September 2020 and reported all positive results to DPH.
to 62,369 students and 36,862 to 45,757 staff members.
Student and staff member case rates were calculated using the
number of school-associated cases reported to DPH, assigned
to a month by episode date, and divided by monthly atten-
dance. Community case rates among children and adolescents
aged 5–17 years and adults aged 18–79 years were calculated
using the number of reported cases in LAC divided by the
2019 county population.
§
Standard errors were calculated for
school-associated rates. Analyses were conducted using SAS
(version 9.4; SAS Institute). This public health surveillance
activity was approved by DPH.
During September 1, 2020–March 31, 2021, a total of
463 school-associated cases were reported among students
attending public TK–12 schools in person and 3,927 among
staff members working on-site. During the same period,
105,577 cases among children and adolescents aged 5–17 years
and 771,409 cases among adults aged 18–79 years were
reported in LAC. School-associated case rates remained low
among students, ranging from 110 per 100,000 in September
to 859 in December 2020 (Figure). Case rates among all chil-
dren and adolescents aged 5–17 years in the county were higher
during most of the period, ranging from 167 per 100,000 in
September to 2,938 in December 2020. School-associated case
rates among staff members were lowest in September 2020
(125 per 100,000), peaked in December 2020 (4,109),
and fell sharply through March 2021 (188). These rates
reflected the trend among all adults aged 18–79 years in
the county (319 per 100,000 in September 2020; 4,624 in
December 2020; and 181 in March 2021) but were lower for
most of the period. As total cases fell sharply in February, rates
across the four groups declined to similar levels by March 2021.
The findings in this report are subject to at least three limitations.
First, these findings from one county should be interpreted with cau-
tion and are not necessarily generalizable to other areas. Second, the
analysis did not include the entire school year because estimates of
students and staff members on campus were collected only through
March 2021. Finally, because of limited available information about
the population on campus, rates were unadjusted and did not
examine potential differences in demographic and socioeconomic
characteristics by in-person status. However, sensitivity analysis
showed similar trends across LAC’s eight Service Planning Areas.
§
Cities of Long Beach and Pasadena were not included because they have their own
health departments separate from LAC DPH. The adult age range reflects the age
range of staff members working at TK–12 schools in LAC during the analysis period.
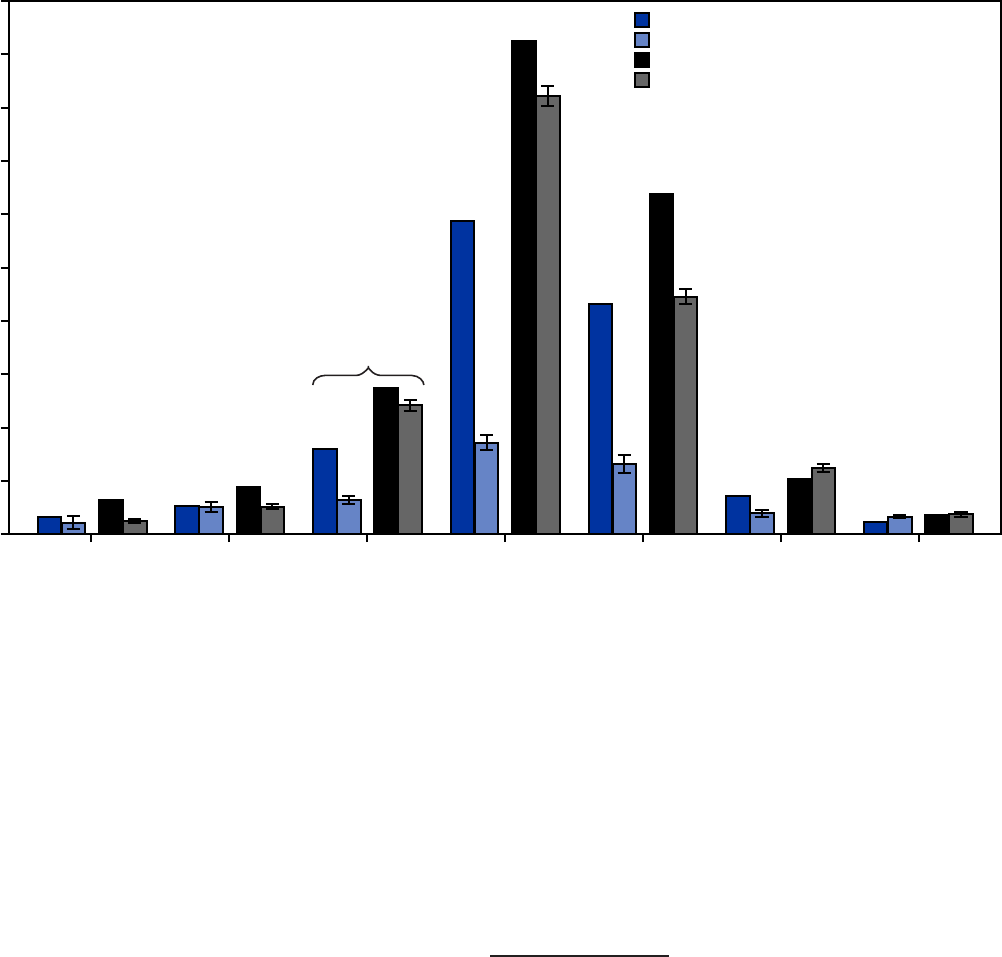
Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1221
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE. COVID-19 case rates* among children, adolescents, and adults
†
in transitional kindergarten through grade 12 schools and in the
community, by month — Los Angeles County, California, September 2020–March 2021
All children and adolescents aged 5–17 yrs in LAC
Students attending public TK–12 schools
All adults aged 18–79 yrs in LAC
Sta members working in public TK–12 schools
Support Width Options
Page wide = 7.5”
QuickStats = 5.0”
1½ columns = 4.65”
1 column = 3.57”
0
500
1,000
1,500
2,000
2,500
3,000
3,500
4,000
4,500
5,000
Sep 2020 Oct 2020 Nov 2020 Dec 2020 Jan 2021 Feb 2021 Mar 2021
Cases per 100,000 population
Month, year
Beginning of surge
(Nov 2020)
Abbreviations: LAC = Los Angeles County; TK–12 = transitional kindergarten through grade 12.
* New cases per month per 100,000 persons; standard error bars shown for school case rates.
†
Adult staff members comprise all school employees and associated workers on campus, including teachers, nurses, public safety officers, administrative staff members,
campus aides, food service workers, custodians, and transportation staff members.
The findings suggest that implementing recommended
prevention measures might protect children, adolescents,
and adults from COVID-19 in TK–12 schools. The level of
protection appears to be higher in children and adolescents
than in adults, which is promising for children aged <12 years
because no COVID-19 vaccine is currently authorized for this
age group. In schools with safety protocols in place for preven-
tion and containment, case rates in children and adolescents
were 3.4 times lower during the winter peak compared with
rates in the community. This analysis reflects transmission pat-
terns before the more transmissible SARS-CoV-2 B.1.617.2
(Delta) variant became predominant in the United States.
A multipronged prevention strategy, including masking,
physical distancing, testing, and most recently vaccination of
children and adolescents aged ≥12 years, will remain critical to
reducing transmission as more students return to the classroom
(5). These findings from a large and diverse county present
preliminary evidence that schools provided a relatively safe
environment during the 2020–21 school year.
Acknowledgments
Sharon Balter, Katie Chun, Barbara Ferrer, Robert Gilchick,
Caitlin Harvey, Mirna Ponce Jewell, Lauren O’Neal, Ellen Paddock,
Alexander Serrano, Nailah Smith, Los Angeles County Department
of Public Health; Division of Acute Communicable Disease Control,
Education Sector Unit, Los Angeles County Department of Public
Health; Debra Duardo, Elizabeth Graswich, Arturo Valdez, Los Angeles
County Office of Education; administrators, staff members, students,
families, and unions in the 80 Los Angeles County school districts.
Corresponding author: Sherry Yin, [email protected].gov.
1
Los Angeles County Department of Public Health, California;
2
Los Angeles
County Office of Education, California.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. No potential conflicts of interest were disclosed.
Morbidity and Mortality Weekly Report
1222 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
References
1. Honein MA, Barrios LC, Brooks JT. Data and policy to guide opening
schools safely to limit the spread of SARS-CoV-2 infection. JAMA
2021;325:823–4. PMID:33497433 https://doi.org/10.1001/
jama.2021.0374
2. County of Los Angeles, Internal Services Department, Information
Technology Service, Urban Research-GIS Section. Population and poverty
estimates of Los Angeles County tract-city splits by age, sex, and race-
ethnicity. Los Angeles, CA: County of Los Angeles; 2019.
3. California Safe Schools for All. State of California safe schools for all hub.
Sacramento, CA: State of California; 2021. Accessed June 18, 2021.
https://schools.covid19.ca.gov/
4. County of Los Angeles Department of Public Health. Order of the Health
Officer. Reopening protocols for K–12 schools: Appendix T1. Los Angeles,
CA: County of Los Angeles; 2021. Accessed June 14, 2021. http://
publichealth.lacounty.gov/media/coronavirus/docs/protocols/Reopening_
K12Schools.pdf
5. CDC. COVID-19: guidance for COVID-19 prevention in K–12 schools.
Atlanta, GA: US Department of Health and Human Services, CDC;
2021. Accessed July 19, 2021. https://www.cdc.gov/coronavirus/2019-
ncov/community/schools-childcare/k-12-guidance.html

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1223
US Department of Health and Human Services/Centers for Disease Control and Prevention
Epidemiologically Linked COVID-19 Outbreaks at a Youth Camp and Men’s
Conference — Illinois, June–July 2021
James Matthias, MPH
1
; Sarah Patrick, PhD
2
; Ann Wiringa, PhD
2
; Amanda Pullman, MPH, MT
1
; Stephanie Hinton, MS, MHS
1
; Jon Campos
3
;
Terri Belville
4
; Mallory Sinner, MPH
2
; Torrie T. Buchanan, PhD
5
; Bryan Sim
5
; Kristin E. Goldesberry, MPH, MLS
5
On August 31, 2021, this report was posted as an MMWR Early
Release on the MMWR website (https://www.cdc.gov/mmwr).
On June 30, 2021, the Illinois Department of Public Health
(IDPH) contacted CDC concerning COVID-19 outbreaks
at two events sponsored by the same organization: a 5-day
overnight church camp for persons aged 14–18 years and a
2-day men’s conference. Neither COVID-19 vaccination nor
COVID-19 testing was required before either event. As of
August 13, a total of 180 confirmed and probable cases had
been identified among attendees at the two events and their
close contacts. Among the 122 cases associated with the camp
or the conference (primary cases), 18 were in persons who were
fully vaccinated, with 38 close contacts. Eight of these 38 close
contacts subsequently became infected with SARS-CoV-2,
the virus that causes COVID-19 (secondary cases); among
the eight close contacts with secondary cases, one half (four)
were fully vaccinated. Among the 180 total persons with
outbreak-associated cases, five (2.8%) were hospitalized; no
deaths occurred. None of the vaccinated persons with cases
were hospitalized. Approximately 1,000 persons across at least
four states were exposed to SARS-CoV-2 through attendance
at these events or through close contact with a person who had
a primary case. This investigation underscores the impact of
secondary SARS-CoV-2 transmission during large events, such
as camps and conferences, when COVID-19 prevention strate-
gies are not implemented. In Los Angeles County, California,
during July 2021, when the SARS-CoV-2 B.1.617.2 (Delta)
variant was predominant, unvaccinated residents were
five times more likely to be infected and 29 times more likely
to be hospitalized from infection than were vaccinated resi-
dents (1). Implementation of multiple prevention strategies,
including vaccination and nonpharmaceutical interventions
such as masking, physical distancing, and screening testing, are
critical to preventing SARS-CoV-2 transmission and serious
complications from COVID-19.
Investigation and Findings
The camp was held during June 13–17, 2021, and included
persons aged 14–18 years from a church organization with
multiple locations across western Illinois, Iowa, and Missouri.
A total of 294 campers arrived on buses or large passenger vans
and were met by 41 staff members. No proof of COVID-19
vaccination or SARS-CoV-2 pretesting or testing on arrival
was required, and the list of suggested items to bring to camp
did not include masks. Campers were housed in large, shared
boarding facilities of approximately 100 campers each, dined in
a cafeteria together, participated in indoor and outdoor small
group activities in which campers were with the same persons
during program events, and participated in activities with all
campers during all 5 days.
On June 16, the second to last camp day, one camper
departed after becoming ill with a fever and respiratory
symptoms and subsequently received a laboratory-confirmed
diagnosis of COVID-19. Campers and staff members were
notified, encouraged to receive SARS-CoV-2 testing, and
instructed to quarantine per CDC guidance and isolate if they
received a positive test result.*
Six camp staff members who received positive SARS-CoV-2
test results also attended the conference during June 18–19 but
did not receive their results until after the conference ended;
all six staff members had symptom onset during June 17–29.
†
The conference was held at a different location from the camp
and included 500 attendees and 30 staff members, and, as with
the camp, no COVID-19 vaccination, SARS-CoV-2 testing, or
masking was required. The first case in a conference attendee
was diagnosed on June 21, 2 days after the conference. After
conference-associated COVID-19 cases were identified, confer-
ence attendees and staff members were notified, encouraged to
receiving SARS-CoV-2 testing, and instructed to quarantine per
CDC guidance and isolate if they received a positive test result.
A confirmed case was defined as receipt of a positive
SARS-CoV-2 nucleic acid amplification test result in a camp
or conference attendee, and a probable case was defined as
receipt of a positive SARS-CoV-2 antigen test result.
§
Cases
were identified through case investigation after laboratory
notification of a positive test result. Information on symptom
onset or specimen collection dates (available for 174 [97%] of
* Persons with positive SARS-CoV-2 test results were instructed to isolate in
accordance with CDC guidance at the time (https://www.cdc.gov/
coronavirus/2019-ncov/hcp/duration-isolation.html), and close contacts were
instructed to quarantine in accordance with CDC guidance at the time (https://
www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/quarantine.html).
†
Six staff members (three at the camp and three at the conference) were identified
as having cases on the basis of their symptom onset date. Because the complete
rosters had not been provided to IDPH, persons might have been counted as
attendees at both events.
§
https://ndc.services.cdc.gov/case-definitions/coronavirus-
disease-2019-2020-08-05/

Morbidity and Mortality Weekly Report
1224 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
180 persons), COVID-19 vaccination status (from the state
immunization registry), county of residence, test results, and
viral sequencing data (available for 31 [17%] persons) was
collected for persons with camp- and conference-associated
cases (primary cases). IDPH’s contact tracing system identified
close contacts of persons with primary cases; close contacts
were defined as unmasked persons who were within 6 ft of a
person with a primary case for >15 minutes during a 24-hour
period while that person was infectious, which was 2 days
before through 10 days after symptom onset (for symptomatic
persons) or after specimen collection date (for asymptomatic
persons). Secondary cases were defined as COVID-19 cases
that occurred in close contacts of persons with a primary case
of confirmed or probable COVID-19.
Persons who had received 2 doses of Pfizer BioNTech or
Moderna COVID-19 mRNA vaccine or 1 dose of Janssen
(Johnson & Johnson) COVID-19 vaccine ≥14 days before
exposure were considered fully vaccinated. IDPH laboratories
performed whole genome sequencing on 25 of 31 available
specimens.
¶
Descriptive analyses were conducted to determine
the distribution of cases by vaccination status, the proportion
of SARS-CoV-2 variants, and the secondary transmission
rate. This activity was reviewed by CDC and was conducted
consistent with applicable federal law and CDC policy.**
As of August 13, a total of 180 outbreak-associated cases
had been identified, including 122 primary cases, 87 (48%) of
which were in camp attendees (among 335 total campers and
staff members; attack rate=26%) and 35 (19%) in confer-
ence attendees (among 530 total conference participants and
staff members; attack rate=7%). Among 262 close contacts
of camp or conference attendees, 58 (22%) secondary cases
were identified, representing 32% of the 180 identified cases
(Figure) (Table). Among the 87 persons with camp-associated
cases, none reported symptom onset before the camp started
on June 13. Among the 35 persons with conference-associated
cases, three reported being symptomatic during the conference
(not including one camp-associated staff member who attended
the conference while symptomatic).
Among the 180 total persons with outbreak-associated cases,
13 (7.2%) required medical care in an emergency department,
and five (2.8%) were hospitalized; no deaths occurred (Table).
¶
Whole genome sequencing was performed on Illumina’s NextSeq 550
instrument using the COVID-Seq workflow. Consensus genome assembly
was performed in Illumina’s DRAGEN analytical pipeline, and variants were
assigned using the most recent Pangolin version.
** 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d);
5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
None of the vaccinated persons with cases were hospital-
ized; three sought care at an emergency department. Overall,
29 (16.1%) cases occurred in fully vaccinated persons (camp
cases: 9%; conference cases: 29%). Among the 262 close con-
tacts of persons with a primary case, 52 (20%) were fully vac-
cinated; 11 of these fully vaccinated persons received a positive
SARS-CoV-2 test result, representing 19% of the 58 secondary
cases among close contacts of camp or conference attendees
with primary cases.
Among the 122 cases in camp or conference attendees,
18 were in fully vaccinated persons (eight in camp attendees
and 10 in conference attendees). These 18 fully vaccinated per-
sons reported a total of 38 close contacts; eight (21%) of these
close contacts received positive SARS-CoV-2 test results, four
(50%) of whom were fully vaccinated. Among the 224 reported
close contacts of unvaccinated and partially vaccinated persons
with primary cases, 50 (22%) received positive SARS-CoV-2
test results, including seven fully vaccinated persons. Among
58 persons with secondary cases, 48 (83%) were infected by
household members, four by nonhousehold family members,
three by friends, and one each by a neighbor, at work, or dur-
ing a Bible study group.
Overall, 1,127 persons from at least four states and 18 coun-
ties were exposed to SARS-CoV-2 through attendance at the
camp or conference or through close contact with a person who
had a camp- or conference-associated case. In the 7 days before
the camp (June 6–12), Adams County, Illinois,
††
reported
31 COVID-19 cases, with an averageof4.4 cases per day. In
the 7 days after the last identified secondary case (July 16–22),
the county reported 232 cases, with an averageof33.1 per day,
a 648% increase from the number reported during the week
before the camp (2).
Among samples sequenced from specimens from 31 infected
persons (15 from camp-associated cases, eight from conference-
associated cases, and eight from secondary cases), the B.1.617.2
(Delta) variant was identified in 27 (87%), including two AY.3
(Delta) sequences; the B.1.1.7 (Alpha) variant was identified
in three (10%); and the P.1 (Gamma) variant was identified
in one (3%) (Table). Among eight sequenced samples from
specimens from vaccinated persons, the Delta variant was
identified in seven samples, and Alpha in one.
§§
††
Adams County is used as the reference county because it was the county of
residence for 49% (43) of persons with camp-associated cases, 40% (14) of
persons with conference-associated cases, and 59% (34) of persons with
secondary cases.
§§
Six of these eight vaccinated persons who were infected with SARS-CoV-2
variants of concern were from households with two persons with sequenced
samples; two pairs of the Delta variant and one discordant pair of Delta and
Alpha variants were identified in samples from these households.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1225
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE. Number of primary COVID-19 cases among attendees of a youth camp (A) and men’s conference (B) and secondary cases among close
contacts* (C), by date of symptom onset or specimen collection
†
— Illinois, June–July 2021
8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
Jun
Date of symptom onset or specimen collection
Jul
8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
Jun Jul
8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
Jun Jul
Start of men's conference:
June 18 (end date June 19)
Start of men's conference:
June 18 (end date June 19)
Start of men's conference:
June 18 (end date June 19)
Start of youth camp:
June 13
(end date June 17)
Start of youth camp:
June 13
(end date June 17)
A. Camp-associated primary cases
B. Conference-associated primary cases
Start of youth camp:
June 13
(end date June 17)
C. Secondary cases among close contacts
20
18
16
14
12
10
8
6
4
2
0
No. of cases
20
18
16
14
12
10
8
6
4
2
0
No. of cases
20
18
16
14
12
10
8
6
4
2
0
No. of cases
* Close contacts were defined as unmasked persons who were within 6 ft of a person with a camp-or conference-associated (primary) case for >15 minutes during a
24-hour period while that person was infectious (i.e., 2 days before through 10 days after symptom onset or specimen collection date). Secondary cases were defined
as COVID-19 cases in close contacts of persons with a primary case of confirmed or probable COVID-19 (confirmed: receipt of a positive SARS-CoV-2 nucleic acid
amplification test result in an attendee; probable: receipt of a positive SARS-CoV-2 antigen test result).
†
Symptom onset date or specimen collection date was missing for six out-of-state persons. Among the remaining 174, onset date was available for 158 (91%), and
specimen collection date was available for 16 (9%).

Morbidity and Mortality Weekly Report
1226 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
Public Health Response
IDPH sent three Epi-X notifications
¶¶
about these outbreaks
to state and local health departments and received case data from
the state health departments in Iowa, Michigan, and Missouri.
On June 30, IDPH requested CDC’s assistance with investigat-
ing these outbreaks. On July 19, a CDC field team arrived in
Illinois to assist with active case finding in several jurisdictions,
collection and analysis of samples, and ascertainment of second-
ary transmission. As of August 13, complete rosters of attendees
and staff members at both events were not available.
Discussion
COVID-19 vaccines currently authorized by the Food and
Drug Administration are safe and highly effective for prevent-
ing COVID-19–related serious illness, hospitalization, and
death.*** In this investigation, most reported COVID-19
cases were identified among unvaccinated persons. However,
transmission of SARS-CoV-2 from vaccinated persons both
to unvaccinated and vaccinated persons likely occurred. These
breakthrough cases among vaccinated persons were identified
among attendees of the camp and the conference and in persons
exposed to the attendees. Consistent with previous studies,
much of the identified secondary transmission occurred within
households, where most prolonged contact occurs (3).
Approximately 1,000 persons in at least four states were
exposed to SARS-CoV-2 through attendance at the camp or
conference or through close contact with a person infected at
the event. The high rate of transmission was likely driven by
the number of persons infected with the SARS-CoV-2 Delta
variant. However, because multiple SARS-CoV-2 variants of
concern were identified from the specimens of camp attendees,
this suggests multiple introductions of SARS-CoV-2 into the
camp, rather than a single introduction event. As of August 7,
COVID-19 outbreaks in at least 21 overnight camps had been
reported in Illinois, reinforcing the importance of COVID-19
prevention measures at these camps, including identifying
infected persons through prearrival and screening testing
programs and consistent implementation of other prevention
efforts, including vaccination, masking, and physical distanc-
ing (4–6). Several camp staff members who were infected with
SARS-CoV-2 (including at least one symptomatic person) or
who had been exposed to the virus attended another large
group event during their infectious period. Therefore, timely
¶¶
Epi-X is a secure, web-based notification system, with approximately 6,000
users from public health agencies, that guides and coordinates public health
professionals during public health threats and investigations. https://
emergency.cdc.gov/epix/index.asp
*** https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html
TABLE. Characteristics of persons with primary COVID-19 cases after
attendance at a youth camp or men’s conference and of close
contacts with secondary COVID-19 cases — Illinois, June–July 2021
Characteristic
No. (%)
Camp
cases
Conference
cases
Secondary
cases Total
Minimum no. of persons
exposed
335 530 262 1,127
Reported cases* 87 (26) 35 (7) 58 (22) 180 (16)
Median age, yrs (range)
†
17 (13–54) 44 (15–68) 38 (3–72) 26 (3–72)
Sex
†
Male 28 (34) 35 (100) 20 (34) 83 (47)
Female 55 (66) 0 (—) 38 (66) 93 (53)
Persons who required
emergency department
care
3 (3) 5 (14) 5 (9) 13 (7)
Persons hospitalized 1 (1) 3 (9) 1 (2) 5 (3)
Fully vaccinated
persons
§
8 (9) 10 (29) 11 (19) 29 (16)
Vaccine product received by fully vaccinated persons
Pfizer-BioNTech 3 (38) 5 (50) 3 (27) 11 (41)
Moderna 2 (25) 3 (30) 2 (18) 7 (24)
Janssen (Johnson &
Johnson)
3 (38) 2 (20) 6 (55) 11 (38)
Unknown vaccine
product received or
partially vaccinated
79 (91) 25 (71) 47 (81) 151 (84)
No. of viruses
sequenced
¶
15 8 8 31
B.1.617.2 (Delta) 13 (87) 7 (88) 7 (88) 27 (87)
B.1.1.7 (Alpha) 1 (7) 1 (13) 1 (13) 3 (10)
P.1 (Gamma) 1 (7) 0 (—) 0 (—) 1 (3)
Minimum no. of
affected counties**
16 7 8 18
* Percentages might not sum to 100% because of rounding.
†
For 174 of 180 cases in persons with a reported onset or specimen collection
date, sex (176), and date of birth.
§
Fully vaccinated persons were defined as persons who had received 2 doses
of Pfizer BioNTech or Moderna COVID-19 mRNA vaccine or 1 dose of Janssen
(Johnson & Johnson) COVID-19 vaccine ≥14 days before exposure.
¶
Illinois Department of Public Health laboratories performed whole genome
sequencing on 25 of 31 specimens using Illumina’s NextSeq 550 instrument
with the COVID-Seq workflow. Consensus genome assembly was performed
in Illumina’s DRAGEN analytical pipeline, and variants were assigned using
the most recent Pangolin version.
** Because seven of 16 counties of residence identified among camp and
conference attendees were outside of Illinois, contact tracing data were
extremely limited.
notification of all close contacts and compliance with isolation
and quarantine guidance are also critical.
The findings in this report are subject to at least two limita-
tions. First, the investigation likely underestimates the number
of SARS-CoV-2 primary infections, secondary exposures, and
secondary cases because the case definition required laboratory
confirmation; therefore, infected persons who did not receive
testing or who used at-home SARS-CoV-2 antigen tests (i.e.,
self-collection kits) were not included in the case count. In
addition, not all persons with cases participated in contact
tracing; the close contacts of persons who did participate were

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1227
US Department of Health and Human Services/Centers for Disease Control and Prevention
Summary
What is already known about this topic?
The Illinois Department of Public Health investigated COVID-19
outbreaks at two events sponsored by the same organization: a
5-day overnight church camp for persons aged 14–18 years and
a 2-day men’s conference.
What is added by this report?
Neither COVID-19 vaccination nor COVID-19 testing was
required before either event. Among 122 primary cases, 104
(85%) were in persons who were not fully vaccinated, and 18
(15%) were in fully vaccinated persons. Eight of 38 (21%) close
contacts of the 18 fully vaccinated persons subsequently
became infected with SARS-CoV-2. No vaccinated persons with
COVID-19 were hospitalized.
What are the implications for public health practice?
This investigation underscores the impact of secondary
SARS-CoV-2 transmission during large events such as camps
and conferences when COVID-19 prevention strategies,
including vaccination, masking, physical distancing, and
screening testing, are not implemented.
likely underreported and were biased toward household con-
tacts (7). Second, investigators did not have access to complete
rosters for the camp or conference, which limited case finding
efforts and analyses involving persons who were not infected
(particularly findings related to vaccination status).
These findings underscore the risk for COVID-19 outbreaks
at camps and large events where prevention strategies are not
implemented and highlight the importance of implement-
ing such strategies to reduce transmission of SARS-CoV-2
in these settings (8). Promoting vaccination, implementing
and encouraging compliance with prompt quarantine and
isolation measures for exposed and infected persons, staying
home when sick, and using nonpharmaceutical interventions
including masking, physical distancing, and screening testing
in large group settings can help reduce secondary infections
in homes and the community and serious complications from
COVID-19 (9).
Acknowledgments
Illinois Department of Public Health and local Illinois Health
Department staff members, health care providers, contact tracers,
and community health representatives; Blessings Hospital, Quincy,
Illinois; Iowa Department of Public Health; Michigan Department
of Health and Human Services; Missouri Department of Health and
Senior Services; Jerrod Welch, Emily Crabtree, Tara Bealor, Ellen
Vonderheide, Katie McConnell, Adams County Health Department;
CDC COVID-19 Response Team; CDC Health Department Task
Force Section.
Corresponding author: James Matthias, [email protected].
1
CDC COVID-19 Response Team;
2
Illinois Department of Public Health;
3
Adams County Health Department, Quincy, Illinois;
4
Schuyler County Health
Department, Rushville, Illinois;
5
Illinois Department of Public Health
Laboratory, Springfield, Illinois.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. No potential conflicts of interest were disclosed.
References
1. Griffin JB, Haddix M, Danza P, et al. SARS-CoV-2 infections and
hospitalizations among persons aged ≥16 years, by vaccination status—
Los Angeles County, California, May 1–July 25, 2021. MMWR Morb
Mortal Wkly Rep 2021;70:1170–6. PMID:34437525 https://doi.
org/10.15585/mmwr.mm7034e5
2. Adams County Health Department. Adams County, Illinois, COVID-19
tracking system. Quincy, IL: Adams County Health Department; 2021.
Accessed August 10, 2021. https://adamscountyilgis.maps.arcgis.com/
apps/dashboards/d8a330c2daa945fca0c8eedeb6e1c409
3. Luo L, Liu D, Liao X, et al. Contact settings and risk for transmission in
3410 close contacts of patients with COVID-19 in Guangzhou, China.
Ann Intern Med 2020;173:879–87. PMID:32790510 https://doi.
org/10.7326/M20-2671
4. Szablewski CM, Chang KT, Brown MM, et al. SARS-CoV-2 transmission
and infection among attendees of an overnight camp—Georgia, June
2020. MMWR Morb Mortal Wkly Rep 2020;69:1023–5.
PMID:32759921 https://doi.org/10.15585/mmwr.mm6931e1
5. CDC. Guidance for operating youth camps. Atlanta, GA: US Department
of Health and Human Services, CDC; 2021. Accessed August 10, 2021.
https://www.cdc.gov/coronavirus/2019-ncov/community/schools-
childcare/summer-camps.html
6. D’Agostino EM, Armstrong SC, Humphreys L, et al. Symptomatic
SARS-CoV-2 transmission in youth and staff attending day camps.
Pediatrics 2021;147:e2020042416. PMID:33536332 https://doi.
org/10.1542/peds.2020-042416
7. Cope AB, Bernstein K, Matthias J, et al. Unnamed partners from syphilis
partner services interviews, 7 jurisdictions. Sex Transm Dis 2020;47:811–8.
PMID:32890335 https://doi.org/10.1097/OLQ.0000000000001269
8. Carter RJ, Rose DA, Sabo RT, et al.; CDC COVID-19 Response
Team. Widespread severe acute respiratory syndrome coronavirus 2
transmission among attendees at a large motorcycle rally and their
contacts, 30 US jurisdictions, August–September, 2020. Clin Infect Dis
2021;73(Suppl 1):S106–9. PMID:33912907 https://doi.org/10.1093/
cid/ciab321
9. CDC. Science brief: transmission of SARS-CoV-2 in K–12 schools and
early care and education programs. Atlanta, GA: US Department of Health
and Human Services, CDC; 2021. Accessed August 10, 2021. https://
www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/
transmission_k_12_schools.html

Morbidity and Mortality Weekly Report
1228 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
Association Between COVID-19 and Myocarditis Using Hospital-Based
Administrative Data — United States, March 2020–January 2021
Tegan K. Boehmer, PhD
1,
*; Lyudmyla Kompaniyets, PhD
1,
*; Amy M. Lavery, PhD
1
; Joy Hsu, MD
1
; Jean Y. Ko, PhD
1
; Hussain Yusuf, MD
1
;
Sebastian D. Romano, MPH
1
; Adi V. Gundlapalli, MD, PhD
1
; Matthew E. Oster, MD
1,2,3
; Aaron M. Harris, MD
1
On August 31, 2021, this report was posted as an MMWR Early
Release on the MMWR website (https://www.cdc.gov/mmwr).
Viral infections are a common cause of myocarditis, an
inflammation of the heart muscle (myocardium) that can
result in hospitalization, heart failure, and sudden death (1).
Emerging data suggest an association between COVID-19
and myocarditis (2–5). CDC assessed this association using
a large, U.S. hospital-based administrative database of health
care encounters from >900 hospitals. Myocarditis inpatient
encounters were 42.3% higher in 2020 than in 2019. During
March 2020–January 2021, the period that coincided with the
COVID-19 pandemic, the risk for myocarditis was 0.146%
among patients diagnosed with COVID-19 during an inpa-
tient or hospital-based outpatient encounter and 0.009%
among patients who were not diagnosed with COVID-19.
After adjusting for patient and hospital characteristics, patients
with COVID-19 during March 2020–January 2021 had,
on average, 15.7 times the risk for myocarditis compared
with those without COVID-19 (95% confidence interval
[CI]=14.1–17.2); by age, risk ratios ranged from approxi-
mately 7.0 for patients aged 16–39 years to >30.0 for patients
aged <16 years or ≥75 years. Overall, myocarditis was uncom-
mon among persons with and without COVID-19; however,
COVID-19 was significantly associated with an increased risk
for myocarditis, with risk varying by age group. These findings
underscore the importance of implementing evidence-based
COVID-19 prevention strategies, including vaccination, to
reduce the public health impact of COVID-19 and its associ-
ated complications.
Data for this study were obtained from the Premier
Healthcare Database Special COVID-19 Release (PHD-SR),
a large hospital-based administrative database.
†
The monthly
* These authors contributed equally to this report.
†
PHD-SR, formerly known as the PHD COVID-19 Database, is a large U.S.
hospital-based all-payer database that includes inpatient and hospital-based
outpatient (e.g., emergency department or clinic) health care encounters from
>900 geographically diverse, nonprofit, nongovernmental, community, and
teaching hospitals and health systems from rural and urban areas. PHD-SR
represents approximately 20% of inpatient admissions in the United States.
Updated PHD-SR data are released every 2 weeks; release date August 4, 2021,
access date August 4, 2021. http://offers.premierinc.com/rs/381-NBB-525/
images/PHD_COVID-19_White_Paper.pdf
number of myocarditis
§
and COVID-19
¶
inpatient encounters
was assessed before and during the COVID-19 pandemic, from
January 2019 through May 2021.
A patient-level cohort was created to assess the association
between COVID-19 and myocarditis. The cohort included all
patients with at least one inpatient or hospital-based outpatient
encounter with discharge during March 2020–January 2021.
To minimize potential bias from vaccine-associated myocarditis
(6), 277,892 patients with a COVID-19 vaccination record
in PHD-SR during December 2020–February 2021 were
excluded. In addition, 37,896 patients for whom information
on sex was missing were excluded. Patients with COVID-19
were defined as those who had their first inpatient or outpatient
encounter with a COVID-19 International Classification of
Diseases, Tenth Revision, Clinical Modification (ICD-10-CM)
code during March 2020–January 2021. Patients with myo-
carditis were defined as those who had their first of at least
one inpatient encounter, at least two outpatient encounters,
or at least one outpatient encounter with a relevant specialist**
with a myocarditis ICD-10-CM code during March 2020–
February 2021.
††
Among patients with COVID-19, the first
myocarditis encounter could have occurred during or after the
first COVID-19 health care encounter.
The risk for myocarditis was defined as the percentage of
patients with myocarditis and was calculated among patients
with and without COVID-19, overall and by sex (male or
§
Myocarditis was identified by the following International Classification of
Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes: B33.20,
B33.22, B33.24, I40.0, I40.1, I40.8, I40.9, or I51.4.
¶
COVID-19 was identified by ICD-10-CM code B97.29 (other coronavirus
as the cause of diseases classified elsewhere) during March–April 2020 or
ICD-10-CM code U07.1 (COVID-19, virus identified [laboratory-
confirmed]) during or after April 2020. ICD-10-CM code B97.29 was
recommended before the April 1, 2020, release of ICD-10-CM code U07.1.
https://www.cdc.gov/nchs/data/icd/Announcement-New-ICD-code-for-
coronavirus-3-18-2020.pdf
** Attending physician with one of the following specializations: cardiac
electrophysiology, cardiovascular diseases, cardiovascular surgery, infectious
diseases, or rheumatology.
††
Myocarditis was assessed using all encounters for each patient from January
2019 to February 2021. Patients were defined as having new myocarditis
during the study period if their first myocarditis encounter in PHD-SR
occurred during or after March 2020. Myocarditis was assessed through
February 2021 to allow for myocarditis diagnoses to occur after COVID-19
diagnoses in January 2021.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1229
US Department of Health and Human Services/Centers for Disease Control and Prevention
female) and age group (<16, 16–24, 25–39, 40–49, 50–64,
65–74, and ≥75 years). The percentage of myocarditis patients
with a history of COVID-19 was calculated for each age group.
Associations between COVID-19 and myocarditis were
estimated using a multiple logit model with the following
covariates: three-way interaction between COVID-19, sex, and
age group, including lower-order interactions and main effects;
race/ethnicity; payer type; hospital U.S. Census region; and
hospital urbanicity. Adjusted risk differences (aRDs, measure
of absolute risk) were calculated as the difference between
1) the adjusted predicted risk for myocarditis (outcome) among
patients with COVID-19 (exposed group) and 2) adjusted pre-
dicted risk for myocarditis among patients without COVID-19
(unexposed group); adjusted risk ratios (aRRs, measure of
relative risk) were calculated as the ratio of the adjusted
predicted risk among exposed to the adjusted predicted risk
among unexposed
§§
(7,8). All models used standard errors
clustered on a unique hospital identifier. R (version 4.0.2;
R Foundation) and Stata (version 15.1; StataCorp) were used
to conduct all analyses. This activity was reviewed by CDC
and was conducted consistent with applicable federal law and
CDC policy.
¶¶
During 2020, the number of myocarditis inpatient encoun-
ters (4,560) was 42.3% higher than that during 2019 (3,205).
Peaks in myocarditis inpatient encounters during April–
May 2020 and November 2020–January 2021 generally aligned
with peaks in COVID-19 inpatient encounters (Figure 1).
Within the cohort of 36,005,294 patients, 1,452,773
(4.0%) received a diagnosis of COVID-19 during
March 2020–January 2021, and 5,069 (0.01%) received a diag-
nosis of myocarditis during March 2020–February 2021. Overall,
4,339 (85.6%) patients with myocarditis were identified by an
inpatient encounter. Patients with myocarditis were slightly older
than patients without myocarditis (median age=54 years versus
50 years) and were more commonly male (59.3% versus 41.7%)
(Supplementary Table, https://stacks.cdc.gov/view/cdc/109261).
§§
First, a multiple logit model was performed with the following covariates:
three-way interaction between COVID-19, sex, and age group, including
lower-order interactions and main effects; race/ethnicity; payer type; hospital
U.S. Census region; and hospital urbanicity. Then the following average
predicted probabilities (predictive margins) were estimated: 1) P1: the average
predicted probability of myocarditis with COVID-19 set to be present and
all other covariates set to their original values, and 2) P0: the average predicted
probability of myocarditis with COVID-19 set to be absent and all other
covariates set to their original values. aRD represents the difference in predicted
probabilities (P1 minus P0); aRR represents the ratio of the predicted
probabilities (P1 divided by P0). aRRs and aRDs were obtained for the full
sample (where all covariates were set at their original values), for each age
group (where age was set at the specific category of interest and other covariates
were set at their original values), and for each sex (where sex was set at the
specific category of interest and other covariates were set at their original values).
¶¶
45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C.
Sect. 552a; 44 U.S.C. Sect. Sect. 3501 et seq.
Among patients with myocarditis, 2,116 (41.7%) had a
history of COVID-19; this percentage was similar among
males (42.4%) and females (40.9%) and differed by age
group, with the lowest percentages among persons aged
16–24 years (23.7%) and 25–39 years (24.1%) and the high-
est among adults aged ≥75 years (64.6%) (Table). Among
the 2,116 patients with COVID-19 and myocarditis, 1,895
(89.6%) received a diagnosis of COVID-19 and myocarditis
during the same month; the remaining patients received a
myocarditis diagnosis 1 month (139; 6.6%) or ≥2 months
(82; 3.9%) after their COVID-19 diagnosis.
During March 2020–January 2021, the risk for myocarditis
was 0.146% among patients with COVID-19 and 0.009%
among patients without COVID-19. Among patients with
COVID-19, the risk for myocarditis was higher among
males (0.187%) than among females (0.109%) and was
highest among adults aged ≥75 years (0.238%), 65–74 years
(0.186%), and 50–64 years (0.155%) and among children
aged <16 years (0.133%).
In adjusted analyses, patients with COVID-19 had, on
average, 15.7 (95% CI=14.1–17.2) times the risk for myo-
carditis compared with patients without COVID-19; however,
because of the low risk for myocarditis in both groups, the
aRD between patients with and without COVID-19 was
small (aRD
= 0.126%; 95% CI = 0.112%–0.140%)
(
Table) (Figure 2). The aRR of myocarditis was higher among
females (17.8; 95% CI=15.6–20.0) than among males (13.8;
95% CI=12.3–15.3), whereas the aRD was higher among
males (0.165%; 95% CI= 0.146%–0.183%) than among
females (0.100%; 95% CI=0.087%–0.113%). The aRR and
aRD were lowest for patients aged 25–39 years and were higher
among younger and older age groups. The aRRs ranged from
approximately 7.0 for patients aged 16–24 and 25–39 years
to >30.0 for patients aged <16 years and ≥75 years.
Discussion
In this study, the occurrence of myocarditis inpatient
encounters was 42% higher in 2020 than in 2019. The risk
for myocarditis among patients with COVID-19 during
March 2020–January 2021 was nearly 16 times as high as the
risk among patients without COVID-19, with the association
between COVID-19 and myocarditis being most pronounced
among children and older adults. Further, in this cohort,
approximately 40% of patients with myocarditis had a history
of COVID-19.
These findings suggest an association between COVID-19
and myocarditis, although causality cannot be inferred from
observational data, and are consistent with those from previ-
ous studies (2–5). Before this report, the two largest known
studies, in the United States and in Israel, also found that

Morbidity and Mortality Weekly Report
1230 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 1. Number of myocarditis and COVID-19 inpatient encounters, by month* — Premier Healthcare Database Special COVID-19 Release,
United States, January 2019–May 2021
No. of COVID-19 inpatient encounters
No. of myocarditis inpatient encounters
0
20,000
40,000
60,000
80,000
100,000
120,000
0
50
100
150
200
250
300
350
400
450
500
No. of myocarditis inpatient encounters
No. of COVID-19 inpatient encounters
550
600
Jan Mar May Jul Sep Nov Jan Mar May Jul Sep Nov Jan Mar May
2019 2020 2021
Month and year
* Data from recent months mightbe incomplete.
TABLE. Frequency of and risk for myocarditis among patients with and without COVID-19 and adjusted* myocarditis risk differences and risk ratios
comparing patients with and without COVID-19 — Premier Healthcare Database Special COVID-19 Release, United States, March 2020–January 2021
Characteristic
No. of
patients
with
COVID-19
No. of
patients
without
COVID-19
No. of
patients
with
myocarditis
Myocarditis among
patients
with COVID-19
Myocarditis among
patients
without COVID-19
Adjusted
myocarditis
risk dierence
(95% CI)
Adjusted
myocarditis
risk ratio
(95% CI)
No. (% of
patients with
myocarditis) Risk, %
No. (% of
patients with
myocarditis) Risk, %
Overall 1,452,773 34,552,521 5,069 2,116 (41.7) 0.146 2,953 (58.3) 0.009 0.126 (0.112–0.140) 15.7 (14.1–17.2)
Sex
Male 680,722 14,339,356 3,008 1,274 (42.4) 0.187 1,734 (57.6) 0.012 0.165 (0.146–0.183) 13.8 (12.3–15.3)
Female 772,051 20,213,165 2,061 842 (40.9) 0.109 1,219 (59.1) 0.006 0.100 (0.087–0.113) 17.8 (15.6–20.0)
Age group, yrs
<16 64,898 3,670,762 218 86 (39.4) 0.133 132 (60.6) 0.004 0.122 (0.065–0.179) 36.8 (25.0–48.6)
16–24 123,865 3,067,575 511 121 (23.7) 0.098 390 (76.3) 0.013 0.088 (0.061–0.115) 7.4 (5.5–9.2)
25–39 268,549 6,246,568 862 208 (24.1) 0.077 654 (75.9) 0.010 0.067 (0.052–0.081) 6.7 (5.5–8.0)
40–49 198,561 4,147,909 620 213 (34.4) 0.107 407 (65.6) 0.010 0.093 (0.078–0.109) 10.0 (8.1–11.9)
50–64 356,697 7,965,264 1,226 553 (45.1) 0.155 673 (54.9) 0.008 0.137 (0.121–0.154) 17.0 (14.7–19.3)
65–74 214,331 5,318,474 801 398 (49.7) 0.186 403 (50.3) 0.008 0.160 (0.135–0.184) 23.0 (19.4–26.7)
≥75 225,872 4,135,969 831 537 (64.6) 0.238 294 (35.4) 0.007 0.208 (0.179–0.237) 31.6 (25.9–37.2)
Abbreviation: CI=confidence interval.
* Adjusted risk differences and risk ratios for myocarditis during or after COVID-19 (reference group: no COVID-19), obtained from a single logit model with the
following covariates: a three-way interaction between presence of COVID-19, sex, and age group, including lower-order interactions and main effects; race/ethnicity;
payer type; hospital U.S. Census region; and hospital urbanicity.

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1231
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE 2. Adjusted risk ratio (A) and adjusted risk difference (B) of myocarditis comparing
patients with and without COVID-19,
* overall and by sex and age group — Premier
Healthcare Database Special COVID-19 Release, United States, March 2020–January 2021
0.5 1.0 2.0 8.0 16.0
32.0
4.0
Risk ratio
A
B
Overall
Sex
Male
Female
Age group, yrs
<16
16–24
25–39
40–49
50–64
65–74
≥75
Overall
Sex
Male
Female
Age group, yrs
<16
16–24
25–39
40–49
50–64
65–74
≥75
-0.1
0.0 0.2
0.3
0.1
Risk dierence (%)
* The panels show adjusted risk ratios (A) and adjusted risk differences (B) of myocarditis comparing
patients with COVID-19 to patients without COVID-19 (reference), obtained from a single logit model
with the following covariates: a three-way interaction between presence of COVID-19, sex, and age
group, including lower-order interactions and main effects; race/ethnicity; payer type; hospital U.S.
Census region; and hospital urbanicity. 95% confidence intervals indicated by error bars.
COVID-19 was strongly associated with myocarditis (U.S.
study: odds ratio=8.17, 95% CI=3.58–18.62; Israel study:
risk ratio=18.28, 95% CI=3.95–25.12) (3,4).
In this study, the association between COVID-19 and myo-
carditis was lowest for persons aged 25–39 years and higher
among younger (<16 years) and older (≥50 years) age groups, a
pattern that has not been previously described in age-stratified
analyses and that warrants further investigation. This find-
ing might be partially explained by age-related differences in
COVID-19 case ascertainment, because younger adults with
less severe disease might be less likely than older adults to have
a health care encounter with a COVID-19
diagnosis captured within PHD-SR. This age-
related differential misclassification (underas-
certainment) of COVID-19 status might bias
risk differences and risk ratios toward the null
more for younger adults and could partially
explain the observed age-related association.
The risk difference for myocarditis between
persons with and without COVID-19 was
higher among males than among females,
consistent with some earlier studies (2,5). The
finding of a higher risk ratio among females
than among males is novel. However, it likely
reflects the low risk for myocarditis among
female patients without COVID-19 (5).
Although the exact mechanism of
SARS-CoV-2 infection possibly leading to
myocarditis is unknown, the pathophysiol-
ogy is likely similar to that of other viruses
(1). Among persons with COVID-19 and
myocarditis, some myocarditis diagnoses
might represent cases of multisystem inflam-
matory syndrome (MIS), particularly among
children aged <16 years (9). Further study
is warranted to understand how the clinical
course of myocarditis among patients with
COVID-19 might differ by presence or
absence of MIS (10).
Since the introduction of mRNA COVID-19
vaccines in the United States in December
2020, an elevated risk for myocarditis among
mRNA COVID-19 vaccine recipients has
been observed, particularly among males
aged 12–29 years, with 39–47 expected
cases of myocarditis, pericarditis, and myo-
pericarditis per million second mRNA
COVID-19 vaccine doses administered (6).
A recent study from Israel reported that
mRNA COVID-19 vaccination was associ-
ated with an elevated risk for myocarditis
(risk ratio = 3.24; 95% CI = 1.55–12.44); in the same study,
a separate analysis showed that SARS-CoV-2 infection
was a strong risk factor for myocarditis (risk ratio = 18.28,
95% CI = 3.95–25.12) (4). On June 23, 2021, the Advisory
Committee on Immunization Practices concluded that the
benefits of COVID-19 vaccination clearly outweighed the
risks for myocarditis after vaccination (6). The present study
supports this recommendation by providing evidence of an
elevated risk for myocarditis among persons of all ages with
diagnosed COVID-19.

Morbidity and Mortality Weekly Report
1232 MMWR / September 3, 2021 / Vol. 70 / No. 35 US Department of Health and Human Services/Centers for Disease Control and Prevention
The findings in this study are subject to at least six limita-
tions. First, the risk estimates from this study reflect the risk
for myocarditis among persons who received a diagnosis of
COVID-19 during an outpatient or inpatient health care
encounter and do not reflect the risk among all persons who
had COVID-19. Second, misclassification of COVID-19 and
myocarditis is possible because conditions were determined
by ICD-10-CM codes, which were not confirmed by clinical
data (e.g., laboratory tests or cardiac imaging) and could be
improperly coded or coded with a related condition (e.g., peri-
carditis). Third, encounters for COVID-19, myocarditis, and
COVID-19 vaccination occurring outside of hospital systems
that contribute to PHD-SR are not included within this data
set. Fourth, underlying medical conditions and alternative
etiologies for myocarditis (e.g., autoimmune disease) were not
ascertained or excluded. Fifth, the obtained measures of associa-
tion could be biased because of the choice of the comparison
group (all patients without COVID-19) and if physicians were
more likely to suspect or diagnose myocarditis among patients
with COVID-19. Finally, the findings represent a convenience
sample of patients from hospitals reporting to PHD-SR and
might not be generalizable to the U.S. population.
Myocarditis is uncommon among patients with and without
COVID-19; however, COVID-19 is a strong and significant
risk factor for myocarditis, with risk varying by age group. The
findings in this report underscore the importance of imple-
menting evidence-based COVID-19 prevention strategies,
including vaccination, to reduce the public health impact of
COVID-19 and its associated complications.
Acknowledgments
Matthew Ritchey, Paula Yoon, Min Levine, Data, Analytics, and
Visualization Task Force, CDC COVID-19 Response Team; John Su,
Vaccine Task Force, CDC COVID-19 Response Team; Jason Block,
Department of Population Medicine, Harvard Pilgrim Health Care
Institute, Harvard Medical School.
Corresponding author: Tegan Boehmer, [email protected].
1
CDC COVID-19 Response Team;
2
Emory University School of Medicine,
Atlanta, Georgia;
3
Children’s Healthcare of Atlanta, Atlanta, Georgia.
All authors have completed and submitted the International
Committee of Medical Journal Editors form for disclosure of potential
conflicts of interest. No potential conflicts of interest were disclosed.
Summary
What is already known about this topic?
Viral infections are a common cause of myocarditis. Some
studies have indicated an association between COVID-19
and myocarditis.
What is added by this report?
During March 2020–January 2021, patients with COVID-19 had
nearly 16 times the risk for myocarditis compared with patients
who did not have COVID-19, and risk varied by sex and age.
What are the implications for public health practice?
These findings underscore the importance of implementing
evidence-based COVID-19 prevention strategies, including
vaccination, to reduce the public health impact of COVID-19
and its associated complications.
References
1. Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis—
diagnosis, treatment options, and current controversies. Nat Rev Cardiol
2015;12:670–80. PMID:26194549 https://doi.org/10.1038/
nrcardio.2015.108
2. Rathore SS, Rojas GA, Sondhi M, et al. Myocarditis associated with
Covid-19 disease: a systematic review of published case reports and case
series. Int J Clin Pract 2021;e14470. Epub July 7, 2021. PMID:34235815
3. Murk W, Gierada M, Fralick M, Weckstein A, Klesh R, Rassen JA.
Diagnosis-wide analysis of COVID-19 complications: an exposure-
crossover study. CMAJ 2021;193:E10–8. PMID:33293424 https://doi.
org/10.1503/cmaj.201686
4. Barda N, Dagan N, Ben-Shlomo Y, et al. Safety of the BNT162b2
mRNA COVID-19 vaccine in a nationwide setting. N Engl J Med 2021.
Epub August 25, 2021. PMID:34432976 https://doi.org/10.1056/
NEJMoa2110475
5. Daugherty SE, Guo Y, Heath K, et al. Risk of clinical sequelae after the
acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ
2021;373:n1098. PMID:34011492 https://doi.org/10.1136/bmj.n1098
6. Gargano JW, Wallace M, Hadler SC, et al. Use of mRNA COVID-19
vaccine after reports of myocarditis among vaccine recipients: update
from the Advisory Committee on Immunization Practices—United
States, June 2021. MMWR Morb Mortal Wkly Rep 2021;70:977–82.
PMID:34237049 https://doi.org/10.15585/mmwr.mm7027e2
7. Kleinman LC, Norton EC. What’s the risk? A simple approach for
estimating adjusted risk measures from nonlinear models including
logistic regression. Health Serv Res 2009;44:288–302. PMID:18793213
https://doi.org/10.1111/j.1475-6773.2008.00900.x
8. Norton EC, Miller MM, Kleinman LC. Computing adjusted risk ratios
and risk differences in Stata. Stata J 2013;13:492–509. https://doi.
org/10.1177/1536867X1301300304
9. Most ZM, Hendren N, Drazner MH, Perl TM. Striking similarities of
multisystem inflammatory syndrome in children and a myocarditis-like
syndrome in adults. Circulation 2021;143:4–6. PMID:32787714
https://doi.org/10.1161/CIRCULATIONAHA.120.050166
10. Vukomanovic VA, Krasic S, Prijic S, et al. Differences between pediatric
acute myocarditis related and unrelated to SARS-CoV-2. Pediatr Infect
Dis J 2021;40:e173–8. PMID:33847291 https://doi.org/10.1097/
INF.0000000000003094

Morbidity and Mortality Weekly Report
MMWR / September 3, 2021 / Vol. 70 / No. 35 1233
US Department of Health and Human Services/Centers for Disease Control and Prevention
QuickStats
FROM THE NATIONAL CENTER FOR HEALTH STATISTICS
Death Rates* from Colorectal Cancer,
†
by Age Group —
United States, 1999–2019
0
20
40
60
80
100
120
140
160
1999
2000
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
Deaths per 100,000 population
Year
45–54 yrs 55–64 yrs 65–74 yrs 75–84 yrs
* Deaths per 100,000 population in each age group.
†
Deaths from colorectal cancer were identified using International Classification of Diseases, Tenth Revision
underlying cause-of-death codes C18–21.
During 1999–2019, deaths per 100,000 persons from colorectal cancer decreased among persons aged 55–64 years (from 33.5
to 24.4), persons aged 65–74 years (from 77.4 to 41.5), and persons aged 75–84 years (from 146.7 to 77.9). The death rate from
colorectal cancer among persons aged 45–54 years generally increased from 1999 (11.1) to 2019 (12.0). In each year during
1999–2019, the death rate was highest among persons aged 75–84 years and lowest among persons aged 45–54 years.
Source: National Center for Health Statistics, National Vital Statistics System, Mortality Data, 1999–2019. https://www.cdc.gov/nchs/nvss/deaths.htm
Reported by: Sibeso N. Joyner, MPH, [email protected], 301-458-4254; Deepthi Kandi, MS.

Morbidity and Mortality Weekly Report
ISSN: 0149-2195 (Print)
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free
of charge in electronic format. To receive an electronic copy each week, visit MMWR at https://www.cdc.gov/mmwr/index.html.
Readers who have difficulty accessing this PDF file may access the HTML file at https://www.cdc.gov/mmwr/index2021.html. Address all inquiries about
the MMWR Series to Editor-in-Chief, MMWR Series, Mailstop V25-5, CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30329-4027 or to mmwr[email protected].
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations
or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of these sites. URL addresses
listed in MMWR were current as of the date of publication.
