This information leaflet explains how to hand express colostrum while
you are pregnant and the benefits for your baby. If you have any
questions or concerns, please do not hesitate to speak to your midwife
or infant feeding team.
Antenatal colostrum
harvesting
www.kch.nhs.uk
Confirming your identity
Before you have a treatment or procedure, our staff will ask you your
name and date of birth and check your ID band. If you don’t have
an ID band we will also ask you to confirm your address.
If we don’t ask these questions, then please ask us to check.

2
What is colostrum?
It is the first milk you produce, usually from about 16 weeks of
pregnancy. Colostrum may leak from your breasts during pregnancy.
Colostrum is perfectly balanced for all your baby’s needs. It contains
antibodies to protect your baby from infections and hormones to
help gut growth and kick start their immune system. It also helps
them pass their first dark poo (meconium) which can reduce the risk
of jaundice.
What is antenatal colostrum harvesting?
It is the expressing and collection of your first milk – colostrum –
during pregnancy and helps get breastfeeding off to a good start. If
your baby requires extra milk you can use your harvested colostrum
instead of artificial milk.
When should I start colostrum harvesting?
We recommend you start colostrum harvesting from 36 weeks
of pregnancy. It is unlikely to trigger labour but please check the
‘reasons why I should not hand express colostrum before birth’
information in this leaflet prior to commencing. If while expressing
you have any painful contractions, you should stop expressing and
call your midwife or the Maternity Telephone Assessment Line for
advice.
Denmark Hill Telephone Assessment Line: 020 3299 8389
Princess Royal University Hospital Assessment Line: 01689 864189

3
Why should I express colostrum before I have had
my baby?
Learning how to express milk while you are pregnant helps you
to get to know your breasts and how they work, giving you extra
confidence to start breastfeeding. It is useful if you are unable to
feed your baby straight after birth for whatever reason, ensuring
they get the protection needed for life outside the womb.
Expressing colostrum can also help if you:
• have pre-existing diabetes or develop diabetes while you are
pregnant (gestational diabetes)
• have breast hypoplasia (underdeveloped milk-producing breast
tissue)
• have multiple sclerosis
• are having a planned (elective) caesarean section
• have a history of breast surgery
• have taken certain medications during pregnancy for high blood
pressure. Your doctor or midwife will advise if this applies to you.
• have had problems with breastfeeding after previous births
• have a strong family history of dairy intolerance
• have a strong family history of inflammatory bowel disease (IBD)
• are having more than one baby
• have a body mass index (BMI) score of 35 or above
• have a hormonal disorder such as polycystic ovary syndrome
(PCOS).
In addition, it can be of benefit to your baby to collect and feed
them your colostrum if:
• scans show they are small for their gestational age
• they have been diagnosed with fetal cleft palate/lip
• they are going to have a planned admission to the neonatal ward
after birth
• they have any congenital conditions.

4
Are there any reasons why I should not express
colostrum before birth?
Do not express colostrum while pregnant if you:
• have a history of threatened and/or actual premature labour
• have a cervical suture (stitch) in place
• are taking a drug that may be harmful for your baby to have
through your breast milk. For more information you can
contact the Drugs in Breastmilk information service through its
Facebook page – BfNDrugsinBreastmilkinformation – or email
• have placenta praevia, accreta, percreta, placental site unknown in
absence of USS, vasa praevia and/or low-lying placenta.
There may be other reasons why you should not express colostrum
before you have had your baby, so please discuss this with your
midwife and obstetrician.
How do I hand express colostrum?
Wash your hands with soap and water, then dry them with a clean
towel. Next, make sure you have a sterile container, such as a
syringe, to collect the colostrum.
Make sure you are relaxed and comfortable. Try looking at a
picture of your scan, talk to your baby or touch your bump to feel
connected to your baby. It might take a while for the colostrum to
appear when you start. Be patient and relax – it can take several
goes and it’s normal to see a small amount.
1. Gently massage your breast from the outer
parts towards your nipple in all directions (for
about two minutes). Then roll or tweak your
nipple (for about one minute). This stimulates
oxytocin which is your milk release hormone.

5
2. Position your thumb and your fingers in
a ‘C’ shape. Start at the end of your nipple
and feel back to where there is a texture
change, usually about 2 – 3cm from your
nipple.
3. Gently but firmly compress and release
your finger and thumb in a rhythmic motion.
Do not slide your fingers over your skin or
nipple. Expressing should not hurt. It may
take a few minutes before you see any
colostrum. Collect your colostrum in a sterile
syringe.
4. When the flow slows down or stops,
change the position of the ‘C’ shape so that
you move around your breast. You can move
to your other breast and repeat.
5. When you have finished, label your colostrum with your full
name, hospital number, date of birth and the date and time you
expressed it. Then store it following the guidelines in the ‘Safe
storage of colostrum table’ on page 6.
How often should I hand express?
It is up you. You can express as little as twice a day or as much as
8 times a day. For example, you could start hand expressing twice
a day, for 10 minutes, from 36 weeks increasing the frequency
gradually to a maximum of 8 times a day if you choose. Just
remember to do what feels comfortable for you.
6
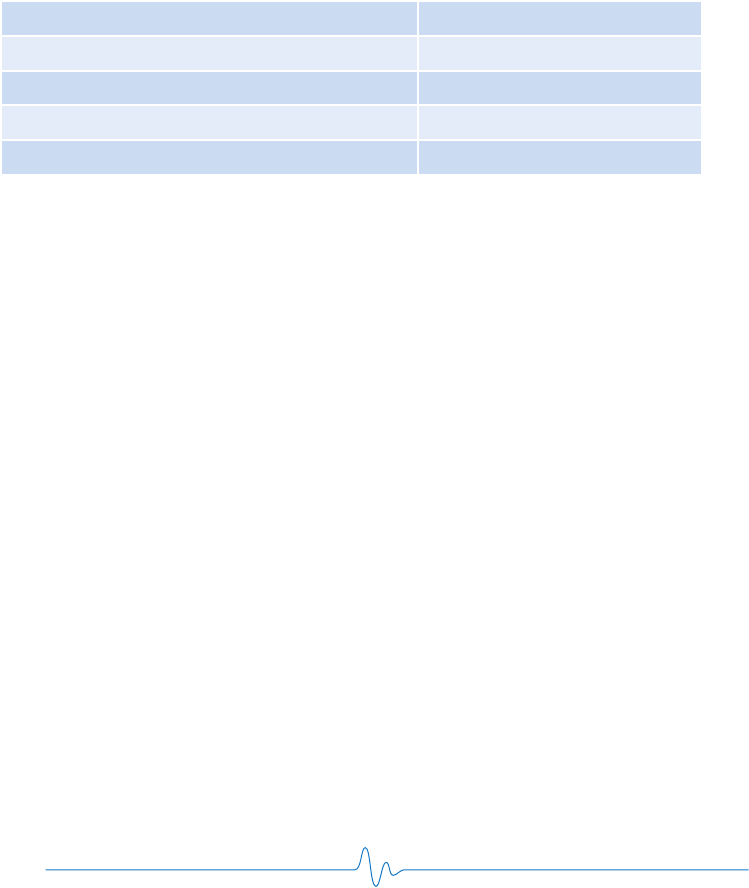
Safe storage of milk at home
This table shows the recommended maximum safe storage times for
your colostrum whilst you are at home. In hospital these times will
change. Do not forget to note on the container the date and time
you express the milk.
Storing your milk at home
Milk can also be frozen in the ice compartment but only for 2 weeks
(Off to the Best Start, 2015).
Milk stored at home should be kept away from meat products, eggs
or any uncooked food. It should be kept in the back of the fridge
and not in the door.
What is the best way of bringing my colostrum into
hospital with me?
When you transport your colostrum into hospital put your colostrum
into an insulated cool bag and fill the space with ice packs, this will
maintain the temperature. Defrosted milk cannot be refrozen. You
can also leave your colostrum at home and bring it into hospital
when needed so it does not exceed the recommended storage
times. When you get to hospital, let your midwife know you have
brought your first milk with you and they will put it in the fridge
or freezer. You need to make sure it is labelled with your name,
Room temperature 6 hours
Fridge 5-10 degrees 3 days
Fridge 4 degrees and lower 5 days
Freezer minus 18 degrees and lower 6 months
Defrosted Use straight away.
The Breastfeeding Network, 2019

7
hospital number, date of birth and time and date expressed. After
your baby is born, the midwife will show you how to safely give
your first milk to your baby.
Storing your milk in hospital
The storage times are different in hospital from at home so please
speak to your midwife.
Using your colostrum
When you are ready to use your colostrum the midwife will show
you where it is, how to defrost and how to safely give it to your
baby. Please check the label for your name, hospital number and
date of birth to ensure it is your milk.
How do I hand express?
Scan this QR code to watch the UNICEF video on
hand expressing or visit (https://www.unicef.org.uk/
babyfriendly/baby-friendly-resources/breastfeeding-
resources/hand-expression-video/)
This video is a demonstration of technique, the amount of colostrum
is not reflective of what you may find in the antenatal period. It is
normal to see small amounts or can be none at all.
More information
If you would like any more information on feeding and caring for
your baby visit www.unicef.org.uk/babyfriendly
www.breastfeedingnetwork.org.uk www.laleche.org.uk

PALS
The Patient Advice and Liaison Service (PALS) is a service that offers
support, information and assistance to patients, relatives and visitors.
They can also provide help and advice if you have a concern or
complaint that staff have not been able to resolve for you.
PALS at King’s College Hospital, Denmark Hill, London SE5 9RS:
Tel: 020 3299 3601 Email: kch-tr[email protected]
You can also contact us by using our online form at
www.kch.nhs.uk/contact/pals
PALS at Princess Royal University Hospital, Farnborough Common,
Orpington, Kent BR6 8ND
Tel: 01689 863252 Email: kch-tr[email protected]
If you would like the information in this leaflet in a different
language or format, please contact PALS on 020 3299 1844.
PL969.1 June 2022 Urgent & Planned Care
Review date June 2025 Corporate Comms: 2640
Infant feeding sessions – available from 34 weeks
Denmark Hill
Sign up to Infant Feeding on Eventbrite:
http://kchparenteducation.eventbrite.com
Princess Royal University Hospital: Sign up to Infant Feeding
on Eventbrite: www.eventbrite.co.uk/e/pruh-infant-feeding-
tickets-146566250601
Phone helpline: 07866 927594, 7am – 7pm everyday, including bank
holidays.
