Association of Women Surgeons
Pocket Mentor
A Manual for Surgeons in Training
and Medical Students
Fifth Edition
2013
Association of Women Surgeons
E-mail: [email protected]
Website: www.WomenSurgeons.org
1
POCKET MENTOR
Fifth Edition
Annesley Copeland MD, FACS
This edition was prepared with
input from many individuals.
Special thanks to the AWS Resident
and Medical Student Committees for
their thoughtful insights and contributions.
Fourth Edition
Mary Hooks MD, MBA, FACS
Third Edition
Danielle Walsh MD, FACS
First and Second Editions
Joyce Majure MD, FACS
Published by the
Association of Women Surgeons
WomenSurgeons.org
© 2013 The Association of Women Surgeons. All rights reserved. This book and all its contents are protected by
copyright. No part of it may be reproduced, stored in a retrieval system, or transmitted in any form or by any
means, electronic, mechanical, photocopying, recording or otherwise, without written permission from the publisher.
Made in the United States of America.
2
The Association of Women Surgeons, founded in 1981, is an organization whose
mission is to inspire, encourage, and enable women surgeons to realize their
professional and personal goals. This publication represents two of our goals:
advancing
the highest standards of competence
, and
promoting professional growth and
development
. At the time the first edition was written, there was a very small number
of women faculty in most Departments of Surgery, and many women residents found it
difficult to identify appropriate role models and advisors to facilitate their surgical
education. The first three editions were therefore written primarily for women students
and residents. Over the years the wisdom contained in this publication has become a
resource for both male and female trainees, and the fourth edition was intentionally
gender-neutral. With this, the fifth edition of this publication, we have updated and
expanded the information and advice contained herein. We expect that all surgical
residents as well as medical students will find this book to be a valuable resource. It is
the intent of this book to provide practical information and advice, which we believe will
make your surgical training experience more rewarding. We hope it will help you
improve communication with your peers and attendings and inspire you to develop
confidence in your skills and abilities. We encourage those who derive benefit from this
publication to pass along the wisdom and share it with colleagues. We would like to
invite all who have benefited from this publication to join our organization.
3
TABLE OF CONTENTS
Preface……........................................................................................................1
Introduction......................................................................................................2
Chapter 1: Learning to be a Surgeon ...............................................................5
Professional Behavior
Knowledge and Patient Care
Making Decisions
Rounds
Presentations
Call
References
Chapter 2: Getting The Work Done ................................................................17
Internship
Junior Resident
Chief Resident
Residency Calendar
References
Chapter 3: In the Operating Room ................................................................26
Technical Skills
Operating Room Strategies
When a Case Is Not Going Well
References
Chapter 4: Care and Feeding of Your Surgical Education ..............................32
Core Competencies
Seeking and Using Feedback
ABSITE
Who’s Who in the Hierarchy
Mentors
References
Chapter 5: Problems and Pitfalls ...................................................................41
When You Make a Mistake
When a Patient Does Badly
Substance Abuse
Discrimination
Sexual Harassment
Reproductive Issues
Personal Relationships
4
Conflict Resolution
Resident Rights
If you Think You Want to Quit
References
Chapter 6: Taking Care of Yourself.................................................................54
Basics of Self-Preservation
Locker List
Life Balance
Occupational Hazards
Maintaining Relationships Outside the Hospital
References
Chapter 7: Directing Your Future....................................................................59
Research Experience
Non-traditional Experience
Fellowships
Board Certification
Practice Options
References
Chapter 8: For the Medical Student ...............................................................74
Introduction
The Junior Surgery Clerkship
Fourth Year Concerns
FAQs for Medical Students
Appendix.........................................................................................................85
Electronic Resources and References
ABSITE Resources
Surgical Bibliography
Quotes...........................................................................................................105
5
Chapter 1: LEARNING TO BE A SURGEON
PROFESSIONAL BEHAVIOR AND APPEARANCE
Appearance
Attendings, residents, nurses, and patients will be forming an opinion of you as a doctor
and as a coworker. You must learn to be professional and businesslike in your affect
and attire if you expect to be taken seriously as a surgeon. Begin with always being
clean, neat, well-groomed, and dressed in a professional and practical manner. Find out
exactly what the customary attire is for each institution participating in your particular
program. In some institutions, for example, scrubs are only to be worn in the operating
room (OR) or on call, but not on rounds, in clinic, or at conference. In other programs,
everyone wears scrubs most of the time. Some ORs have strict policies regarding the
wearing of jewelry in the OR, so check with the OR supervisor. Many programs will
have specific dress codes. Dress codes for men generally run to the collared shirt and
tie, which is easy enough to adhere to. Dress codes for women tend to be less specific,
and it may be more difficult to decide what is within the norm. Do not wear anything
that can remotely be considered seductive. Avoid short skirts, half shirts, low necklines,
sheer fabrics, dangling earrings and anything tight. Fingernails must be clean, and
trimmed or filed short. Comfortable shoes are a must in and outside the OR. Open-toe
shoes in clinic may be both a health hazard and prohibited in your institution. It is
possible to have style and flair – and dress like a professional. Ours is generally a
conservative profession; leave the green hair dye and glitter nail polish to your time off.
If in doubt, use this good rule of thumb: dress the part of the surgeon whom your
grandmother would be at ease to see as her surgeon. You can be yourself, but be
comfortable, and be practical. Remember that during the course of a day, you may be
seeing patients in clinic, pulling chest tubes, and helping out with a fresh trauma in the
Emergency Department (ED). Take this into consideration when dressing for the day.
NEVER continue to wear your white coat, shoes, scrubs, or any article of clothing if it is
visibly soiled by blood or other body fluids. It is not only unprofessional, it is a health
hazard. Store an extra outfit and shoes in your locker as backup.
Attitude
Be upbeat and positive. Treat everyone with respect, including nurses, fellow residents,
medical students, ancillary personnel, and other specialists, as well as your patients and
your superiors. Surgery is a team sport; nobody wants a whiner or complainer on their
team. Show enthusiasm for your chosen specialty; enthusiasm to learn begets
enthusiasm on the part of your senior residents and attendings to teach. Be open to
“The reward for work well done is the opportunity to do more.”
-- Jonas Salk, MD

6
learning from every situation you encounter; even a “negative” experience can serve as
an example of what NOT to do. Confidence on the one hand is a good thing, and
should come to you naturally as you gain greater clinical experience; arrogance,
however, is a dangerous character trait at any level. When you are tired and stressed,
you will be faced with all kinds of situations that will test your personal integrity,
judgment, and stamina. Try to view each challenge as a learning opportunity and do
your very best to avoid becoming defensive and hostile.
When you find yourself rotating on a subspecialty that you do not care for, or working
with a particularly difficult attending, do not let this affect how hard you work or how
well you work with others. Grit your teeth, keep your head down and your nose to the
grindstone. You can learn something by observing the strengths and weaknesses of
each of your colleagues. The world of surgery is amazingly small and the attending you
operate with today may be old friends with the head of that fellowship program you
want in a few years. Don’t burn any bridges. Keeping your goals in mind can help you
maintain perspective and keep you on track.
Behavior
Probably the most highly-valued characteristics of interns and junior house staff are
honesty, hard work, the ability to accept feedback and, particularly in the era of
resident work hour restrictions, efficiency (See Chapter 2, “Getting the Work Done”).
The greatest sins are laziness and being untrustworthy.
Beyond cultivating efficiency, you should identify and consciously emulate
characteristics of the surgeons you most admire. Do not imitate negative or juvenile
behaviors. Behave so that your honesty, integrity, sense of responsibility, and reliability
are never called into question.
Surgical residency is a long road with a number of physical and emotional challenges.
There is no doubt that at times you will feel overwhelmed. Don’t let it drag you down.
Do the best that you can and don’t be afraid to ask for help if you need it.
Professionalism
The ACGME (Accreditation Council for Graduate Medical Education)
1
has identified the
specific knowledge, skills, behaviors and attitudes, and the appropriate educational
experiences required of residents to complete Graduate Medical Education (GME)
programs. These are known as the six competencies (surgeons consider technical skills
to be the
seventh
competency). One of these (see Chapter 4) is “Professionalism”.
While there is considerable debate within the educational community regarding exactly
“You never know when you’ll be in need
of those you’ve despised.”
-- Cormac McCarthy, All the Pretty Horses, Knopf 1992

7
how professionalism should be taught, assessed, and remediated, it goes without
saying that you do not want your professionalism ever to be questioned.
Professionalism captures the essence of the physician’s duty to the public. The
construct includes such virtues as honesty, altruism, service, commitment, suspension
of self-interest, commitment to excellence, communication, and accountability.
Cultural Sensitivity
In your training and in your professional life, you will inevitably encounter attendings,
co-workers, and patients with very different cultural, religious, and political beliefs from
your own. In the professional setting, you must be respectful of these individual
differences. Avoid jokes or comments that degrade any member of society, be it an
alcoholic patient or a person who doesn’t speak English. Be aware of imposing your
own biases on others and letting these biases determine how you treat others. Keep an
open mind, learn about the challenges others face, and set a good example to others of
the sensitive, caring surgeon.
For more information, the Association of American Medical Colleges (AAMC) has a
number of useful resources.
2
Do Not Gossip!
Hospitals can be miniature soap operas. Remember the walls have ears! Think before
you speak or act. Never malign one colleague to another, and avoid bad-mouthing your
fellow residents under any circumstances. Be mindful of what you say of others; it will
reflect on you.
Profanity
Profane language is simply unprofessional. Don’t use it.
KNOWLEDGE AND PATIENT CARE
Medical Knowledge and Patient Care are two of the six ACGME competencies. Surgery
residents are required to demonstrate knowledge of established and evolving
biomedical, clinical, epidemiological and social behavioral sciences, as well as the
application of this knowledge to patient care.
3
This includes an ability to critically
evaluate and demonstrate knowledge of pertinent scientific information and a
knowledge of the fundamentals of basic science as applied to clinical surgery. In terms
of Patient Care, residents must be able to provide patient care that is compassionate,
appropriate, and effective for the treatment of health problems and the promotion of
health. In addition, residents must demonstrate level-appropriate manual dexterity; and
develop and execute patient care plans.
Our character is what we do when no one is looking.
--
H. Jackson Browne
8
The obvious professional activity that distinguishes surgeons from other physicians is
performing operations. While good operative technique is critical to competence, the
fundamental ability surgeons MUST possess is incisive clinical reasoning and decision-
making. This allows surgeons not only to make an accurate diagnosis, but also to
conduct the operative procedure and manage the patient’s clinical course. The care of
the surgical patient is accomplished by a series of clinical decisions – some large, most
small – often in the face of incomplete data. Developing the ability to make reasoned
and prompt judgments under stress with overt confidence is essential to independent
surgical practice.
One of the criteria universally used to evaluate surgical residents is “fund of medical
knowledge”. An assessment of medical knowledge is made based on performance on
standardized tests such as the ABSITE (American Board of Surgery In-Training
Examination)
4
and on direct observation of your clinical behavior and decision making.
You will be assessed, usually at the end of each rotation, on whether you know what
you ought to know at a given stage in your training. If you are simply carrying out a
series of assigned tasks with no understanding of why, you will never become a
competent surgeon. Some knowledge is gained simply from experience. Nurses, scrub
technicians, x-ray technicians, and other ancillary personnel can be excellent sources of
practical tips. You can learn a lot by both watching and speaking with your attendings
and senior residents. Morbidity and Mortality (“M&M”) conference is an invaluable forum
to learn from the mistakes of others and how to handle complications when they arise.
Grand Rounds and other academic conferences are useful for reviewing certain clinical
topics and for staying abreast of new developments in the specialty.
Reading
Reading is an essential component of residency training. You will never gain a thorough
understanding of the complexities of surgery without spending time reading. Both
textbooks and surgical journals must become part of your own personal library. Surgery
is not a static profession – it is constantly changing and improving. New technologies
and advances in basic sciences have transformed the specialty of surgery just in the
past few decades. One of the great joys of being a surgeon is that you never get bored.
There is always something new to learn, so get into the habit of reading daily. Most of
the major texts and journals are readily available online and an entire library can be
carried in your pocket on your smartphone or electronic tablet, so there is no excuse for
not reading!
Reference Materials
Most surgery training programs subscribe to the SCORE (Surgical Council on Resident
Education) curriculum,
5
the American College of Surgeons Fundamentals of Surgery
Program,
6
and/or UpToDate.
7
Every surgery resident should USE at least one standard
surgical text and a good atlas. (See the Appendix for suggestions.) Review every
surgical diagnosis and procedure preoperatively in your preferred text and atlas.
Prepare for every elective surgical case, particularly the first time you encounter a
9
problem or procedure. Adults remember best those things that they learn experientially.
Learning that is motivated by reading about your patients is likely to be remembered for
a lifetime. Besides having a general idea of the operative steps, you should also know
the indications for and possible risks and complications of a given operation or
procedure, and alternatives.
Study Habits
As a medical student, you could spend a week in the library and “cram” for an
examination. In residency this amount of protected time will not be an option, and this
approach is not recommended in any case. Therefore, you need to adapt your study
habits and find a way to study in shorter but more frequent time periods. Here are
some hints for reading during residency:
Carry a pocket copy of one of the major surgical texts (or an electronic
version) with you at all times. This will help you learn the basics and serve as
a reference for you to understand your patients’ problems, and can alert you
to related concerns.
Formulate a reading program that will ensure adequate coverage of the
relevant material for the service on which you rotate. Read all the pertinent
material. Set a specific goal for your reading every day,
and stick to it!
Don’t
underestimate the amount that can be learned in short periods of study.
Utilize the quiet times when you are on call to read.
Pick one journal and read it each month, even if you only skim it.
The
Archives of Surgery
and
American Journal of Surgery
are good choices. Read
through the abstracts or the summaries, and if there is time you can read the
articles in full. You will likely receive a few “throw away” journals in the mail
for free. Tear out the better articles and keep them in your coat pocket for
reading during down-time.
Review
Selected Readings in General Surgery
, and make sure you read
the overview each month (see Appendix).
Look upon your reading time as a treat, not as a chore.
Ask for suggestions on specific reading from your attending or senior
residents, particularly if you encounter something new that is not covered in
your texts.
If your program has enrolled residents with the American College of
Surgeons Resident and Associate (RAS) Program,
8
this will give you
access to many online resources such as
Access Surgery
.
9
MAKING DECISIONS
Seasoned judgment is the consequence of making decisions, observing the results, and
learning from both successes and failures. Much more is learned from mistakes,
particularly one’s own, than from things that go well. It is all too easy for the intern and
junior resident to focus on pragmatic immediate tasks to be accomplished for the
10
patient, chief resident, or attending, rather than considering the problem the patient
presents as an exercise in diagnosis and management. Only by actually making
judgments and observing the consequences of those judgments will you develop the
confidence to function independently. With each new patient, try to evaluate the
problem, make a differential, and formulate a plan of action in your own mind, even
though others may have presented the case signed, sealed, and delivered.
Be complete in your work-ups; you will often find things that others miss, such as
identifying a colon cancer by rectal exam on a hernia patient. Quality almost always
trumps speed. If your findings are not in agreement or you identify something not
previously documented, speak up and pass on the information in a respectful and
discrete manner. Many of your senior residents primarily will appear to value the
speediness with which you complete your work. But in the long run, you will learn more
if you force yourself to think past the admission H&P. If an operation is indicated,
decide which one, the ideal timing of the procedure, if any additional studies are
needed preoperatively, and the alternatives to surgery. Do not stop thinking! This
sounds kind of funny but it can be a real challenge when you are trying hard to
complete a long list of daily tasks. Review the radiographs of your patients with a
radiologist so you learn to read films yourself. Go to the pathology lab and view the
slides of specimens. Follow up on autopsy results when patients die; this is a very
useful and usually underutilized learning opportunity. Ask attendings for follow-up on
patients who have been discharged if you don’t have an opportunity to see a patient
yourself. This is increasingly important given the compromised continuity in patient care
that may result from work hour restrictions.
Plan of Action
When presenting a new case to the chief or attending, have a plan of action already in
mind and suggest it. Only by demonstrating your own problem-solving abilities will you
be judged capable of being a surgeon. At the very least, whenever a new diagnosis
comes up, review the appropriate section in your preferred pocket resource.
ROUNDS
The style of rounds will vary with your program and the hospital service on which you
are rotating. Chief resident morning rounds tend to be devoted primarily to patient
care, while attending rounds serve the dual purpose of teaching as well as keeping the
staff informed of patients’ progress. If you are in a private hospital, you may find you
only make rounds with individual surgeons to whom you have been assigned. This can
get challenging if several round at the same hour, but won’t round together; if this
happens, always inform your attending(s) of this conflict so they know where you are.
If you are not sure how to choose which attending to accompany on rounds, ask a
senior resident.
11
Your behavior and performance on rounds is of utmost importance during internship
since this will be your first and best chance to prove yourself. It will also be your most
frequent exposure to staff, and the decision of whether or not to assign cases to you
can depend on it. Be sure to read Chapter 2 on “Getting The Work Done.” Here are
some additional tips:
• Be on time.
• Pay attention. Idle chitchat and socializing is a great way to miss important details
of patient care that could have an adverse impact on patient safety and on your
evaluation by the attending.
• Know the patients and be able to give a BRIEF description of their
problems. This usually consists of the patient’s age, current surgical diagnosis
and procedure (planned or completed), date of the procedure, current status and
clinical plan going forward. However, the preferred format may vary within
specialties so observe how the senior residents present to the attending. Be ready to
review vital signs and their trends, pertinent labs and imaging studies, pertinent
physical exam findings, etc. Formulate a plan for dealing with any problems you
have identified and present them for approval.
• Make sure people can see and hear you. Move to the front if someone else has
been presenting before you. Use note cards as needed, but don’t “read” everything;
show you know the patient. Speak up and speak clearly. Make
declarative statements, bringing your voice down at the end of a sentence. Do not
end your remarks, ideas, and treatment plans with a tag question such as “don’t you
agree?” “Okay?” “You know?” These expose your uneasiness and need for
reassurance. Hedging phrases, for example “sort of, kind of, and could be” also
diminish your impact. Use strong verbs such as “I will...” and declarative statements
like “my plan is to...” rather than “you could...”, “maybe I would...” or “I would like
to...”
• Stay organized. Present patients in a logical, orderly fashion. Know what you are
going to say before you say it. Give the patient summary, vital signs, physical
examination, lab results, radiology results, assessment and plan in a consistent
manner. Jumping all over the place makes you look disorganized in your approach
to clinical problems and your ability to formulate a plan for further work up and
treatment. It also makes it difficult for those listening to understand what’s really
happening with a patient.
• Keep track of tasks. Use an organized patient list to take notes on rounds. Make a
checklist of tasks to do and test results to follow up on at a later time. Run this list
prior to leaving for the day to ensure that all of your patient care has been
completed and that the appropriate information has been checked out to the on-call
resident. S
ome procedures require specific preoperative order sets (such as a bowel
prep for colon surgery – see the chapter on “Getting the Work Done”). Your chief or
attending may forget to mention the orders to you, assuming you already know
them. If it is an emergency, look it up, but at the very least get some experienced
help if you are unclear about anything you are tasked to do.

12
• Don’t be afraid to say “I don’t know” or “I haven’t done that yet.” NEVER
make up lab values or x-ray reports if you don’t know them, even when you
should
know them. NEVER say you have done something if you have not. This is both
unethical and dangerous, and will get you fired. If you normally work hard, pay
attention, and show interest, your superiors understand that some details will get
lost in the shuffle and they will not hold it against you. Lying is not the solution and
may be grounds for dismissal.
• Keep an online resource text in your coat pocket (or app on your mobile
electronic device), such as the Mont Reid Surgical Handbook
10
(see Appendix for
other references), in case you need to look up some basic information as you are
walking to the bedside of a more complicated case. For example, you might want to
double-check the correct weaning parameters on a patient who is about ready for
extubation.
• Anticipate needs on working rounds to make them more efficient. For
example, keep dressing supplies handy if you know a wound is going to need to be
checked. Everyone appreciates a timesaver.
• Keep a neat and clean appearance. If the attendings don’t wear scrubs on
rounds, you probably shouldn’t. Do not carry food or drinks with you on rounds.
• Have a good attitude. If good-natured bantering occurs, respond assertively, not
defensively. Learn to laugh at yourself. Don’t whine or pout.
PRESENTATIONS
Throughout your residency you will be required to present at various conferences, such
as M&M and Grand Rounds. The manner in which you do this will play an important role
in how you are perceived by your colleagues. Presentations should be viewed as an
opportunity to learn and enhance your reputation, and they require definite effort on
your part beforehand. If you are not well prepared, you will lose ground fast. For all
presentations:
Discuss the presentation beforehand with a more senior resident. They
have experience giving presentations and are an invaluable tool for which format
to use, what topic to present, what information needs to be included, and
questions that might come up from the attendings. Learn from their experience.
Always inform the attending responsible for the patient if their case is to be
presented in M&M.
Make sure you are on time. If you are detained in the OR or have an
emergency, arrange for another resident to present the case.
“If all my powers and possessions were to be taken from me with one exception,
I would choose the power of speech, for by it I could recover all else.”
-- Nathaniel Webster
13
Be concise. Speak clearly and precisely. Present only the data that is
pertinent to the specific conference or rounds at which you are speaking. More of
the H&P details will be required at a case presentation conference than for a
Morbidity & Mortality conference, where the main issues are the surgery
performed and the complications.
Speak loudly enough to be heard by everyone present. If a microphone is
available, use it. Make a conscious effort to improve a soft voice, stammer, or
language difficulty. Practice speaking in a similar room, with a friend or two to
critique your efforts. Nothing makes a worse impression than if you can not be
heard or understood. Avoid talking too fast or using a high-pitched tone; these
are dead giveaways that you are nervous. Serious performance anxiety can
sometimes be treated medically; we advise seeking professional advice regarding
the medical treatment of anxiety if you feel your situation warrants it.
Check the dress code for presenters. Abide by it.
Plan what you are going to say carefully. Speak from note cards with key
words until you gain experience and confidence. Avoid memorizing a script, as
you are more likely to lose your place this way. Aim for brevity and clarity.
Continue on if you stumble. There is no need to profusely apologize, as this
tends only to draw attention to the error.
Think in advance of questions you may be asked. Either include the
answers to these questions in your presentation, or be prepared with the
answers at the end. If there is a visiting professor, ascertain his or her area of
expertise ahead of time and be prepared for more esoteric questions. Do not
guess an answer to a question or make an excuse for why you can not answer.
Simply reply that you do not know, but that you will make an effort to find out, if
that appears to be required. Be certain that you know the evidence-based
medicine to support your decisions.
After the conference, seek feedback on your performance by asking
senior residents and/or trusted friends. If you make mistakes, try not to
repeat them at the next presentation.
Preparing for higher profile meeting presentations (local, regional or
national).
11
• Practice, practice, practice. Plan on giving at least one “practice”
presentation, complete with slides, to your mentor well in advance of the
meeting. Check out the podium set up in the break before the talk so that you
know how to advance the slides and use the pointer. If necessary adjust the
microphone to your height. If water is provided, hide a glass under the podium
so that you can access it if needed.
• The first thirty seconds of your presentation are CRUCIAL. Unless you
are otherwise instructed, the usual format for a research presentation is:
Background, Purpose, Methods, Results, Conclusions and Study Limitations.
14
• If presenting from slides, standardize the background and color
formats of your slides. Studies show that light color backgrounds with dark
color letters are the easiest on the eyes. The Society or Organization to which
you are presenting may ask you to use a specific format or PowerPoint template.
Alternatively, your institution might mandate a specific institutional format, so
check with your mentor in advance. Stick with three or fewer colors for word
slides and use picture slides in place of text slides whenever possible. The font
should be at least 24pt and avoid more than about ten lines of text on the slide.
Avoid reading your slides. The bullet points on slides should give the key words –
you provide the explanation.
• If using a laser pointer or computer mouse pointer, balance your hand on the
podium or with your other hand to minimize the appearance of tremors. Be
judicious in your consumption of caffeine before your presentation. Use the
pointer economically; there is nothing more annoying or distracting than sitting
through a presentation where the speaker points to every word on a slide.
• Prepare for questions. Begin answering the question with eye contact to the
questioner, then move to the rest of the room.
• Project confidence! Remember, you will usually know more about your topic
than anyone else in the room.
CALL
Taking call is an essential part of surgical training, whether it’s overnight call or a “night
float” system. However the ACGME no longer permits interns to take call and these
work periods should be referred to as “duty periods” whether during the day or at
night.
3
While the days of a trainee sitting at a patient’s bedside for 36 hours straight
are definitely over, there is no doubt that the hospital is a different place at night and
on weekends. You will have to make critical decisions with fewer senior residents and
fewer ancillary staff to support you. At the start of each rotation, establish expectations
with the chief resident about when you should call him/her. When you are new, a good
plan is to set up a specific time to call and “run the list”. This avoids calling with each
minor issue but provides you with a safety net.
ACGME requires that each program provide guidelines for resident supervision and
these should be made available to you at orientation. If in doubt, call a senior person!
There is ALWAYS backup and communication is essential. Often you will have your first
opportunities to participate in more difficult cases at night, as there are fewer senior
residents available to assist in the operating room. Night time duty periods translate
into caring for more patients, including those who are not personally known to you.
When an issue arises with a patient,
go see the patient
, especially if you are unfamiliar
with his or her hospital course or the issue is new to that particular patient. Efficiency,
prioritization, and triaging care are essential skills when you are covering many
services. Use your time wisely and call for help if it becomes overwhelming or any time
patient care is at risk.
15
While the duty schedule should be as fair as possible, it may not always come out equal
for a variety of reasons. If you feel that there is a systematic pattern of unequal or
inequitable night or weekend duty, ask for clarification from the person responsible for
making the schedule. If the problem persists, your program director is the next best
person to approach. You and your fellow residents will need to perform as a team.
Adjustments in the schedule may be necessary to cover unexpected absences. You
never know when you will require emergency leave and they will pick up the slack for
you. In general, surgery is a team sport and being selfish is not appreciated.
Call provides an opportunity to gain some independence in decision-making and triage.
Maintain a good attitude about why you’re there and take advantage of any
opportunities you have to learn new skills and management strategies. In the morning,
shower and try to look as fresh and alert as possible, no matter how little sleep you got
the night before. Most people will know you were up all night, but that is no excuse for
a disheveled appearance. You can do it!
Duty Hour Restrictions
Residency Programs must ensure their trainees strictly adhere to an 80-hour work week
to maintain accreditation. You are required to document your hours and you must
speak up if you are scheduled to work more than the ACGME regulations permit or if
you are encouraged to enter your duty hours dishonestly. Training programs are
penalized for duty hour infringements, so the program director should be appreciative
when a problem is brought to his/her attention. Use your best judgment regarding the
use of your time, and let your chief resident know in advance if you think that you will
not be able to comply with the hours. Your program should be setting up rotations to
facilitate compliance, and you should be encouraged to speak up when you are not able
to comply. Adjustments may be necessary on occasion to successfully do this, and you
should discuss this with your chief resident if the schedule for the week or events have
arisen that would put you over the 80-hour limit. This may mean sacrificing cases;
hopefully good planning and foresight will help prevent this.
Patient Hand-Offs
Patient hand-offs are an integral element of patient care, and regularly passing off
information about your patients and associated “to-dos” is the rule. It will benefit you to
gain a reputation as a resident who takes care of the necessary tasks during the day.
Knowing your patients well and communicating this will be critical to the best care of
your patients, and will contribute to your reputation as reliable, thoughtful, and
considerate of others. Organization and communication are extremely important skills to
ensure optimal quality patient care.
12-14
REFERENCES
1. Accreditation Council for Graduate Medical Education (ACGME)
http://www.acgme.org/acWebsite/home/home.asp. Accessed 6/6/12

16
2. American Association of Colleges of Medicine (AAMC).
https://www.aamc.org/download/54340/data/tacctbibalpha.pdf. Accessed 6.6.12
3. Surgery Residency Review Committee Program Requirements
http://www.acgme.org/acWebsite/downloads/RRC_progReq/440_general_surgery_01
012008_07012012.pdf. Accessed 6.6.12
4. American Board of Surgery http://www.absurgery.org/. Accessed 6.6.12
5. Surgical Council On Resident Education (SCORE) Curriculum.
https://portal.surgicalcore.org/. Accessed 6.6.12
6. American College of Surgeons Fundamentals of Surgery Curriculum.
http://www.facs.org/education/fsc/index.html. Accessed 6.6.12
7.
UpToDate
. http://www.uptodate.com/contents/search. Accessed 6.6.12
8. American College of Surgeons Resident and Associate Society.
http://www.facs.org/ras-acs/index.html. Accessed 6.6.12
9. Access Surgery. http://www.accesssurgery.com/. Accessed 6.6.12
10. The Mont Reid Surgical Handbook, 6
th
Edition. (Scott Berry et al., 2008, Mosby
Yearbook, Inc.)
11. Taylor K et al. “Effective Presentations; How can we Learn from the Experts?”
Medical Teacher
1999; (21):5-11
12. Greenberg CC, et al. “Patterns of Communication Breakdowns Resulting in Injury
to Surgical Patients.”
JACS
2007; 204: 533-540.
13. Singh H, et al. “Medical Errors Involving Housestaff: A Study of Closed
Malpractice Claims from 5 Insurers.”
Arch Intern Med
2007; 167: 2030-2036
14. Arora V, Johnson J. “A Model for Building a Standardized Hand-Off Protocol.”
Jt
Comm J Qual Patient Saf.
2006; 32(11):646-655.
17
Chapter 2: GETTING THE WORK DONE
The balance between service and education is a fine one because residency training
was founded on an apprenticeship model where both are important.
1
In addition,
residents are hospital employees who are paid to provide services that include ordering
tests and completing paper work. Occasionally this work will appear to be demeaning,
but it is essential to appreciate and value service to the patient as part of your
education to become a health care professional.
2
INTERNSHIP
The keys to surviving internship are organization, efficiency, and prioritization of tasks.
Time is a precious commodity and must be managed expertly or you will be lost – a
dangerous situation both for an intern and patients. The primary and essential role of
an intern is to be the gatherer of data, keeper and communicator of information, and
doer of tasks. The intern’s role is to learn about surgical disease processes and to
acquire the basic surgical skills necessary for a career in surgery. (However, more
senior residents rarely perceive operating as a priority for the intern.) Internship is an
exciting time filled with new educational experiences, including adjusting to a new role.
It is vital to recognize that as an intern you are the team’s foundation. The intern truly
is the eyes, ears, and hands of the surgical team outside of the operating room. If you
recognize the importance of this role, you will be able to find reason and purpose in the
sometimes mundane and sometimes overwhelming number of tasks to complete.
Remember the entire team and its patients rely on a good intern getting the work done.
Pay Attention. Truly listen to what is being said on rounds about the patients and
their proposed plans of care, both short- and long-term, and write it down. Important
information is communicated, and understanding it and relaying it accurately are
essential for optimal patient care. Not only does paying attention to patient plans help
make you efficient and organized in completing tasks, but it can also be seen as a
learning opportunity on pre- and post-operative patient care. It is beneficial to learn
and remember the patient care preferences of individual attendings with whom you
work. (Also see “Rounds” in Chapter One.)
Write it All Down in One Place. As soon as a plan is formulated, put it in writing.
You will NOT remember everything that is supposed to happen every day to every
patient. Many programs have interns use clipboards, patient lists, etc. Whatever system
you use, be consistent and always write it down in one place.
“I long to accomplish a great and noble task, but it is my chief duty to accomplish
humble tasks as though they were great and noble. The world is moved along, not
only by the mighty shoves of its heroes, but also by the aggregate of the tiny
pushes of each honest worker.” -- Helen Keller
18
At a minimum, you should always have the following information at hand:
• Patients – name, age, diagnosis, location, attending, ID number, significant
medical history, post-operative day, diet status (NPO/clears/regular), drains/lines,
and pertinent medications, including antibiotics, etc.
• Labs – which tests on which patients, and when results should be ready.
• Radiology – which tests, which patients, when results should be available, who
needs to be scheduled, when the test will be performed, and what prep, if any, is
required.
• Consults – what consulting service, which patients, which resident or attending
to call, and most importantly, the reason for a consult. Descriptions of key clinical
issues, the reason for and urgency of the consult are all important in
communicating with consultants. Ascertain if any specific tests should be ordered
for a patient so that the results are available for the consultant. For example, if a
patient needs a cardiology consult, often an ECG and Echo should be ordered/
completed. Also, be sure to ask when the consultant will be able to see a patient,
and the name and pager number of the individual to contact for follow up. Always
treat consultants with respect and never criticize their recommendations in front
of the patient. Also, avoid preempting a consultant decision; for example when
consulting a cardiologist do not tell the patient that the cardiologist will want to
do a cardiac cath as this will create mistrust if the consultant offers an alternate
management plan.
• If you have trouble scheduling tests and procedures or obtaining a
consult, let your senior resident or attending know as early as possible. Leave
the decision up to them regarding whether to wait or press the issue. They may
also have better persuasive ability than you do by virtue of their seniority.
• Other studies – ECGs, Echos, etc.
• Bedside Procedures: dressing changes, IV starts, CVP lines, NG tubes, drain
tubes to be pulled, etc.
• OR schedule – who needs pre-op and post-op checks (and on what cases you
have an opportunity to be in the operating room).
• Admissions – scheduled and emergent. Don’t forget to add these patients to the
service list and check their labs, etc.
• Paperwork – dictate discharge and transfer summaries, contact primary care
physicians, prepare prescriptions, and any special needs for discharge such as
physical therapy, ostomy teaching, home TPN, etc.
• Attending, resident, and ancillary staff contact information, commonly
used phone numbers, door codes, etc. Make sure you know your attendings’
preferred mode of communication; some may not wear pagers and prefer to be
contacted by other means.
An important note: Cross coverage and sign outs (or hand offs) are increasingly
important (see “Patient hand-offs” in Chapter 1). Make sure that your notes are
complete, clear and legible so that anyone taking care of your patient can pick up

19
where you left off without skipping a beat. Be complete in your sign out. Note the
recurring themes of how important organization and communication skills are. This
applies to both verbal and written forms of communication.
Do It Now. Following morning rounds, begin the day’s work
immediately
. Organize the
day by looking at the list of things noted on rounds and consolidating as many as
possible, as well as prioritizing which tasks need to be completed first. For example, sit
down and make all phone calls at once; if lab results are available by 10 AM, check
them at 10:15. Waiting until the afternoon to check morning lab results may create an
avoidable situation of discovering that the wrong lab was sent (or was never actually
sent), or finding critical lab values that are not addressed for several hours after being
available. Do not procrastinate, even on a light day! Your goal should be to have all the
“routine” work completed before noon. Tasks such as consultations and imaging
studies, which depend on others, should be scheduled first. The early bird does catch
the worm; tests scheduled first thing after rounds will usually be run earlier than if you
wait until the afternoon. Begin the discharges as soon as the above orders have been
entered. Getting people on their way allows rooms to be turned over, nurses to be
freed up, and admissions to come in. You never know what disaster lurks in the ED or
when a surprise admission from clinic may wreck plans to do things later. If a patient is
planned for discharge the next morning, complete the discharge paperwork the day
before if possible. Delegate where you can, but be sure to follow-up on your assistants
(e.g. medical students or physician assistants).
Always Make Waiting Times Productive Times. While waiting for the next case to
begin, write post-operative orders, make phone calls, read your pocket textbook or
study from an online resource. It may be tempting to sit in the lounge and socialize, but
most lounge conversations are rarely educational unless you make a point to turn the
conversation to the case at hand. (On the other hand, occasional social conversations
may keep you from appearing stand-offish.) While scrubbing, ask the attending or
senior resident about post-operative management, any preferences regarding orders,
dressings, drains, tubes, etc. Also use the time to develop and discuss your learning
objectives for the case.
3
Start Admission H&Ps, even if you don’t think you have time to complete them. You
may think you need more time than turns out to be necessary and you are apt to never
feel you have a large enough block of time. Just Do It! This can be especially
important if you need a translator or some family member who may not be there when
you come back, prolonging the time required. You may also discover tests that have not
yet been ordered that will need to be expedited after you get the patient’s history and
medication list.
“The surest way to be late is to have plenty of time.” -- Leo Kennedy
20
Make Learning a Priority. Work must be completed, and sick patients tended to, but
always remember that you are there to learn the art and science of surgery. You must
be proactive about your surgical learning experience. Make every effort to spend as
much time in the OR as possible. Your presence there can only be interpreted as
enthusiasm for surgery, and your absence a lack thereof. Attending surgeons are
important to your evaluations and your future. They will be more likely to give you
better cases and to assume a more active mentoring role if you take the initiative to be
in the OR.
Know Your Cases. Be sure to obtain the case assignments at least the day before.
Always make time to read about the operation beforehand. Meet the patient before the
surgery, and be sure you know the indication for the operation, pertinent anatomy, and
main surgical steps. Never go to a scheduled case unprepared; this will leave a poor
impression on the attending and senior residents, and most importantly, will cheat you
from a full learning experience. (For surgical resources, see Appendix.) Also, team
members unfamiliar with the patient history can pose a risk to the patient.
Keep a Case Log and Copies of Your Operative Reports. You will need a
complete list of ALL your defined category cases, especially ones in which you are the
primary surgeon or the first assistant, in order to sit the American Board of Surgery
Examinations.
4
Most residency programs require residents to submit a list of cases at
regular intervals. You must also keep track of procedures, including chest tubes
inserted, central lines and Swan-Ganz catheters placed, endoscopies, etc., as well as
non-operative trauma and ICU cases that you have managed. (For your own
information and edification, also record any complications you may have had.) For each
of these procedures record the patient’s name, medical record number, date, attending
surgeon, service (general surgery, plastics, etc.), the procedure, and what role in the
procedure you played (primary surgeon, first-assistant, teaching resident, etc.). Some
residencies will also require you to list the CPT code assigned to that procedure. Some
residents do this by imprinting an index card with the patient and case information;
others use stickers in a logbook, or personal organizers. (If you use a computer system,
be sure to have an updated backup at all times! Many residents have lost their case
logs this way.) Cases are logged in to the ACGME Website
5
electronically. Make sure to
enter your cases in a timely fashion and be disciplined about it. It is very easy to lose
track of cases. The American College of Surgeons also has a Website for logging cases.
6
Delegate. Let other people do their jobs. Learning to delegate is an important
component of being organized and establishing a leadership style. There is a tendency
for interns to believe that they alone need to solve all patient problems, such as
arranging transportation and/or dealing with social situations. Remember that social
workers, ostomy nurses, and other ancillary personnel are trained to take care of
certain aspects of patient care and you should let them do it.
21
Inform Your Superiors. Make a point of informing your chief resident and attending
of tasks accomplished and any significant changes or abnormal results identified
throughout the day. If something you think is very important comes up, inform your
chief between cases, or go in to the operating room. Be careful that you are not
interrupting at a critical point in a case. (Try asking the circulating nurse if it is a good
time or not, or just wait quietly off to the side within the peripheral vision of the
attending, who may speak to you when ready. Better yet, ask how your chief prefers
these types of things handled
before
such a situation arises.) Many times your
appearance in the OR will give you a chance to see something interesting, and it
informs your attending that you are both interested in the case and are staying on top
of things on the ward. Remember the importance of good communication. This is
essential when a patient’s condition deteriorates or there is critical information to share.
Teach the Medical Students. During your internship you will be acquiring the skills
you will need to teach students, which may continue throughout your career. You are
not expected to lecture, but you are expected to explain things and to be a role model
for them. Students are typically happiest when they are doing something they feel is
useful for patient care or contributing to the team, so assign them tasks within the
constraints of your institutional policies (e.g. in some institutions medical students are
forbidden to write in the medical record). Instill a sense of responsibility in the students,
but don’t jeopardize your reputation or your patients’ care by relying entirely on medical
students. When assigning tasks, establish a subsequent time to review what has been
accomplished. Recognize that
any
tasks you delegate to a medical student are
ultimately
your
responsibility. When students ask questions (academic or practical) to
which you do not know the answer, tell them where to find out. Don’t forget to specify
when you expect them to share the answers with the team. Keep in mind that medical
students are present to learn and to be part of the surgical team. For many, it is their
only exposure to a surgical service during their entire careers. Do not underestimate the
potential you have to positively influence their experience. Many programs recognize
outstanding resident teachers each year, or conduct “Resident as Teacher” Courses for
the residents. If a course is not available in your program, ask to participate in the
American College of Surgeons Resident as Teachers and Leaders Program.
7
Document Your Actions. In this litigious society, it didn’t happen if it’s not in the
chart. Every time you have a significant interaction with a patient, especially with a
critically ill patient, briefly note it in the chart. Not only is this good for medico-legal
reasons, it lets your attending and others know you are following the case closely. It
takes two minutes to write: you were called to the patient’s bedside for (x problem),
the patient was seen and examined, the pertinent findings, the assessment and plan
(labs, tests, or observation only), and the senior-level resident with whom you
discussed the problem and plan. Never use the patient record to argue with a
colleague. If you disagree with an entry, go and have a conversation.
22
Keep the Nurses Informed and Involved. The nursing staff is often stretched thin
in these days of managed care. By spending five minutes after rounds to inform the
nurses about the day’s plan for patients and answer questions, you will reap the
rewards of better teamwork, and from a practical standpoint may avoid unnecessary
pages. It’s important to communicate not just what needs to be done with a patient for
the day, but why, as it instills a sense of cooperation and allows the nurses to prioritize
their aspects of patient care. You will find that most nurses will work in the patient’s
best interest as well as yours when they understand why a certain task needs to be
completed sooner rather than later. A collaborative approach usually is the best
approach.
Patients First. There will be times when you are needed in multiple places at the
same time and you just can’t do it all. A general rule for staying out of trouble is to
“keep the interest of the patient foremost in your mind.” If a patient is critical and you
are expected at a conference, for example, ask a nurse or someone else to call the
appropriate superior (senior resident or attending) and let him or her know where you
are and why you can’t be there. If conference attendance is truly required, make sure
your attending knows of any significant changes in your patient’s condition, particularly
if the patient is deteriorating. Few attendings will get upset when you miss conference
if they see you were putting the interest of a sick patient first. (This does NOT apply to
non-critical issues and things that should have been done previously, like discharge
summaries.)
Maintain a Positive Attitude. Residency and hospitals can be extremely frustrating
and aggravating. Internship is filled with many challenges, including learning how to
work with ancillary staff during stressful and overwhelming situations. By learning the
names of support staff, returning pages in a cordial manner, and treating nurses as
colleagues (even if at times they may be hostile or even question your abilities as a
physician), you will be amazed at how much you will benefit. There will be times when
your ability to maintain a positive attitude will be challenged. These are the moments to
really shine by remaining steadfastly professional and composed. If needed, take a
minute alone during times of chaos to refocus and refresh, whether it’s in a restroom or
call room.
Take care of yourself. Integrate taking care of yourself into your daily work schedule.
It is important to make sure you eat more than one meal a day; eating healthy gives
you energy to get your work done and you will be less tired. See Chapter 6, “Taking
Care of Yourself” for additional advice.
Integrate study time into your daily routine. Even when you come home dead tired,
make it a point to read an article from PubMed about a topic you encountered in a
consult, or keep flashcards at your bedside.
23
Again, the keys to surviving surgical residency are organization, efficiency, and
prioritization of tasks. Follow the suggestions above, and remember that you can and
will make it through surgical training!
JUNIOR RESIDENT
As you move up the hierarchy of the surgical team you are expected to assume
increasing levels of responsibility for patient care. It is very important that you know all
the critical history of patients on the entire service whether you were the resident
surgeon on that case or not. This is imperative to providing good care, and models
behavior for the intern.
You will be expected to take a more active role in the decision-making process,
particularly in the diagnostic work-up and treatment planning for patients coming
through the emergency room. It is also a reasonable expectation that you will facilitate
this process for the interns. The expectation that you will take more responsibility as
you become more senior extends to the operating room, and you are expected to start
taking initiative (i.e. asking for instruments). In surgery you are expected to take
charge and be more assertive than in other specialties. If you aren’t, you just get
ignored. As Junior Resident you are also expected to be able to “fill in” for the Chief
Resident whenever he or she is detained in the OR or otherwise unavailable to make
decisions and report to the respective attendings.
CHIEF RESIDENT
As Chief Resident you are the official surgical team leader. You are expected to
organize the team in an effective and efficient manner to ensure that patient care is
optimal. This requires a great deal of organization and coordination. It is important to
orient all team members, including medical students and interns, to the team as early
as possible in the rotation. Inform them of the team schedule and explicitly state your
expectations and preferences. Make sure everyone knows the importance of his or her
role on the team. It is important to remember that junior residents and students will be
looking to you as an advisor and mentor. Recognize that your behavior is constantly
being observed and sets the tone for the team.
Patient issues must be identified and addressed on morning rounds, and responsibilities
are clarified and delegated at this time. It is important to be sure at the end of patient
rounds that all team members fully understand what is expected of them that day. An
open forum for communication is essential to good team dynamics. This is the best way
to ensure that the team is functioning as a system of checks and balances instead of
inefficient redundancy. Team members will not work to their full capacity if they do not
have the sense that they are making significant contributions and getting back a sense
of accomplishment. Giving feedback is another essential role of the team leader.
24
Remember that effective feedback should be FAST: Frequent, Accurate, Specific and
Timely. In addition, it should be delivered in a private environment.
RESIDENCY CALENDAR
Here is a list of things you can be doing to simplify your future as residency progresses.
Internship:
• Begin keeping a case log.
• Begin keeping an OR diary.
• Keep copies of your op reports. Don’t forget to record and dictate procedures such
as CVP lines, chest tubes, etc.
• Pick a mentor, or at least identify some potential ones.
• Scrub and do all the cases you can while still getting your ward work done. Even
being a second assistant can be a valuable experience.
• Begin looking for a topic of interest for research time. If you plan to go into research
after your second year, apply now for grant funding.
• Apply for membership in the American College of Surgeons, Resident and Associate
Society.
Second Year:
• Request fellowship information from several programs if there is a remote possibility
of you seeking subspecialty training.
• Arrange a lab year if you plan to do one (or two). Apply for grants.
• Continue your case log.
• Continue your OR diary.
• Scrub and do all the cases you can.
• Start developing your skills as a teacher to lower-level residents
Third Year:
• Begin the fellowship application process in earnest. Identify which programs will be
best for you, find people to write letters of reference, and make sure you have met
all the prerequisites.
• Finalize arrangements for a lab year.
• Continue your case log and OR diary.
• Scrub and do all the cases you can.
Fourth Year:
• Decide more definitely about your career path. Send for information on places
where you might be interested in practicing.
• Apply for fellowships.
• Continue your case log and OR diary.
• Scrub and do all the cases you can.
25
Fifth Year:
• Meet with the residency coordinator to discuss the requirements (including
paperwork) necessary for you to apply for your Boards and license. NOTE THE
IMPORTANT DEADLINES.
• Start looking for a job if you are not going to do a fellowship. Consider signing on
with a search firm or doing Locum Tenens if you don’t find the job you want.
• Get a permanent medical license in at least one state. The license you practice
under as a resident is usually conditional or temporary. You will need a permanent
license to take your Boards after completing residency. The application process
often takes 3-6 months.
• Fill out the preliminary application for the ABS Exam.
• Scrub and do all the cases you can. Before long, you will be on your own – possibly
alone. Offer to take a Junior Resident through a case while the attending supervises
without scrubbing. Ask the attending to give you more autonomy within the
constraints of patient safety.
REFERENCES
1. Reines, HD; et al. “Defining service and education: the first step to developing
the correct balance.”
Surgery
2007; 142 (2): 303-310.
2. Sanfey et al. “Service or Education: In the Eye of the Beholder?”
Arch Surg.
2011;146(12):1389-1395
3. Roberts, NK et al. “The Briefing, Intraoperative Teaching, Debriefing Model for
Teaching in the Operating Room.”
J Am Coll Surg.
2009 Feb;208(2):299-303.
4. American Board of Surgery http://www.absurgery.org/. Accessed 6.6.12
5. Accreditation Council for Graduate Medical Education (ACGME)
http://www.acgme.org/acWebsite/home/home.asp. Accessed 6.6.12
6. American College of Surgeons Case Entry System.
http://www.facs.org/members/caselogquickstart.pdf. Accessed 6.6.12
7. American College of Surgeons Residents as Teachers and Leaders Course.
http://www.facs.org/education/residentsasteachersandleaders.html. Accessed
6.6.12
26
Chapter 3: IN THE OPERATING ROOM
Obviously, what distinguishes the specialty of Surgery is what we as surgeons do in the
Operating Room.
TECHNICAL SKILLS
Economy of Motion
A universal characteristic of the best technical surgeons is not speed per se, but
economy of motion
. You will be better off at first with slow, deliberate movements than
if you rush. Fidgeting around and multiple trial movements waste time and make for
poor technique. Proficiency and speed will come with repetition. Listen attentively and
try to implement technical suggestions that are offered during your cases. If you do not
understand a technical instruction, ask for clarification or for the attending to
demonstrate for you.
Skills Lab/Simulation
The current training paradigm whereby residents learn in the operating room under
direct supervision through graded responsibility was introduced by William Halsted a
little over a century ago.
2
While teaching residents in the operating room is effective, it
is inefficient, costly, and may increase patient morbidity. In addition, the psychomotor
and perceptual skills required for the newer techniques of laparoscopic and robotic
surgery differ from traditional approaches. Therefore, surgical education has placed
increased reliance on simulation technology in order to improve and evaluate learner
proficiency, and provide controlled and safe practice opportunities.
3
All surgery training programs are now required to have a surgical skills lab and a skills
curriculum.
4
Ideally, the skills lab should be located close to the OR, with 24-hour
access to allow practice during down time between cases. The American College of
Surgeons and the Association of Program Directors in Surgery have established a three-
phase national skills curriculum for all surgery residents.
5
Phase 1 involves a number of
basic surgical skills modules each of which includes objectives for performance,
guidelines for practice and instructions for testing.
Proficiency-based training refers to
the concept of learners practicing certain surgical skills until testing shows them to be
at a predetermined level of ability. Trainees be allowed to progress to more demanding
technical skills only after achieving this predetermined level. Residents must
demonstrate proficiency in the Fundamentals of Laparoscopic Surgery prior to taking
the American Board of Surgery Examination.
6
This is the first example of proficiency-
based criteria for trainee assessment in a high stakes examination, and others will
follow.
Simulation is defined as ‘‘a person, device, or set of conditions which attempts to
present education and evaluation problems authentically.”
7
The trainee is required to
respond to the problems as he or she would under natural circumstances. Frequently

27
the trainee receives performance feedback either because this is built into a simulator,
or given by an instructor during a teaching session. Medical simulation comprises a wide
spectrum of tools and methods that vary in cost from cheap knot-tying boards to the
much more expensive virtual reality robotic models to team training simulations. For
basic laparoscopic skills, the training experiences increasingly rely on tools such as
laparoscopic video trainers and high-fidelity virtual reality laparoscopic simulators.
Simulation training has been demonstrated to have construct validity in a growing
number of studies.
3
More importantly, skills gained by simulation training have been
demonstrated to lead to improved performance in the OR.
3
Many programs have
specific laparoscopic trainers with which you can practice on your own time in addition
to dedicated laparoscopic skills labs. Knot-tying boards are available from the major
suture company representatives such as Ethicon or Davis & Geck. The OR Supervisor
should be able to give you contact information. If possible, get a board even before
you
start your internship so that you can practice during senior year in medical school.
Consider buying a used or cheap needle holder and forceps to practice instrument
handling. (Disposable instruments used by some ERs are satisfactory).
Practice
There is no substitute for practice, or as Arthur Rubinstein answered a stranger in New
York when asked how to get to Carnegie Hall, “Practice! Practice! Practice!” The same is
true for surgery. Just as pilots are not permitted to fly until there has been a clear
demonstration that predetermined criteria have been met or proficiency has been
achieved, surgery residents should achieve proficiency in the skills lab prior to entering
the operating room.
1
Nothing will dissuade an attending from passing down a case more than your bungling
basic tasks such as tying knots. Learn to tie two-handed knots proficiently before doing
them one-handed. It may not look as “slick”, but some attendings are critical of junior
house staff using one-handed techniques. When practicing suturing, be sure to follow
the curve of the needle. Grasp the tissues gently with your forceps. Learn to reset the
needle in your needle driver without grabbing it in your fingers. Become proficient in
releasing instruments with both hands. Deliberative practice does make perfect. Start
slowly and deliberately. Speed comes with frequent repetition of precise movements;
they become more and more automatic until you do not have to think about each one.
Be a good retractor-holder, and you will earn appreciation. Understand the importance
of your role and don’t take it as an insult. You can learn a lot from watching more
senior people operate, even observing a case you may not do yourself for another
several years. When you are retracting for a case, or operating the camera in a
laparoscopic case, observe
actively
. Watch the overall conduct of the case, listen and
try to learn the names of the various instruments and which instrument is used in which
circumstance. Observe how the instruments are held, and how the tissues, needles, and
sutures are manipulated. Ask a scrub tech to go over the names of instruments with
you quickly prior to or after the case if the instruments are not familiar to you. When
28
retracting, try to stand as still as possible. Try to anticipate how you can best help. If
you are not sure what to do, just keep doing exactly what you are doing, and don’t
move. Listen carefully when instructed. Don’t be afraid to ask questions at an
appropriate time. Let it be known that you are there to learn; not just putting in your
time, and not trying to catch up on your sleep. If you can not see the operative field,
don’t risk losing the surgeon’s view just to satisfy your own curiosity. Ask to see the
anatomy at an appropriate time, such as when things are going well, when waiting for
x-rays, or right after a stitch has been tied and cut and the surgeon is getting ready to
put in another. Try to correlate the anatomy you are seeing with the pictures in the
atlas you used. If it doesn’t make sense, ask the surgeon to explain it to you. Keep
asking until you get it straight. After each case, review the atlas once again to reinforce
what you have seen and done.
Observe
Find out who in your program is known to be the best
technical
surgeon; this may or
may not be the same person as the fastest or the best surgeon overall. Try to scrub on
that surgeon’s cases, or at least make it a point to observe his or her technique. You
will soon know which surgeons you want to imitate. The more you can learn about their
techniques, the better you will be able to visualize and practice those moves yourself.
Keep an OR Diary
In addition to the Case Log, develop an “OR Diary”, which serves a different purpose
than an operative log. After every operative case, take five minutes and jot down what
you learned during that case; write down “pearls” and the kinds of technical tips that
aren’t found in atlases. Making sketches to reinforce the surgical anatomy may be
helpful. Record the idiosyncrasies of the particular attending (e.g. suture preferences);
you can review this information in advance of the next case you do with him or her.
Make a note of what you think you did well operatively, and what you would specifically
like to improve the next time you do a similar case.
OPERATING ROOM STRATEGIES
It is important for all residents to scrub on as many cases as possible, and a
certain number of defined category cases.
4
Competing patient care obligations can pose
significant obstacles, but this must be a priority. Here are some strategies to help you
“get” cases:
• Read thoroughly on all assigned cases the night before. Even if you will only
assist on a case, try to read as much about it as possible. Review each patient’s
medical record, including the pre-operative workup and the indication for the
operation. There is something to be learned from every case you participate in; even
if you are doing 5 hernias in a day, use every case as an opportunity to learn
something new.
29
• Discuss the case with the attending at the scrub sink or in the lounge so that
she or he knows you have read about it and are prepared to do the case. Volunteer
a learning objective for the case; for example “today I would like to focus on
improving my dissection of the hernia sac.”
• Arrive early. Evaluate the patient in pre-operative holding and ensure that
everything is in order to go to surgery. Be in the OR ready to go even before the
patient is asleep. Show that you know how the patient should be positioned for the
case. Be gloved and gowned first so that you can immediately step to the position of
the operating surgeon (usually the right side of the patient) if invited.
• Don’t be shy. Ask if you may start the case, or if you can at least make the
incision. Find out the attending surgeon’s preference on incisions; some like to go
straight down to fascia with the first cut, while others prefer just cutting the dermal
layers with the knife, then cutting down to fascia with the electrocautery. Sometimes
just by starting the case, you will be allowed to continue on through the rest.
• Learn to anticipate. The major steps taken during any operative procedure should
be familiar to you, at least in general terms. Have an outline in your mind and try to
anticipate what the next step in the operation will be. This will make you a better
assistant and surgeon. Residents who actively participate in the operation are
rewarded by doing more of the case. It is very easy to Bovie your way through an
operation and have very little idea what you just did. Don’t let this happen to you!
• When assisting, be attentive and courteous. Even when not allowed to do a
case, show your preparedness by being an excellent assistant. Do not sulk or stop
assisting if you don’t get to do the case. There are still many learning opportunities.
See if you can anticipate the next instrument, the next move, etc. Demonstration of
your skill and interest may prompt opportunities for more significant involvement in
the future.
• Develop cordial working relationships. If the attendings know you well and are
relaxed around you, they are more likely to trust you. Ask questions about
technique. Have the surgeon demonstrate a particular stitch, or how to dissect in a
particular situation. Encourage attendings and senior residents to show off their
knowledge and skills.
• Extend your cordiality to the nurses and scrub techs with whom you work.
If they hand instruments to you to do little things like cutting or holding tissue, they
may eventually hand you the needle driver or scalpel, and the at
tending may not
take it away.
• Learn and remember the unique preferences of each attending. Use your
OR diary to record information about each surgeon’s techniques and procedures.
That way you will be prepared for the next time you do a case with that surgeon.
Some surgeons believe their way is the ONLY way, and will appreciate when you
recall their idiosyncrasies.
• Exude confidence appropriate to your level. Know that you are just as qualified as
most other residents at your level. You would not have been selected for your
residency if the staff did not feel you were qualified to be there and capable of
learning. Believe in yourself. Self-confidence breeds confidence from others.
30
• Remind yourself and others why you are there. If you make it very clear that
you are there to learn, it puts your superiors on the spot to teach. Show your
interest in each and every case by scrubbing as much as you can. Don’t spend
all
your time on the ward or in the ICU; you must learn to operate! Make time to scrub
cases that are above your level. Gain a reputation for being interested in learning
and highly motivated. If you love to operate, let it show! If you dread every single
case, find another specialty.
• Ask for feedback at the end of each case. Ask the attending to comment
specifically on what you did well, and what you should aim to improve next time.
If you feel you are not being allowed to do cases that you think you should be doing at
your level of training, talk to your Chief Resident, attending or Program Director. You
may need some additional work on certain skills. If you don’t ask what the problem is,
you will never know. Also realize that different residencies and even different hospitals
within the same program may have different policies about which cases are appropriate
for residents at a given level of training. Your Program Director will have information on
the number of cases that your cohorts have done, and you can ask him or her to assess
how your performance compares to your peers.
When a Case Is Not Going Well
Generally, do just exactly as you are told. If you see something that you can do to help
and not be in the way, do so. If you notice a problem that no one else has identified,
notify the appropriate person immediately. This is usually the surgeon, but sometimes it
may be more appropriate to tell the scrub nurse or anesthesia. Pay very close attention.
A crisis is not the time to assert your independence. If you get yelled at, remain calm
and try to correct whatever you are doing wrong. Some surgeons lose their cool when
problems occur, and you may be the most convenient target for their anger, even if you
did not create the situation. Don’t take it personally. Don’t get mad and walk out. Don’t
shout back or try to defend yourself, even if the accusations are false. Take a deep
breath, swallow hard if necessary, tell yourself to remain calm, and remember that your
first obligation is to the patient. Usually it is best to keep silent and just listen until the
surgeon calms down.
REFERENCES
1. Fried GM, et al. “Proving the value of simulation in laparoscopic surgery.”
Ann
Surg
2004; 240:518 –25.
2. Halsted WS. “The training of the surgeon.”
Bull Johns Hopkins Hosp
1904;
15:267.
3. Sachdeva A, et al. “A New Paradigm for Surgical Training.”
Current Problems in
Surgery
. Volume 48, issue 12, December 2011 Pages 854 – 968.

31
4. Surgery Residency Review Committee Program Requirements
http://www.acgme.org/acWebsite/downloads/RRC_progReq/440_general_surgery_0
1012008_07012012.pdf. Accessed 6.6.12
5. ACS/APDS. Surgical Skills Curriculum Information. American College of Surgeons:
Division of Education, 2008. http://elearning.facs.org/login/index.php. Accessed
2.10.10.
6. American Board of Surgery http://www.absurgery.org/. Accessed 6.6.12
7. McGaghie, W.C. (1999) “Simulation in professional competence assessment: basic
considerations, in”: A. Tekian, C.H. McGuire & W.C. McGaghie (Eds), Innovative
Simulations for Assessing Professional Competence (Chicago, Department of Medical
Education, University of Illinois at Chicago).
8. Society for American Gastrointestinal and Endoscopic Surgery (SAGES)
http://thesagesmeeting.org/. Accessed 6.6.12
32
Chapter 4: CARE AND FEEDING OF YOUR
SURGICAL EDUCATION
CORE COMPETENCIES
The ACGME requires residency programs to evaluate and document six core
competencies for each clinical rotation throughout residency.
1
These are: patient care,
medical knowledge, practice-based learning and improvement, systems-based practice,
professionalism and interpersonal skills and communication. Practice-based learning and
improvement requires that residents demonstrate a commitment to continuously
expanding their knowledge, are responsive to feedback and become dedicated life-long
learners. This also includes acquiring the ability to critically evaluate medical literature
and actively participate in the learning of others such as patients, families, and other
professionals. Systems-based practice refers to learning about the health care system
and resources in the system to optimize patient care. It also includes knowledge in the
areas of patient safety and advocacy. The ACGME Website
1
contains useful and broadly
applicable information for all residents, and for new interns in particular. The resident
evaluation process has evolved to a 360-degree evaluation. This means that staff
evaluations are included in overall assessment.
Seeking and Using Feedback
Feedback is the interactive process of providing learners with specific information about
their current performance that they can use to improve and reinforce future
performance. As such, feedback is absolutely critical to your learning as a surgical
resident and applies not just to your technical skills but also to the cognitive and
behavioral domains of competence. Feedback is most useful when it is timely, non-
judgmental, is based upon direct observations and consists of specific information.
Ideally you should be receiving feedback on a regular basis regarding your performance
in the OR, on the wards and clinics, in the ICU, and in conferences. Unfortunately there
are multiple barriers to effective feedback, so if this is not happening you must be
proactive in seeking feedback, particularly from attendings. After each operative case
you do, for example, find a time to ask the attending, “What do you think I did well in
that case, and what do I need to improve?” Alternatively, begin a self-critique and ask
the attending to comment. Make a point of meeting with the service chief at the mid-
point of any rotation and discuss your performance. There will be times when you know
that your performance in the cognitive domain falls short, for example when you are
asked a question that you know you should know the answer to, but don’t. Use this
opportunity to “double down” and ensure that doesn’t happen again.
Seeking and using negative feedback regarding your behavior is probably the most
challenging but may be the most valuable of all. If you have an uncomfortable or
negative experience with an angry patient, for example, ask an attending or senior

33
resident you trust and respect to review that scenario with you after the fact, to explore
ways in which you may have been able to handle that situation better.
Responding to Criticism
Inevitably during your training, you will be on the receiving end of criticism regarding
your clinical performance, attitude, or knowledge. When you are criticized, try to
evaluate the feedback as objectively as possible. Resist the temptation to take criticism
as a personal attack. Accept that a criticism may be valid, and you were simply wrong
and/or need to do something different in the future. Do not make excuses under any
circumstances. Consider how to use the feedback to build upon your skills.
Some criticism, upon considering its source and motivation, may appear petty or invalid
to you. If you believe that this is the case, remain calm and do not become defensive or
argumentative. A simple, neutralizing response could be “I will take that into
consideration and do better next time.” Learn from your mistakes, but don’t dwell on
them. Process the information, formulate a plan to incorporate the feedback into your
plan (or not), and move on.
ABSITE: THE AMERICAN BOARD OF SURGERY IN-TRAINING EXAMINATION
Disclaimer
The following collection of useful information has been gathered through the blood,
sweat, and tears of those who have gone before you. It has been road-tested by many
senior surgery residents. However, no one method of preparation will guarantee that
you pass the ABSITE. We hope that you find the following recommendations helpful
and use them to supplement the advice of your mentors. Good luck!
Introduction
The American Board of Surgery
2
annually offers to general surgery residency programs
the In-Training Examination (ABSITE), a multiple-choice examination designed to
measure the progress attained by residents in their knowledge of basic science and the
management of clinical problems related to general surgery.
2
Most programs use
ABSITE scores as one means to assess medical knowledge; if you do not achieve a
score above a certain percentile (usually the 30th percentile) you may be placed on
academic deficiency and prescribed a remediation program. On multivariate analysis,
scoring below the 35th percentile on the ABSITE at any time during residency was
associated with an increased risk of failing both the Qualifying and Certifying Board
Criticism may not be agreeable, but it is necessary. It fulfills the same
function as pain in the human body.
It calls attention to an unhealthy state of things.
-- Winston Churchill
34
examinations.
3
Many of your future employing institutions will ask you to indicate if you
have ever been placed on probation or academic deficiency when you apply for
credentialing, so this is an important issue and the exam must be taken seriously.
Each year, during the last week of January, general surgery residents of all levels take
the ABSITE. The exam is designed so that junior residents and senior residents take
different exams, If you’re in the PGY1-2 group, 60% of the exam content will be Basic
Science, therefore, be sure to read The Surgical Review: An Integrated Basic and
Clinical Science Study Guide.
4
You should consider it an invaluable adjunct to your core
surgery textbook. You can (and should) definitely read it cover-to-cover in the six
months before the ABSITE in January. It distills the encyclopedic quality of the core
textbooks down to essential facts that you can remember. The ABSITE for PGY3-5
residents has some basic science (20%), but 80% is on clinical management.
Your ABSITE score is reported in two ways: as a percentage of the questions answered
correctly and as a percentile to allow you to compare your score with your peers. When
your scores return, you will get feedback on which questions you missed. Ideally, you
should review your weak areas immediately, and then plan to focus extra attention on
those areas when studying for the following year’s exam. It is worth asking the
coordinator for a copy of the algorithm explaining how absolute percentages correlate
with the percentiles. Often the difference between achieving the 30th percentile and the
50th percentile is just a handful of wrong answers, so improving your performance is
not insurmountable.
Your program director should be able to give you advice on preparation, and there are
many review books available (see Appendix for recommendations). Also, talk with more
senior residents for recommendations for review books and question banks. Several
texts now have study question workbooks that are certainly worth considering, since
they help train your brain for taking this type of exam. If you have been reading
consistently, as suggested in Chapter 1, you should do fine. Try to get a good night’s
sleep before the exam. (Specialty residents rotating on your service may not have to
take the test, so arrange for them to take call the night before.) If you do poorly on the
ABSITE despite reading on your own, consider taking the Basic Science Review Course
offered each year by the Association of Program Directors (see Appendix). It’s a bit
costly to travel and stay in a hotel (not to mention the potential loss of vacation time to
do this), but it may be worthwhile if studying by yourself fails.
7 months before the Exam
(~ July 1
st
)
Core General Surgery Reading. Start out with the mindset that “I’m reading to
become a competent general surgeon.” You should plan on reading through at least
two core general surgery textbooks (in traditional bound or electronic format) during
the course of your residency. In the first two years of residency, it should be a core
basic science textbook (see bibliography in the Appendix); during the last half of your
training, the textbook should be one that deepens your foundation in surgery and
35
broadens your judgment. Review the table of contents and set a reading schedule for
yourself. Plan to finish each book by the end of the academic year. What you read will
be reinforced by your rotations on different surgical services. These texts are available
through SCORE
5
and can be accessed on most electronic devices.
4 months before the Exam
ABSITE Studying
The Fiser ABSITE Reviews
6,7
is a very popular text in large part because of its
portability. This book does a good job of addressing the breadth of the ABSITE topics;
however, there are some areas of inaccuracy where it relates to “current standard of
care.” The best thing to do is not rely on this review book as your only source of
information.
ABSITE Practice
There is no substitute for doing practice questions – lots of them. Hold off on intensive
ABSITE question preparation until September or October, however, as it is possible to
burn out/hit a wall when studying for a standardized test. The major basic science
textbooks (e.g. Sabiston
8
or Schwartz
9
) have question books that accompany the
textbooks. The questions (usually 10-20 per chapter) are designed to be used after
each chapter is read. You should be working on those all throughout the year. For
ABSITE practice, use question books directed specifically at ABSITE content. Some
options are listed in the Appendix.
Review Courses (see Appendix)
2 months before the Exam
At this point, you should plan to start going through your ABSITE Review book for the
second
time, and keep working through practice questions (lots of them). If you’ve
taken the ABSITE before, your score report should include a list of the topics/key
question themes that you missed from the year before. (The score report doesn’t give
the exact question verbatim, but it does highlight the key topic.) December would be a
good point to go over each of them line-by-line to make sure that you understand why
you missed them. It’s no secret that questions are repeated from year to year.
1 month before the Exam
A person probably is never “done” studying for a standardized test, but at some point
you must stop – stop studying to acquire
new
information, and focus your energy to
solidify what you already know.
In the month before the exam, a book like the General Surgery ABSITE and Board
Review
10
is a good resource. It is a book filled with one-line questions and answers on

36
core topics (both basic and clinical science) that helps you with rapid-fire review of the
things you’ve been studying for the last six months. Studying for the ABSITE is like
training for a marathon – the process starts long before race day. Remember, you’re in
training to become a competent general surgeon; anything you do to advance that
process will help you do well on the ABSITE.
WHO’S WHO IN THE HIERARCHY
Every residency program is a bit different, but all have some sort of hierarchy. Private
hospital training programs will differ considerably from universities, and the hierarchy in
single-hospital programs will be easier to decipher than in multi-institution programs. In
general, each department will have a Chair, Division Chiefs for the various surgical
specialties, and a number of attendings whose roles will vary considerably from one
place to another.
The Chair
The Chair of Surgery at a College of Medicine is the “Big Dog”, responsible for all
academic, clinical, and research activities of the department. The Chair manages the
faculty and support staff, and is responsible for the departmental budget. In many
institutions, the Chair of Surgery is also the Chief of Surgery at the major teaching
hospital, but this is not always the case. The Chair is ultimately responsible for the
quality of care, the spectrum of services offered, and may be responsible for the
practice plan. The Chair reports directly to the Dean of the College of Medicine.
The Chief of Surgery
The Chief of Surgery oversees all the surgical activities at one hospital and is ultimately
responsible for patient care that is delivered in the ORs, ambulatory surgical center,
SICU, and surgical wards and clinics. The Chief is responsible for compliance with
accrediting bodies (e.g. The Joint Commission
11
) and may be involved in institutional
quality initiatives. The Chief of Surgery reports to the Hospital Director.
Division Chiefs
The Division or Service Chief has a more narrow focus, and is responsible for the clinical
activities of attendings within that Division. The Division Chief may oversee activities at
several affiliated hospitals. He or she is responsible for the educational activities within
the division, and may be responsible for research activities within the division of an
academic institution.
“Academic politics is the most vicious and bitter form of politics,
because the stakes are so low."
-- attributed to Wallace Stanley Sayre (1905-1972)
37
The Program Director
The Program Director is responsible for seeing that residents meet the requirements of
accrediting bodies such as the ACGME
1
and the Surgery RRC
12
in addition to ensuring
that graduates will be eligible to sit the American Board of Surgery
2
examinations. They
oversee the rotation assignments and see that you have training in each subspecialty as
required by the Board. The Program Director will assign an advisor to each resident to
ensure that the resident receives timely feedback and advice on career decisions.
However, you are also free to ask any other attending to be your
informal
advisor or
mentor. Above all else, the Program Director is a resident advocate and as such should
make an effort to get to know each resident personally. Your Program Director is the
primary author of your residency summative evaluation and letter of recommendation.
A full description of the role and responsibilities of the Program Director is available on
the ACGME Website.
1
The Residency Coordinator
Once considered a glorified secretary, the Residency Coordinator now often has high-
level managerial and administrative skills in order to ensure the residency program
meets accreditation requirements. A Coordinator reports to the Program Director, and
typically views him or herself as filling multiple roles, including counselor, advocate, den
mother, social planner, cheerleader, arbitrator and data analyst. Keep in mind that the
Residency Coordinator is on your side and can be a tremendous resource for you. Do
not feel intimidated or threatened by confiding in this person. Most Program Directors
view the Coordinator as the program’s most valuable resource. So treat the Coordinator
respectfully at all times.
House Staff Hierarchy
The house staff hierarchy is determined by your training year. There are sometimes
specific types of operative cases or procedures associated with each year (i.e. interns
do hernias, Chief Residents do Whipples, etc.) but this is changing as programs adopt a
more flexible, proficiency-based approach to training. There are also specific tasks and
rotations assigned by year. A house staff team
is
hierarchical, and you should pay
attention to the “chain of command” when fulfilling your clinical duties. For example, if
as an intern you consistently inform an attending of non-urgent patient problems but
neglect to let the junior resident or Chief know, you will be
persona non grata
pretty
quickly. No one likes to be caught off guard. On the other hand, if an attending asks
you to do something, clearly that task must assume some priority in your list of to-dos.
Remember, trouble rolls downhill, and unnecessarily and consistently jumping the chain
of command in a non-emergent situation is a good way to make it roll harder and
faster.
MENTORS
The dictionary defines a mentor as “a wise and trusted counselor or teacher.” A mentor
also can be referred to as a sponsor, which is defined as “one who assumes
38
responsibility for a person or thing.” The first criterion for a mentor is someone who is
wise, which means not only knowing the facts, but also knowing what is true, right, and
lasting. They have experience, common sense, and good judgment. This usually means
someone senior to you in the surgical hierarchy. The relationship should be mutually
beneficial, and evolve over time until you become a valuable colleague to the mentor.
Why You Need a Mentor
Having a mentor is absolutely essential for you to advance through the academic ranks.
A mentor can serve many useful functions to make your professional life successful and
progress easier. They can offer advice on everything from surgical techniques to solving
a tricky clinical situation, to useful references. A mentor should help you to understand
the hierarchy and “chain of command” in both your own program and the field of
surgery. You must learn whom to trust, and whom to avoid. Mentors can promote you
by nominating you to speak at conferences, publish papers, and become involved in lab
research or clinical trials. Mentors can give you thoughtful critiques on your clinical work
and your writing. A mentor will alert you to useful meetings and conferences, both for
their political as well as their educational aspects. Mentors can ensure that you receive
challenging assignments that will showcase your talents. It will enhance your reputation
to be associated with and accepted by a good mentor. A good mentor will help you to
stay focused and avoid over-committing your time to activities that will
not
enhance
your career aspirations. A good mentor will also serve as a role model for you in terms
of style, demeanor, and dealings with patients and others. Simply having the mentor’s
support can be a protective measure if you find yourself in a hostile environment.
Contacts and networking are keys to success in the academic environment. Therefore
you must actively seek out a mentor for yourself.
Finding a Mentor
In your lifetime you will almost certainly have more than one mentor, as your interests
and priorities will change over time. It is helpful to have at least one mentor who has a
solid reputation within your own institution and is a more senior faculty member, but
not necessarily a member within your department. The ideal candidate should have
strong contacts within the national surgical societies and may be actively involved in
research. This is particularly important if you are planning for an academic career. It
will probably take some time to identify someone and develop a working relationship.
Keep in mind that you are not the only one who benefits from the association with your
mentor; there is a strong synergism between good mentors and their protégés. When
you are successful, your mentor’s stature among his or her own colleagues is enhanced.
Some of the most lauded surgeons are department chairs who have promoted their
own faculty so well that they have also become department chairs. Recognize that your
mentoring needs are likely to change over the course of time. You may find it useful to
build a pool of mentors – maybe even in different institutions or disciplines – to help
with different aspects of your professional life as your career evolves.
13
39
If your intent is to enter private practice, you should seek a mentor who is in that
type of practice. It is easier to ask someone with whom you have some rapport to
help you find a job, set up practice, and choose between solo, group, or HMO
practice. Another option to help evaluate job opportunities is to use the AWS
Directory to find someone practicing in your area or the area to which you may wish
to relocate. A large number of women in AWS are in private practice, and most are
willing to offer advice to younger women coming up through the ranks. While the
prospect of going solo may seem daunting, it is not nearly as difficult as it seems at
first glance. Useful resources on HMOs and private practice are available in the AWS
Career Development Resource
14
on the AWS Website.
REFERENCES
1. Accreditation Council for Graduate Medical Education (ACGME)
http://www.acgme.org/acWebsite/home/home.asp. Accessed 6/6/12
2. American Board of Surgery http://www.absurgery.org/. Accessed 6.6.12
3. De Virgilio C et al. “Predicting performance on the American Board of Surgery
qualifying and certifying examinations: a multi – institutional study.”
Arch Surg
2010;
145 (9): 852 – 6
4. The Surgical Review: An Integrated Basic and Clinical Science Study Guide. Atluri
P. et. al, 2005 published by Lippincott Williams.
5. Surgical Council on Resident Education (SCORE) Curriculum.
https://portal.surgicalcore.org/. Accessed 6.6.12
6. The Senior ABSITE Review. Steven Fiser, 2006. Lippincott Williams & Wilkins
7. The Practice ABSITE Question Book
Steven Fiser, 2010. Lippincott Williams &
Wilkins
8. Sabiston Textbook of Surgery. Townsend, Beauchamp, Evers, Mattox. 2012. 19
th
edition. Saunders. (Hardcover)
9. Principles of Surgery, 9
th
Edition. Seymour I. Schwartz, et al., 2009. McGraw Hill
Text
10. General Surgery ABSITE and Board Review (Pearls of Wisdom) Matthew J. Blecha
and Andrew Brown
11. The Joint Commission http://www.jointcommission.org/ Accessed 6.11.12

40
12. Surgery Residency Review Committee Program Requirements
http://www.acgme.org/acWebsite/downloads/RRC_progReq/440_general_surgery_0
1012008_07012012.pdf. Accessed 6.6.12
13. American Heart Association Mentoring Handbook
. Second Edition, November
2008. AHA Early Career Investigator/Clinician Task Force
14. Association of Women Surgeons
Career Development Resource
,
https://www.womensurgeons.org/home/Career_Planning.asp. Accessed 6.7.12

41
Chapter 5: PROBLEMS AND PITFALLS
WHEN YOU MAKE A MISTAKE
You will make mistakes. Everyone does. Some will be little mistakes of no consequence;
others may be life-compromising for a patient. NEVER try to cover up mistakes you
make. In these situations do the following:
• Get help.
• Tell the truth as you know it. State only facts. Do NOT offer excuses or try to
blame someone else. Keep explanations under wraps unless specifically asked
for them. DO NOT LIE!
• Be careful what you say of others; it will reflect just as much on you.
• Accept responsibility when it lies with you. This is especially important when
dealing with medical students and more junior residents. If you tell them to
do something and problems ensue, accept responsibility. If others dump on
you when you were really not involved, take them aside and discuss it in
private. Make it clear that this behavior is unacceptable.
• Ask for an explanation if you don’t understand what you should have done
differently and why. However, you may need to wait until any hot tempers
have cooled.
WHEN A PATIENT DOES BADLY
There is no question that surgery is an enormously rewarding career. However, no
specialty is as acutely aware of the relationship between what we do (or fail to do) for a
patient, and the outcome. When a patient has a complication, it can be emotionally
challenging for the operative surgeon. When a patient dies, it can be devastating. When
this happens to your senior colleagues be supportive, and do not criticize or second-
guess their decision-making. Some day it will happen to you. When it does happen to
you, recognize that it is
entirely normal
to experience regret, guilt, sadness, anger, and
a host of other “negative” emotions in response to a patient’s morbidity or mortality. It
is common to question your own abilities. It is okay to hole up in a bathroom and cry
for a few minutes if you must. While it is permissible to shed a tear in private you must
not, however, allow yourself to become psychologically paralyzed by a complication or
poor outcome. If you feel this is happening, seek counsel from a more senior surgeon
to help you put a situation in perspective. If you are more comfortable seeking help
outside the department go to Employee Health for assistance.
Good judgment comes from experience;
experience comes from bad judgment.
-- Will Rogers
42
Morbidity and Mortality Conference
One of the great and hallowed traditions of surgery is the practice of critically
evaluating our practice, at M&M Conference. A proper M&M presentation includes a
discussion of the indication for the operation, the patient’s course including specific
disclosure of any factors that may have contributed to the complication, the
complication itself, how the complication was recognized and managed, and the
outcome. An effort should be made to classify all M&Ms as “error in diagnosis”, “error in
technique”, or “error in judgment”, and to discuss what could have been done
differently to have prevented the complication. A complication blamed on “nature of
disease” is suspect and will not be as educational. The most valuable M&M case
presentations are the result of brutal honesty and introspection where the surgeon
assumes full responsibility for the complication and seeks truly to share what he or she
learned. It’s not unlike a confessional and can actually be a cathartic experience.
Presenting your first M&M is an anxiety-provoking experience, but remember that the
point is to recognize errors so that they won’t happen again. It is
not
the objective to
punish or publicly humiliate you for an error. Always discuss any M&M presentation with
the surgeon of record well before the conference; nothing will infuriate an attending
more than hearing you present an alternate view of reality to a group of colleagues.
SUBSTANCE ABUSE
The prevalence of substance use disorders among U.S. physicians has been estimated
to range from 10% to 15%, and one study has suggested a higher incidence in women
surgeons.
1
Studies have also linked an increased likelihood of medical and surgical
errors to surgeons who are depressed, and who abuse alcohol and other drugs.
2
However, the stigma of reporting oneself as having an alcohol or other drug problem is
so great in the medical profession that impaired surgeons (as with other physicians)
are, in general, extremely reluctant to admit that they have an alcohol or drug problem.
Most medical boards still require physicians to indicate whether or not they have a
history of drug or alcohol abuse on licensure applications, and the medical profession,
in general, still seems to be in a state of denial regarding the unusually high incidence
of drug and alcohol abuse among physicians when compared to the general public.
NEVER consume alcohol when on call, even when taking call from home. Even if you
have “only one” beer, you will smell just like you drank a case. Additionally, studies
have shown that alcohol consumption degrades surgical skills among surgeons even
well into the day following alcohol intake
.
Most institutions have a confidential hotline to
report colleagues who are impaired on duty.
If you suspect a fellow resident has a substance abuse problem, you must bring this to
the attention of the Program Director, who is obligated to treat your concern
confidentially. A “head in the sand” approach is a disservice to the resident and,
ultimately, to the public. If
you
believe you may be dependent upon drugs or alcohol,
discuss this with your personal physician. As terrifying as this may be, it will be much

43
better for you to get out in front of this problem than to be “found out” in some
ignominious way or as a result of harm to a patient or yourself. The goal ultimately
must be to identify and rehabilitate impaired physicians, not to punish them. You can
also go directly to the Employee Assistance Office in your institution. If you do need
treatment, this will be treated as confidential and your Program Director is only entitled
to know whether you are fit (or unfit) for practice, not the specific details of your
diagnosis or treatment (see Resident Rights at the end of this chapter).
SYSTEMATIC DISCRIMINATION
Discrimination: Definitions
Gender discrimination is defined as a situation in which a superior uses your gender
as the basis for a negative decision that affects your career. It may or may not be
combined with sexual harassment. Examples of this would be if your department
pays a woman less than a male physician for the same staff position or consistently
chooses the male residents over the female residents for career advancement
opportunities.
Under federal law it is illegal to discriminate in the workplace against a person based
solely upon their race, color, religion, sex, national origin, age or disability. Harassment
based upon these characteristics is illegal, and retaliation against an individual for filing
a complaint of discrimination is prohibited. Protection extends to hiring and firing
actions, compensation, assignment, and recruitment.
What Discrimination is NOT
It is equally important for you to understand what does
not
constitute
discrimination. Affirmative action plans aside, your employer or Department Chair is
rarely under obligation to hire or promote you over an equally qualified physician
solely to have a woman/black/Muslim in the department. When interviewing for a
residency position or job, it is not permissible for the interviewer to inquire about
your marital status or if you plan to have children. However, if you are applying for a
residency position as part of a couples match, then questions about your spouse/
partner will be legitimate. If you
volunteer
that you are planning to take an
extended leave after each child, it should not be used as a criterion for refusal of
employment, but extended absence from residency training could impact your timely
promotion from one year of training to the next and your ability to graduate the
program on time. If you plan on taking an extended leave after each child when you
are in practice, thereby failing to achieve the requisite academic milestones or RVU
(Relative Value Units) benchmarks, you should be aware that this decreased
academic and/or clinical productivity can be used as a criterion for refusal of
promotion, and/or a reduction in salary.
44
SEXUAL HARASSMENT
Definition
Sexual harassment is defined as any unwelcome sexually-oriented behavior,
comment, demand, or physical contact made to or about you that interferes with
your work, creates a hostile or offensive working environment, or that is made for
the purpose of threatening your position or humiliating you. A blatant example is
when an attending demands sexual favors and refusal will adversely affect your
evaluations. A less obvious case would be where you are in the OR lounge and
colleagues start telling dirty jokes or stories with the express intention of making
you uncomfortable.
Title VII's
3
broad prohibitions against sex discrimination specifically cover:
• Sexual Harassment - This includes practices ranging from direct requests for
sexual favors to workplace conditions that create a hostile environment for
persons of either gender, including same sex harassment. (The "hostile
environment" standard also applies to harassment on the basis of race, color,
national origin, religion, age, and disability.)
• Pregnancy-Based Discrimination - Pregnancy, childbirth, and related medical
conditions must be treated in the same way as other temporary illnesses or
conditions. Note that as a woman you can not be refused a position because you
may be exposed to agents that would affect the health of any baby you might
carry. This means that you can not be refused privileges for any case that might
require fluoroscopy or use of a teratogenic agent (though you should assess the
risks for yourself and take appropriate precautions).
For Women: What Sexual Harassment is NOT
Surgery is a predominantly male profession (although this is slowly changing) so you
need to understand what is
not
harassment. You may be exposed to off-color stories or
jokes from time to time. If they are not directed at you, try to ignore them and change
the topic. If you find such jokes demeaning, speak up and ask that such comments not
be made in your presence. You can point out that it is inappropriate to tell such jokes in
front of individuals who may not feel comfortable voicing their disapproval (e.g., if the
comments are embarrassing to medical students or ancillary female personnel). Try to
do so without being antagonistic or confrontational. Be very clear about this, and do not
give any double messages while trying to be tactful.
In some cases, an older man will call you “dear”, or pat you on the shoulder. This
may seem paternalistic and demeaning, but it may be how he was raised to treat
women; he may perceive his actions as being polite and respectful to your
femininity, rather than offensive. Don’t confuse courtesy with chauvinism; nothing
irritates a guy more than a woman who gets angry when he opens the door for her.
In most cases this is not harassment. Additional information can be obtained in a
separate pamphlet on sexual harassment, which is available from AWS.
45
Dealing with Discrimination or Sexual Harassment
All that being said, how should you deal with a presumed case of sexual harassment
or discrimination? First, after an incident has occurred, sit down, take a deep breath
and try to look at the situation objectively. Record the facts of what happened in as
much detail as you can recall. Review the problem with an objective outsider.
Decide if the episode really was one of discrimination or sexual harassment. It may
be easier for you to blame your lack of promotion on bias rather than the fact that
another resident actually did a better job.
If you decide that this was indeed a case of discrimination or sexual harassment,
you have several options:
• Familiarize yourself with the discrimination and sexual harassment policies at
your institution.
• Document all incidents at the time they occur; a “memorandum for record”
document is appropriate. Note the presence of witnesses. Use discretion when
discussing the incident or behavior with colleagues. Use your personal e-mail
account to communicate sensitive information, as your supervisor has the right
to access your hospital or institutional e-mail account.
• Make an appointment with your Program Director to discuss the incident. If
the problem is with the Program Director, talk this over with a trusted staff
member or mentor and let him or her help you. Be prepared to listen. There may
be other perspectives that you have not considered.
• Be prepared to support yourself with documentation, such as statements from
witnesses of specific events, or letters of recommendation from other coworkers
(including other residents or nurses). Prepare yourself to be disappointed. Many
men and women you consider your friends are not willing to stick their necks out
if they think it will be detrimental to their own careers. Come to meetings with a
copy of your CV and any additional materials that you feel would bolster your
case, such as evaluations from other physicians on staff.
• Record all discussions after any meeting. If specific promises were made,
document them as well as any other comments made that you thought were
significant. These notes may have legal importance if the matter proceeds as far
as arbitration or court. If possible, consider having someone you trust in the
room with you.
• If you feel your needs are not met within your department there are several
options. Check the bylaws, rules and regulations of your institution. Generally
each institution will have an Equal Opportunity Office with staff trained to offer
advice. Your Human Resource Department will know how to contact the
appropriate staff. Resident unions or the Residency Housestaff Office may also
be supportive. For residents, the chain of command to report a
n incident should
be 1) Program Director, and then 2) Associate Dean for GME. If there is a need
to go outside the institution, residents should go to ACGME
4
rather than the
Residency Review Committee (RRC).
5
46
The chain of command for students is 1) Clerkship Director, then 2) Dean of
Student Affairs. If the problem is not being handled appropriately and it
interferes with your surgical education, reporting to the RRC may be appropriate.
Remember that you may be jeopardizing your program (and your training) by
such reporting, however, your complaint may prevent another resident from
having to deal with the same problem in the future. If you are considering
leaving your program, you might try to obtain a position in a different training
program prior to reporting to the RRC.
• Legal action should be a last resort, but is a real consideration if you have
serious, documented, and legitimate complaints that are not adequately
addressed by your program or institution. If you are threatened or pursued
outside the physical space of your institution, it is time to seek legal advice.
Find an attorney who is familiar with employment law particularly as it relates to
discrimination and harassment. For help finding such a person, contact the Equal
Employment Opportunity Commission (EEOC)
6
or the National Organization for
Women (NOW).
7
Both of these organizations have legal staff who can help with
these problems. Merely the threat of legal action often will cause a problem to
disappear, but don’t “cry wolf.” If you initiate a lawsuit, be prepared to see it
through to the end.
• Prepare for a backlash and for the broader consequences of your actions.
Fellowships, staff appointments, partnerships, and most jobs in our profession
are gained through the “old boy/girl network.” If you antagonize too many
politically powerful people with complaints or a lawsuit, you may find yourself
winning the battle and losing the war. Your best defense against the rumors and
innuendoes that can accompany such problems is to state your case in the most
objective way.
• If you find yourself on the other end of a discrimination or harassment
complaint, you have the right to request documentation for any incidents that
are being held against you and to respond to any complaints [see Resident
Rights]. Do not accept a statement that “a complaint was made, but I won’t tell
you by whom, to protect their privacy.” This type of secrecy is not permissible if
it affects your career.
REPRODUCTIVE ISSUES
Pregnancy
Many women surgical residents choose to begin a family during residency. Some
residents spend one or two years doing research during their residency and choose to
have a child during that time. Others choose to have a child during the clinical portion
of their residency. A pregnant resident was a rarity in the past; this is no longer true. It
is an undeniable fact that the years a woman is typically in surgical residency happen to
coincide with her last years of peak fertility. That said, it is incumbent upon a woman
resident to assume some responsibility for family planning.
47
Before planning a pregnancy, investigate your institution’s maternity leave and childcare
options. Most likely, vacation time will be used as part of your maternity leave, so learn
the rules at your institution early in the process. The graduate medical education office
should have information available on these topics. It also may be helpful to discuss
them with a respected attending or friend whom you can trust.
It is no longer tolerated for women surgical residents to receive verbal abuse from
colleagues or attendings for getting pregnant. If you do feel ridiculed or mistreated, you
should speak with the Program Director immediately.
Issues to Consider When You’re Pregnant
• Safety: Review your institution’s Environmental Health and Safety Policy on
radiation exposure. It is safe for pregnant women to continue to perform
fluoroscopy and interventional procedures with proper shielding. Some institutions
will require a pregnant woman to wear a radiation detection badge on her abdomen
to ensure limited exposure to the fetus.
• Health Benefits: Contact your health care provider to determine which OB/GYN
group(s) is/are covered, and your financial responsibility.
• Sharing Your News: Deciding when to share the news that one is expecting is a
very personal decision. For some, waiting until the second trimester (13 weeks),
when the risk of miscarriage is substantially reduced, is the best option. Be sure to
give your Program Director and colleagues ample time to prepare for your absence
during maternity leave. You should inform your Program Director and/or Chair early
in the pregnancy so that rotations can be organized to everyone’s advantage. The
issue of call coverage while you are out can be tricky. With current work hour
restrictions, it is likely not possible to offer to take extra call before or after your
maternity leave. There may be some other way to “repay” your fellow residents; for
example, by offering to cover an unpopular clinic assignment.
• Taking Care of Yourself While Pregnant: Be sure to carry snacks in your white
coat, eat in between cases, drink plenty of fluids, rest/nap, and sit or elevate your
legs whenever possible to care of your pregnant body. Wear good support hose to
avoid varicose veins and help with leg edema.
• Maternity Leave: A nationwide policy for maternity leave for residents currently
does not exist. Each institution has its own policy on maternity leave, so become
familiar with it. The AWS put forth a statement in 2002 that encouraged each
surgical program to provide six weeks paid maternity leave for residents.
8
Discuss
plans for maternity leave with your Program Director well in advance of your due
date. The American Board of Surgery (ABS) published the following statement in the
Booklet of Information, 2005
: “For documented medical problems or maternity
leave, the ABS will accept 46 weeks of surgical training in
one
of the first three
years, for a total of 142 weeks during the first three years, and 46 weeks of training
in
one
of the last two years, for a total of 94 weeks during the last two years.”
9
48
If, for unforeseen reasons, you do not meet these criteria, you may have to repeat a
year or a portion of a year to qualify to take your Boards.
• Board Exams: Surgical residents who miss an extended part of their training as a
result of pregnancy (or any other reason) may not meet the requirements to sit the
American Board of Surgery Exams at the end of residency. This is not a problem if
only the normal six weeks of maternity leave are needed.
• Paternity Leave/Adoption: As indicated above, there are no uniform guidelines
for time off following the arrival of a new baby (including adoption). It would be
reasonable to expect consideration similar to maternity leave. It is very important to
have these discussions as early as possible in the process so that expectations are
clear and plans can be made.
• Childcare: Begin researching childcare options
early
, even as soon as you find out
you are pregnant; there are frequently waiting lists. Institutions may offer childcare
services at the hospital, and some may subsidize the cost of childcare for residents.
Ask colleagues, attendings, and friends who have children about available options.
Choose the best childcare that you can afford. Knowing that your child is safe and
well-cared-for will bring security and peace of mind. This can not be overstated. It is
hard to do your best at work if/when you are distracted by concerns regarding your
family.
• Returning to Work: Returning to clinical work after maternity leave can be quite
difficult. Consider beginning with a rotation that has a lighter schedule to make this
transition easier. If you have to work late or are unable to leave the hospital before
your child is in bed, consider asking your spouse/partner or sitter to bring the child
to the hospital for a quick visit. Visits on weekends and holidays are also helpful.
• Acknowledge conflicting feelings surrounding pregnancy/parenthood and being
a resident. Women in particular are prone to guilt feelings that they are failing to be
a good mother or a good resident, or both. Seeking help early from either a mental
health provider or someone you trust can really help ease the transition and help
you develop reasonable expectations for yourself and others.
• Breast Feeding: The American Academy of Pediatrics recommends that infants be
breast-fed through the age of six months, at a minimum. This can be difficult but it
can be done. If you choose to nurse your baby, explore the options available for you
to pump and store breast milk at your hospital. Every institution should have a
policy and a private room where you can use a breast pump.
Fertility
We are frequently asked for advice regarding the optimal time to have children during a
surgical career. There are obviously many options extending from medical school (or
before), during residency (including lab time), during fellowship, as a new attending or
later. The issue of fertility must be seriously considered in making this decision. The
longer you delay having children, the more likely the process may be complicated by
fertility issues. It is important that you discuss this risk with your physician.

49
PERSONAL RELATIONSHIPS
We are all human, and sex is one of the basic human desires. Additionally, surgical
residency can be a time of great personal vulnerability. We’ve all been there. But the
workplace is a potentially hazardous environment in which to play the dating game.
Your education and ultimately your career depend to a large extent upon the good
will of your attendings and senior residents. If you wish to be evaluated on the basis
of your surgical skills and talents, you should keep your social life to yourself and
ideally keep it outside the hospital. People love to gossip, and speculation about
your love life will not enhance your career.
Because long work hours may hinder meeting eligible mates outside the hospital,
there is a temptation to seek affection among your peers. Getting involved with
anyone in your program or department can have repercussions, however,
particularly if the relationship ends badly. If it doesn’t work out, you will still have to
see this person every day. If you wear your heart on your sleeve, your work, and
perhaps your career, may suffer. Note that the American Medical Association
considers even consensual amorous relationships between those in a position of
responsibility and their students or trainees to be unethical.
Do look for someone outside the Department of Surgery. There are many appealing
potential partners who are not surgeons! Meet people in other departments and
outside of medicine altogether. Continue to participate in the activities that you
enjoyed before you became a surgery resident. This is only one of many important
reasons to maintain a life outside of the hospital.
Choose relationships carefully. Seek personal relationships that help to sustain you
without exacting undue drama.
In any case, a number of successful lifelong partnerships began in the workplace
and if you do decide to date another resident or an attending, or anyone else in the
hospital, you would not be the first (or last) resident to do so. Keep your in-hospital
dealings with each other strictly professional. Be discreet, avoid rotations together,
and keep your personal relationship out of hospital view.
Peace hath her victories
No less renowned than war.
-- John Milton,
To the Lord General Cromwell
50
CONFLICT RESOLUTION
Conflict is natural and it is inevitable that you will encounter some during the course
of your residency. Mastering conflict constructively will help you immensely in many
aspects of your personal and professional lives. Here are some general principles
governing constructive conflict resolution:
• Commit to resolving any conflict constructively. Direct your emotional
energy toward positive problem-solving rather than whining or complaining.
• Manage your anger. Recognize when you are angry and direct it appropriately.
Angry outbursts never contribute positively. Understand that your emotions may
cause you to make an inaccurate judgment about the intent of the other person.
• Do not seek “victory”. Learn to listen, and try to understand your opponent’s
perspective. Focus on doing right not being right.
• Assume the best. Give other people the benefit of the doubt.
• Watch your tongue. Words can inflame conflict unnecessarily. Before
speaking, ask yourself: is it true, is it kind, is it necessary to say?
• Speak the truth. Do not confuse the truth with your opinion.
• Be respectful. Treat others with dignity.
• Attack the problem, not the person. Do not disparage the character of
another person.
• Deal with specific issues and behaviors, not sweeping generalizations.
“You are a liar” is not a helpful opening gambit in dealing with a colleague.
Better would be: “I see you wrote something in the chart that doesn’t completely
align with my recollection of events. Can we talk about that?” or “Help me
understand why you made this decision/said this/did that.”
• Deal with conflict directly. Go to that person. It is cowardly to go behind a
person’s back and complain or gossip about them. Don’t do it.
IF YOU THINK YOU WANT TO QUIT
Surgery is not for everybody. One in five residents will change to another career.
10
If you find you are miserable and dreading coming in to the hospital every day, it’s
possible that you need to reconsider your specialty choice. A decision to leave
surgical training is one that should not be made lightly, or on a “bad” day such as
when a case has gone extraordinarily badly or a patient has died. Seek counsel
from your mentor, and from those you trust outside the hospital.
RESIDENT RIGHTS: PROTECTING YOURSELF FROM DISMISSAL OR
DISCIPLINARY ACTION
About one in five residents will have a significant performance deficiency in their
training but most of these will be successfully remediated. In an ideal world, you will be
treated fairly, given timely feedback and your Program Director will always do the right
51
thing. However, we do not live in an ideal world and it is worth informing yourself and
taking responsibility for your own success. If you are struggling and are concerned
about your future in the program, there are certain actions that you can take to
improve your performance and avoid being terminated or placed on probation:
• Clarify expectations for EACH rotation at the onset as these expectations may
differ from one service to another (and from one attending to another).
• Read the Surgery RRC Program Requirements
5
so that you know the educational
expectations and standards for your training.
• Read the American Board of Surgery
8
eligibility requirements.
• Ask for feedback at least weekly (or after each case); reflect upon it and act
upon it.
• Respond promptly to any complaint from a patient, nurse or other health care
professional
• Take all hospital policies seriously, particularly those relating to patient
confidentiality and timely completion of medical records. Almost every future
credentialing authority will ask you if you have ever been placed on probation /
academic deficiency. If your hospital places you on probation for not completing
discharge summaries in a timely manner you will need to declare this for the rest
of your life.
• Most programs require that you pass all USMLE examinations by a certain time in
your training. Know the rules for your program and apply for the exams well in
advance of the deadlines.
• Read your written evaluations at regular intervals (at least quarterly). Usually
these will not be anonymous. If you receive a negative comment on your
evaluation, you should approach the evaluator for suggestions on how to
improve your performance.
• You have a right to see your resident performance file. Read it so that you know
what it contains. If you see something in your file that is not true, discuss this
with your Program Director.
There are important differences between the detailed documentation required by
ACGME and the minimum legal requirement, which is less stringent. The courts say that
as long as the individual was provided with “
notice and an opportunity to cure and the
faculty decision is conscientious and deliberate,”
they will not second-guess decisions
to place a resident on probation or to terminate him or her from the program.
11
If you
are being placed on probation or academic deficiency, you should receive a formal letter
(by ACGME standards, but the law says that this information can be communicated
verbally) outlining the reason for the decision/what you need to do to correct the
deficiency and a time frame for reassessment.
This is your fourteenth amendment right
to due process
. You may be asked to sign this letter on receipt. You are NOT required
to sign it and should only do so if the sole purpose of your signature is to acknowledge
receipt of the letter without indicating agreement with the content. DO NOT SIGN
ANYTHING ADMITTING CULPABILITY without legal advice.
52
ACGME requires that your program provide four months notice of either dismissal or a
failure to promote unless immediate disciplinary action is mandated by misconduct.
12
By
definition, misconduct is behavior that is wrong; that one knows (or should know) is
wrong and therefore will not be cured by remediation. Misconduct includes such “fatal
flaws” as dishonesty, covering up mistakes thereby putting patients at risk,
inappropriate touching, patient abandonment, and criminal activity. If you are accused
of misconduct, the incident should be investigated, and a report generated that
considers extenuating circumstances, if present.
13
In cases of either probation or
dismissal you can appeal through the office of the Associate Dean for Graduate Medical
Education at your institution. Institutional Grievance and Appeal Policies are usually
posted on the GME Website and distributed to all new residents at orientation.
Resident Rights: Protecting Your Right to Confidentiality
The Americans with Disabilities Act (ADA)
14
mandates that a residency program makes
reasonable accommodation to ensure that a resident with a disability or chronic illness
can complete the curriculum; however the resident
must
ask for accommodation
before
a performance deficiency occurs. If you do not disclose, for example, that you have
dyslexia until after you have failed the ABSITE several times, you are not entitled to
accommodation for your disability. In addition, the ADA limits when a psychiatric
evaluation can be required and is usually restricted to decisions about “fitness to
practice”. A doctor-patient relationship does not, and should not exist between a
resident and a Program Director; therefore if there is a fitness to practice concern
necessitating a referral to employee health by your Program Director, the medical
assessments must be kept confidential and separate from your academic file. After such
evaluations the Program Director should be informed that appropriate follow up is
occurring, but not specific medical details. Future employers should not be told about
impairment except to the extent that it involved misconduct (or lack of fitness for
practice) that resulted in employment action. However, certain licensing authorities may
ask about a history of impairment. If asked, always answer truthfully.
REFERENCES
1. Oreskovich MR et al. “Prevalence of Alcohol Use Disorders Among American
Surgeons”
Arch Surg
. 2012;147(2):168-174
2. Buhl A, Oreskovich MR, Meredith CW. “Prognosis for the recovery of surgeons
from chemical dependency: a 5-year outcome study.”
Arch Surg
. 2011;146
(11):1286-1291.
3. Title VII. http://www.eeoc.gov/laws/statutes/titlevii.cfm Accessed 6.11.12
4. Accreditation Council for Graduate Medical Education (ACGME)
http://www.acgme.org/acWebsite/home/home.asp. Accessed 6/6/12
53
5. Surgery Residency Review Committee Program Requirements
http://www.acgme.org/acWebsite/downloads/RRC_progReq/440_general_surgery_0
1012008_07012012.pdf. Accessed 6.6.12
6. Equal Opportunity Commission (EOC) http://www.eeoc.gov/ Accessed 6.7.12
7. National Organization of Women (NOW) http://now.org/ Accessed 6.7.12
8. Association of Women Surgeons
Family Leave Policy for Residents
https://www.womensurgeons.org/aws_library/ResidentPolicy.pdf. Accessed 6.6.12
9. American Board of Surgery http://www.absurgery.org/. Accessed 6.6.12
10. Yeo, H; et al. “A National Study of Attrition in General Surgery Training: Which
Residents Leave and Where Do They Go?”
Ann Surg
. 2010; 252 (3) : 529-536
11. Richard K; et al. “Does ‘Fair Hearing’ = ‘Due Process’ in Residency Programs?”
Health Lawyer News
December 2006.
12. Accreditation Council for Graduate Medical Education (ACGME)
http://www.acgme.org/acWebsite/downloads/RRC_progReq/440_general_surgery_0
1012008_u08102008.pdf. Accessed 6.7.12.
13. Sanfey, H. et al. “Pursuing Professional Accountability: An Evidence Based
Approach to Addressing Residents with Behavior Problems.”
Arch Surg
. July 2012.
14. American with Disabilities Act (ADA) http://www.ada.gov/pubs/ada.htm.
Accessed 6.7.12

54
Chapter 6: TAKING CARE OF YOURSELF
BASICS OF SELF-PRESERVATION
With the initiation of the 80-hour work week by the Accreditation Council for Graduate
Medical Education (ACGME), surgical residency has become more tolerable and certainly
less time-consuming. A limit on the work week has provided more time for residents to
focus on self-directed reading outside of the hospital and to take care of themselves.
However, 80 hours is still a lot of time, and the hours in the hospital can still be
stressful and overwhelming.
Sleep
Getting enough sleep is important, as studies have shown that the ability to make
appropriate decisions worsens with sleep deprivation. While in the hospital on call
overnight, if you have a few hours or even a few minutes of downtime, use it to catch
up on some sleep.
If you are responsible for answering floor calls, you may find it helpful to briefly round
on the floors and talk to the nurses to address any patient issues that may be arising
before you go to the call room. By answering pages in a timely fashion, being
courteous, and promptly addressing patient problems, the nursing staff may be willing
to “batch” non-emergent calls.
While sleeping in the hospital or at home, consider clipping the pager to the neck of
your clothing to decrease the chances of missing a page. If you inform the charge nurse
and/or page operator of your location, he/she can also contact you in the event of a
pager malfunction or a missed page.
As a more senior resident you will take call from home. On these nights, go to bed a
little earlier than normal, if possible. A few hours of uninterrupted sleep can make a
huge difference in your mood and abilities.
If you are on a night float schedule, create a comfortable sleeping environment to get
adequate sleep during the day. You might wear earplugs, keep the TV and radio off,
and use dark or opaque shades/window treatments for your room to block out natural
light.
Eat
Eating is often the last thing a surgical resident has time to think about during the day,
but quality nourishment is essential to optimal function. A little preparation may be
Sleep is the best meditation. --
Dalai Lam
a
55
needed to ensure you feed your tired body as regularly as possible. Use the time
between cases to get something to eat in the cafeteria. If you leave your pager number
with the circulating nurse, he/she can call you when the next patient arrives in the
operating room. (Always know the number to the OR for the next case in the event the
nurse is too busy to call you.) If the turnover time in your hospital is too fast to run to
the cafeteria, try packing some non-perishables (such as fruit snacks, crackers, granola
bars, power bars, and small bottled waters) in your pockets before leaving for work in
the morning.
Avoid drinking a lot of fluid before a case, since you don’t want to scrub out of a case
because you must use the restroom. Morning coffee is frequently a necessity, though.
Dehydration can become a real problem for surgical residents, so make sure to drink
water in between cases and catch up on fluids at the end of the day.
Because much of your eating will be “on the run”, take time to eat well-balanced foods
when you have more time. Eat plenty of fruits and vegetables, whole grains and
calcium-rich foods, and drink a lot of water. Stock your home refrigerator with healthy
food and if you don’t already know how to cook, learn now. During your time off, “stock
up” and freeze what you’ve made in smaller portions that can be easily warmed in the
microwave. It can be difficult to find healthy meals at the hospital after hours, so it is
worth it to take a few minutes to pack something healthy for dinner or a snack during
evening/night float rotations. Many residents gain weight during night float months,
even while making an effort to eat well. Resist the temptation to raid the vending
machine or cafeteria grill late at night. The old motto still rings true: “eat when you can,
sleep when you can, and use the restroom when you can.”
Exercise
Exercise improves mood, concentration, and physical health. Take the stairs whenever
you have the chance. Do a few sit-ups, or find some other minimal-space exercises you
can do in your call room. Any form of exercise will do, but you are more likely to do it if
it’s something you enjoy. Ride your bike to work. Join a running club. Take a yoga
class. Start a Cross-Fit program with fellow residents. Go rock-climbing with your
spouse. Find
something
, and find the time to “just do it” regularly.
Fun
Make a list of 10 things you like to do for fun. If you are working too hard, you will
probably have trouble coming up with that many. A sense of humor is essential to
surviving residency! Promise yourself the time to do at least one of those 10 things
every single day. Then go for two. Short breaks can be real energizers. Don’t feel guilty
that you are “wasting” time! Everyone needs a balanced life and it will make you a
better person and a better physician.

56
LOCKER LIST
Most hospitals provide lockers for house staff. Below is a list of items that you may find
helpful to keep in your locker:
• Toiletries, including toothbrush and toothpaste, deodorant, bar of soap, face
wash, skin care products, lip balm, and personal hygiene items.
• Medication, including prescription and OTC items (e.g. Advil)
• Non-perishable snacks such as crackers, pretzels, fruit snacks, granola bars and
power bars. (Remember: most sport nutrition bars have a high sugar content.)
• Change of clothes for clinic
• Extra pair of shoes, socks/stockings, underclothes
• Comb/brush
• Portable audio/entertainment equipment; be careful with valuables in the
hospital. Even the “safest” places can be vandalized.
• Spare charger for your phone and/or other electronic device(s)
LIFE BALANCE
The key to a happy and successful surgical residency is good time management. There
are several publications on how to manage a strenuous lifestyle,
1
be successful in your
career, and accomplish a great deal. While each author recommends a different
strategy, the overwhelming consensus is that
balance
is the key to success. The
happiest residents are typically those who enjoy their time both in and out of the
hospital. Make sure everything you need and want to do is
scheduled
because it is easy
to let things slip.
Make a list of priorities for your life. Be realistic! It is simply not possible to bake all
your own bread
and
serve as PTA President
and
train for a marathon
and
care for an
aging parent . . . during surgical residency, anyway. Decide which ones are the most
important to you, and schedule these into your down time. Although it is nearly
impossible to do each one every day, you can usually find time to squeeze some of
them into most days. It is important to keep up with your surgical reading on a regular
basis, so be sure to schedule that in as well.
"The biggest myth that I'd like to set to rest is that you can't have a family and
a successful career. The same skills that make a good leader -- organization,
drive, trust, delegation and compassion -- also go a long way to balance the
responsibilities of work and family life."
--
Ilene Gordon, CEO of Corn Products
57
Some other important activities to consider:
• Spending time with a spouse and/or child
• Spending time with friends
• Calling friends and family
• Going out for dinner/drinks
• Exercising
• Watching movies/TV
• Attending sporting events
• Religious services
• Volunteering
• Household chores
If you can afford it, pay someone to take care of the mundane tasks at home, such as
lawn care, cleaning, and laundry, especially if you don’t enjoy them. Many cleaning
services will let themselves in and out of your home once you establish a routine.
Laundry services are lifesavers. Consider grocery delivery systems, online and automatic
bill paying, and other conveniences that will reduce the time you must devote to
activities that provide extra, unneeded stress.
If you have a day off coming up, remember to schedule something fun and let your
loved-ones know you’re available. Friends and family may not want to bother you or
may just assume you’re too busy to call or include in activities. There is nothing more
depressing than finally getting a day off and having nothing to do.
OCCUPATIONAL HAZARDS
Part of taking care of yourself as a surgical resident includes protecting yourself from
blood-borne pathogens. ALWAYS practice universal precautions. Each hospital has its
own protocol to follow when you experience a needle stick or other exposure to a
potential pathogen, so become familiar with the procedure. Do not take a needle stick
or other exposure lightly; it is imperative for your own safety that protocol be strictly
followed.
MAINTAINING RELATIONSHIPS OUTSIDE THE HOSPITAL
If you are relocating to a new city and have minimal contacts, research areas of interest
to you before you move. Check out a newcomer’s guide, which is often published by
local chambers of commerce or available online. These sites often provide discount
coupons for such things as gym memberships and local restaurants. Consider joining a
club focused on one of your interests. Make friends with nurses at the hospital. While
much is written about conflicts between residents and nursing staff, we often have
many things in common, and nurses can be our greatest allies both in and out of the
hospital.
58
Expect to make close, long-lasting friendships with your fellow residents. These
relationships are important. Surgical residents frequently see each other more often
than they see their spouses, partners, families, and other friends. Surgical residency is a
time in which residents, fellows and attendings bond over the care of a sick patient, an
interesting operative case, a humorous event in the hospital or great dynamics on a
surgical team.
It is very important, however, to develop and maintain relationships outside of the
hospital as well. They can provide balance and a dose of reality to a world that is
frequently hectic, overwhelming and stressful. You might find the following tips helpful
to maintain these relationships.
• Call: Call your spouse or partner at least once a day. This requires just a few
minutes, and will be worthwhile to both of you. Don’t underestimate when you
will be home, as being just a few minutes late will likely frustrate your significant
other. However, if you over-estimate and arrive home early, they will be
pleasantly surprised.
• Notes: send an e-mail, text, or leave a note at home just to let your spouse or
partner know that you care. Again, this doesn’t take a great deal of time or
effort, but will be appreciated by the recipient.
• Gifts: put birthdays and special occasions in your calendar and set up reminders
for a week before. You can buy gifts online and arrange for quick delivery easily
from the hospital, and the effort will be appreciated by the recipient.
• Make time: If you have a weekend night or weeknight off, schedule a date.
Consider doing an activity that your partner prefers, in order to reinforce that
his/her agenda is also important.
• Listen: The lives of your partner and friends are important, too. Try to listen to
their stories; don’t monopolize the conversation, no matter how interesting you
think your day was. Also, it will be healthy for you to have a mental break from
the grind of the hospital.
• Utilize down time in the hospital: If a spouse, partner, or friend lives close
to the hospital, ask him/her to join you for a quick dinner in the hospital before a
case or while your call is “quiet.” (This requires that the spouse, partner, or
friend understand you may have to leave at any time for patient care.)
• Share tasks: avoid arguing over the chores at home. Hire help or make a list of
responsibilities and divide them in a way that is fair to both of you. It is often
difficult for partners to understand how little a surgical resident may be able to
contribute to household chores, particularly in the beginning of residency.
• Remain faithful to your partner.
REFERENCES
1. Brandt M. “The Claude Organ Memorial Lecture: the practice of surgery: surgery as
practice.”
AJS
2009; 198: 742–747

59
Chapter 7: DIRECTING YOUR FUTURE
Now that you are a surgical resident, you need to start thinking about the many
possible options for your career after residency. Although it may seem as if you have
just started, certain decisions will need to be made during your intern and second
years. The Association of Women Surgeons’ Website contains a “Career
Development Resource” (CDR)
1
that provides helpful advice for career planning with
links to subspecialties and organizations.
RESEARCH EXPERIENCE
Research time is typically scheduled after either the second or third year of residency
and will stretch your training to a total of six or seven years, depending on the number
of years taken in the lab. Alternatively, the laboratory experience can follow a five-year
residency, allowing you to carry over your research directly into your academic career.
Even if academics is just a consideration and not a final decision, you should consider
spending time in a lab. Doing research teaches you how to more critically evaluate the
literature, formulate a plan for investigation, learn proper data collection and analysis,
and compose an original research publication. In addition, most research residents
submit abstracts to meetings, learn to give a presentation to the scientific community,
and meet some of the leaders in surgery at conferences and meetings. Lab time hours
are a little better, if not more flexible, and the stress is a little lower, giving you a
chance to regroup and rekindle enthusiasm for surgery.
Academic Surgery
If you are considering a career in academic surgery, you will need to participate in
research and produce publications in order to be successful. Consequently, spending
one to two years in a research laboratory is strongly encouraged.
Laboratories and Mentors
Selecting a good laboratory and a good mentor for your research are the biggest keys
to success, especially if you have never done research before. If you are considering a
fellowship in a highly competitive subspecialty such as surgical oncology or pediatric
surgery, research experience is expected. In addition to helping with fellowship
selection, a strong research foundation will also be a catalyst to an academic career. It
is important that you select an area of interest to you; if you do not have one, find an
advisor or mentor that may help you with this important decision. An association with
one of the top people in your subject area is particularly important if you want to
pursue an academic surgery career. Similar to other professional circles, you will want
“Success can be attained if you care more than others think is wise, risk
more than others think is safe, dream more than others think is practical,
and expect more than others think is possible.” -- Anonymous
60
this person to make introductions for you, write letters of recommendation, and – most
importantly – steer you in the right direction. Go onto Websites such as PubMed to
determine the level of productivity of the lab and gauge whether it is working on
something that you are truly interested in. Who you know is crucial if you hope to gain
name recognition yourself. If you do not have a mentor, ask faculty members, the Chair
and/or the Program Director to suggest someone with whom they think you would work
well. Talk to fellow residents about their research experiences and ask them to suggest
a lab. It is important to talk to the PI (Principal Investigator) because s/he may have
new projects that are not apparent on the lab’s Website. Throughout your residency,
appreciate and cultivate relationships with the surgeons who take an interest in your
education and training.
Funding
The next, and equally important consideration, is funding your research experience.
Some residencies provide full salary and benefits for their residents in research years,
but some do not. Many provide funding if you stay at your home institution; still others
want you to do research time, but leave finding a salaried position up to you. Your
department and/or research mentor should be able to help with these questions, as
they tend to vary widely by institution. You may be asked to write a grant application
for the intended research. There are many funding sources available. The American
College of Surgeons
2
gives out a number of these grants annually. ACS also publishes
an annual list of available research grants relevant to surgery. Not only is writing a
grant proposal a tremendous learning experience, but obtaining a grant is quite
prestigious. Because deadlines for applying for these grants is often more than a year
before the start date, the sooner you know what you want to do, the better. You may
be able to supplement your income by “moonlighting”, but check first with your
program to see if this is permitted.
Courses
If you have never done research before, consider taking a course on how to conduct
research. The Association of American Medical Colleges (AAMC)
3
and the Association for
Academic Surgery (AAS)
4
sponsor courses on lab research each year that can be
extremely helpful in getting you started. Your program or research lab will often pay the
expenses for such a meeting, so be sure to ask. Also, the Association for Surgical
Education (ASE)
5
sponsors a “teaching skills for faculty and residents” course. Ask your
Chair to send you.
Timeline
Another important issue is to determine how long you should spend in the lab. Even
though a year sounds like a long time, most who have been there can attest that it’s
pretty difficult to complete meaningful research in only one year, especially in the field
of the basic sciences involving bench work. It really takes two or more years to get
projects up, running, and completed. Be realistic in terms of what you expect to
accomplish during your time in the lab; a straightforward conversation with your PI at
61
the very beginning regarding this issue is strongly encouraged. If you are considering
doing a PhD, you should consider three years of research. Residencies may be willing to
reorganize positions of residents to allow one person to do a third year, but this will
require careful planning and should be determined as soon as possible.
Advanced degrees
• PhD: For residents planning to spend at least three years in the lab, a PhD in
their field of interest can be very helpful. In addition to the practical research
training that you will receive in the lab, you will take classes on a variety of
subjects related to your field, data analysis, experimental design and conducting
research, all of which may improve your chances of successful scientific inquiry.
However, the decision to pursue a PhD will have to be made after discussions
with your department, particularly as residency duration and other requirements
are becoming less flexible.
• MPH: Academic surgeons with interests as diverse as cancer screening, injury
prevention, and trauma systems have pursued an advanced degree in public
health. It is an additional one or two years of coursework. Many residency
programs may be willing to accommodate interested applicants. Some programs
that have worked with residents and fellows to achieve this goal include Rush
University, University of Texas-Southwestern, University of Washington,
University of Virginia, and University of North Carolina. The coursework is often
taken as a separate, additional year of training. It typically provides a
background in Biostatistics, Epidemiology, Public Health, and Health Policy. A
thesis and/or practicum is often required. At the very least, an MPH helps you to
strengthen skills at interpretation of the current literature and understand
evidence-based practice. The degree can also help you learn to design strong,
elegant studies that have a higher likelihood of success and publication.
• MBA: An MBA has obvious applications for those interested in an administrative
role, but it also provides information and skills useful in many types of
organization management, including academic leadership and education. Study
areas include organizational management/behavior, which is broadly applicable
to many systems; operations management, used to optimize systems of
healthcare delivery in a variety of ways; accounting and finance, which are vitally
important for leading an office, division, department or other organizational
units; strategy, which is needed to develop an organizational vision, formulate a
plan and execution; marketing and negotiation, helpful in garnering support for
projects and/or programs within and beyond the organization; and leadership
development. Some MBAs, like executive weekend and modular (concentrated
face time) programs, can be tailored to your needs and time limita
tions, and may
even have a healthcare focus (e.g. a Masters in Management of Health Care, or
MMHC). MBAs can also be used as a pathway from clinical practice to an
alternate career choice like corporate leadership and/or entrepreneurship.
62
Helpful Tips
Because the length of time you spend in the lab is so brief, you will really have to be
focused and organized to make it worthwhile. Here are a few suggestions for
maximizing your experience:
• Choose a productive area where your research results will be important
regardless of the outcome. Formulate your research question clearly and remain
open to modifications. If possible, choose a project with multiple “arms” so that if
one experiment doesn’t work out, you can continue with others. Putting all your
eggs in one basket can lead to two years of research with no publication if you are
not careful.
• Emphasize quality rather than quantity. Academicians are more impressed by
one good study over five case reports.
• Frequently seek advice and criticism. It’s painful and frustrating to find out that
you made a wrong turn two months after you made it.
• Keep a careful record of your data. You never know if someone ten years from
now will question the outcome, and you will be called upon to defend your findings.
• Write it up and get it published! Research isn’t of use to others if you don’t
spread the word. Keep in mind the issue of authorship when selecting a lab. If
the resident doing the research isn’t going to be listed on the publication, steer
clear! While this is unethical and unlikely in surgical labs, many PhD students have
run into this problem. Ask specifically about authorship issues before you sign up for
the research.
NON-TRADITIONAL EXPERIENCES
The fabric of medicine and surgery is changing. The last few decades of surgery have
seen tremendous growth, primarily due to new technologies. Minimally invasive
approaches have revolutionized and brought new life into the fields of bariatric, thoracic
and vascular surgery. With the continued search for newer and better instruments and
devices, surgeons work closer than ever before with industry. Many have been
successful in turning their ideas into commercial products and patents.
In addition, healthcare policy remains a volatile and controversial issue in a society that
continues to age and live longer. Physicians and surgeons have not traditionally pursued
a strong voice in healthcare politics, but with the changing needs in 21st century
medicine, surgeons are more frequently finding themselves in “non-traditional” roles as
consultants, CEOs, medical directors, entrepreneurs, and policy makers. It is not
surprising that non-traditional degrees, such as the MBA, are now pursued by surgeons.
Individuals who are planning to practice in a rural setting or as a missionary surgeon
should seek opportunities to train in these settings during residency. Check with your
program director for information about elective rotations that provide this sort of
exposure.
63
FELLOWSHIPS
The term “fellowship” is used somewhat loosely to describe a period of training
beyond primary residency. Some “fellowships” lead to additional board certification,
are subject to accreditation and oversight by ACGME
6
and are more correctly termed
residencies. Examples are Pediatric and Colorectal Surgery. Examples of true
fellowships, where an individual may have a junior faculty position, are Transplant
Surgery and Minimally Invasive Surgery. The key to matching for your ideal position
is having research experience and a mentor willing to open doors and make phone
calls on your behalf. The sooner you make a decision on a fellowship, the more time
you will have to identify a mentor, research the various programs, and begin the
process of making yourself competitive.
Subspecialties
For some, the inclination to sub-specialize may have been what brought you to surgery
in the first place. Others find that they become interested in learning more about a
specific area after doing a rotation on a subspecialty service. The decision of whether or
not to pursue fellowship training is closely tied to your vision of how you wish to
practice surgery when you complete your training.
While all fellowships are designed to train you as a subspecialist who will provide
complex surgical management within a specific sphere of clinical problems, some are
also geared to producing the next generation of surgical faculty and academic leaders.
The majority of fellowships want you to be Board-eligible for your primary surgical
discipline before you start the additional training. Therefore, you won’t begin them until
after your five clinical years of general surgery are finished. One exception is Trauma/
Critical Care, where you can do a fellowship after three years of general surgery
training. In addition, Plastic and Vascular surgery have some “integrated” positions in
which you complete two to three years of general surgery followed by three or four
years of subspecialty. Most of these spots are actually secured through the residency
match when you’re a medical student, but there are sometimes unexpected openings
due to attrition.
Completing the minimum requirements for surgical training should be a primary goal,
and you should not leave a program before becoming Board-eligible, except to transfer
to an integrated program. While most people go into a fellowship directly after
completing their primary surgical specialties, there are a few who wait to go back for
extra training until after being in practice. In general, your chances of matching a
competitive fellowship are more difficult the farther you are out of training, particularly
in the more competitive academic programs.
Personal Life Considerations
An important consideration should also be your personal life. Are you willing to give up
more time for training? Are you willing to have someone else own your time for more
64
years? Being a fellow means putting some of your independence on hold while you gain
additional expertise in an area. Talk openly with your spouse or partner about plans for
additional training, as he or she may be putting career or child-rearing plans on hold
until you finish. The financial considerations of continuing as a trainee should also be
factored into the decision. Student loans can generally be deferred but other debt may
be piling up. Despite all of these sacrifices, if you really want it, go for it!
Resources
Before applying, it is important to learn as much as you can about a given subspecialty.
One place to start is the American College of Surgeons Website
2
, which has links to a
variety of surgical society Websites that give information about subspecialty training.
Ask to do a rotation in a specific area if you previously have not had the opportunity to
do it. Talk with current practitioners of the discipline to determine if you see yourself as
one of them.
Explore both the private and academic options for the subspecialty. Try to get a sense
of the availability of positions after completion of a fellowship. Some disciplines, such as
Pediatric surgery, have published workforce estimates. Transplant surgeons have
limited the training spots available in their field because of limited organs and
institutions where solid organ transplant can be performed.
The Pursuit
As soon as you know you want to pursue a certain fellowship, start working on the task.
The application and interview process for some fellowships begins as early as the PGY-3
year. Additional details are available from the National Residency Matching page
7
. You
can always withdraw an application or change your mind, but if you start the process
too late, you may have to spend an extra year doing something else while waiting to
start your fellowship. Pediatric, Plastic Surgery and Surgical Oncology fellowships are
currently the most competitive, so do not postpone doing your investigative legwork
and getting the required paperwork going on these programs! Most programs use a
match process to offer positions to candidates, similar to what you used to enter
general surgery. Because of the time delay between acceptance into a program and
starting it, openings in good programs can occur because of the loss of an accepted
candidate. Thus, if you make the decision late to pursue fellowship training, check
around. What you are looking for might become available when you least expect it.
Find a mentor early in the process to guide you through the unspoken rules. The choice
of a mentor or mentors is critical to the successful pursuit of a fellowship. Similar to
when you applied for surgery the first time, your application may look the same as ten
others who want the same position. Networking can mean the difference between
getting a fellowship or not. The world of surgery grows constantly smaller with every
step, and the people who help you today may be your peers tomorrow. Do not be
afraid to ask for advice and guidance from people within your department or those you
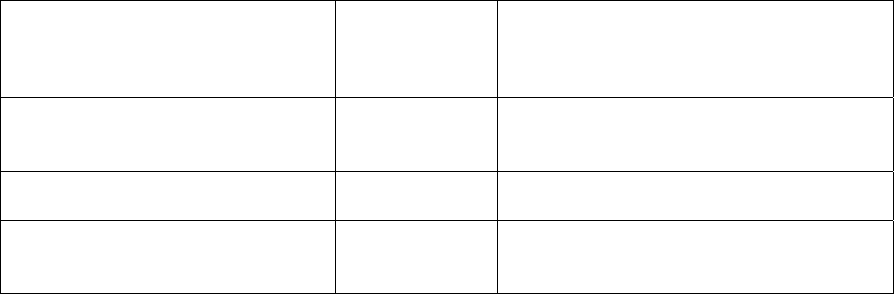
65
meet at surgical meetings. A mentor does not have to be in the same city. E-mail
relationships abound!
The most competitive fellowships generally want you to show a record of interest in the
discipline. Most often, this is accomplished by taking extra time during residency to
conduct research and produce publications in the field. Taking this time will also help
you to decide what type of fellowship within a discipline may be of interest to you. If
you want to have a basic science lab as part of your academic practice, you may want
to pursue a fellowship that will combine a basic science program with a clinical
program. A requirement for additional lab time may discourage you from pursuing a
fellowship, but you should take the time you need to get the training that will allow you
to become the surgeon you want to be. It is not uncommon for the time span to last up
to 10 years for completion of primary and subspecialty surgical training. Those of us
who have done it will generally tell you it was worth it.
Societies and Certifications
In order to find the specific training programs and their requirements, you need to
know if a fellowship is overseen by a surgical society or the ACGME
6
. Fellowships under
the jurisdiction of the ACGME will lead to special certification after you pass an
examination similar to the Board certification process for primary surgical disciplines.
Most society-accredited programs do not have a special Board certification process.
Always make sure that the program you wish to apply for is properly accredited. There
are programs (e.g. non-accredited Pediatric Surgery fellowships) that do NOT entitle
you to sit for specialty Boards upon completion. Make sure the time invested in your
fellowship will get you the credentials you desire. Fellowships accredited by the ACGME
are listed in the Graduate Medical Education Directory (a.k.a. the “green book”) for
each subspecialty
6
. Society Websites are good resources for locating the society-run
programs. You can also call the main office of the society to get a list of approved
programs. There are some fellowships that are currently in development in a variety of
disciplines. These may be more loosely organized without a definitive organizing body.
Be cautious about pursuing this type of fellowship. See the table below for types of
fellowships available after the completion of general surgery.
Subspecialty Fellowship Certifying
Body
Affiliated Society
Plastic and Reconstructive Surgery ACGME American Society of Plastic and
Reconstructive Surgeons
http://www.plasticsurgery.org/
Colon and Rectal Surgery ACGME American Society of Colon and Rectal
Surgeons http://www.fascrs.org/
Vascular Surgery ACGME Society for Vascular Surgery
www.facebook.com/pages/Society-for-
Vascular-Surgery-SVS/
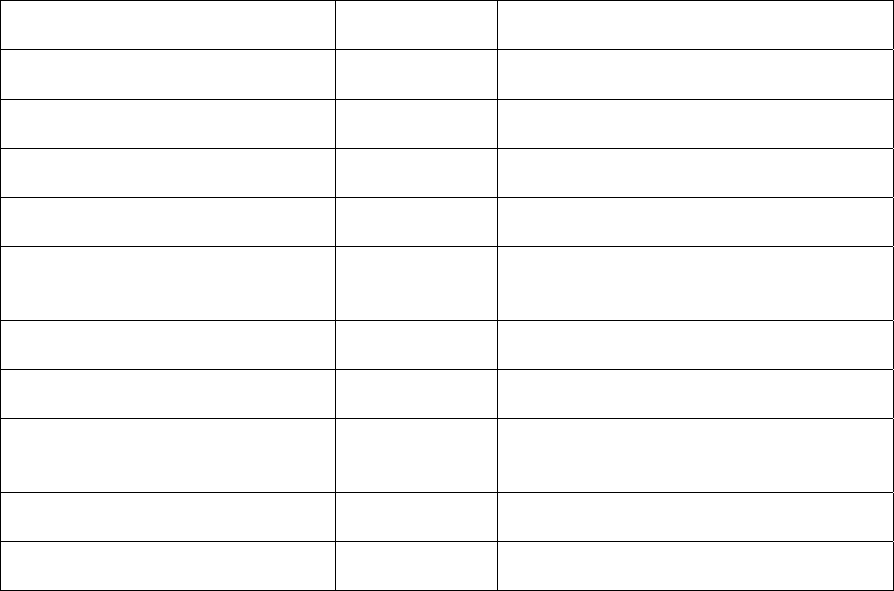
66
Cardiothoracic Surgery
Non–Cardiac Thoracic Surgery
ACGME Society of Thoracic Surgeons
http://sts.org/
Critical Care ACGME Society of Critical Care Medicine-Surgical
Section http://www.sccm.org
Pediatric Surgery ACGME American Pediatric Surgical Association
http://www.eapsa.org
Surgical Critical Care ACGME American Association for the Surgery of
Trauma (AAST) http://www.aast.org
Surgical Oncology ACGME Society of Surgical Oncology
http://surgonc.org/
Minimally Invasive and
Gastrointestinal Surgery
Fellowship
Council
Society of American Gastrointestinal and
Endoscopic Surgeons
http://www.sages.org/
Breast Surgery Society American Society of Breast Surgeons
https://www.breastsurgeons.org/
Organ Transplantation Society American Society of Transplant Surgeons
http://www.asts.org/
Endocrine Surgery Independent American Association of Endocrine
Surgeons
http://www.endocrinesurgery.org/
Hepatobiliary Surgery Independent Americas Hepato-Pancreato-Biliary
Association http://www.ahpba.org/
Head and Neck Surgery Independent American Head and Neck Society
http://www.ahns.info/
BOARD CERTIFICATION
Upon successful completion of five years in an accredited surgery residency you will be
“Board” eligible (i.e. eligible to take the examinations necessary for Board certification).
Board certification in general surgery requires that you demonstrate proficiency in the
Fundamentals of Laparoscopic Surgery prior to taking the American Board of Surgery
Examination, and pass a written (qualifying) and an oral (certifying) examination. You
must be re-certified by written examination every 10 years. The qualifying exam is
offered in August and the certifying exam is offered after successful completion of the
qualifying exam. The qualifying examination is a computer-based exam that consists of
multiple-choice questions designed to evaluate a candidate’s knowledge of general
surgical principles and the basic sciences applicable to surgery. It lasts eight hours and
is held at computer-testing facilities across the U.S. The certifying exam is an oral
examination offered five times a year, with three consecutive 30-minute sessions, each
conducted by a team of two examiners. The emphasis, unlike the qualifying exam, is
more about judgment and clinical decision-making, and evaluates the examinee’s ability
to manage a broad range of clinical scenarios in an organized and “safe” way. There are
several good reasons to pass these on your first attempt: 1) It is no fun to retake them;
2) you have to pay each time; and 3) there is a limit to the number of failed attempts.
Once an application is approved, the applicant is granted a maximum of five
opportunities within a five-year period to pass the Qualifying Examination and a
maximum of five opportunities within a five-year period to pass the Certifying
Examination
8
.

67
Oral Boards
As you prepare to take oral Boards (or interview for a position), remember that your
examiners will score you on the basis of sensory input. What you say is only part of
what they will perceive.
• Sight: Dress professionally. Consider a blue or gray suit, and avoid heavy makeup
or flashy jewelry. Before your exam, practice sitting in front of a mirror to pick a
professional, calm position; don’t move out of it during your exam. Many examiners
comment on nervous appearances (tapping fingers or toes, wringing hands, chewing
your mouth or lip, crossing and bouncing your leg, or playing with a tissue).
Practicing with a peer may be informative and helpful, and may alleviate some of
the anxiety of the real experience. Videotaping yourself may give you invaluable
insight into your idiosyncratic gestures and speech.
• Smell: Do not wear heavy perfumes or cologne.
• Touch: Be gracious and offer a firm, dry handshake when offered.
• Sound: Do not chew gum. Before the exam, imagine yourself speaking in a calm
and professional tone of voice and then try your best to do so. Avoid any and all
sarcastic, facetious, or disrespectful remarks.
• Organization really matters. Make sure that you always start with a focused
history, only asking relevant questions. It is helpful to ask pertinent questions as a
group so that the examiners know you are organized and not just picking things out
of the air as you go. Indicate that you would do a complete physical exam but focus
on the issue being addressed in the question. Always ask for lab and x-ray data in a
specific sequence as this will help you remember everything and make it less likely
that you will leave anything out. Don’t forget to ask them for any specific
information you need or if there is anything else significant in the history, physical
exam, lab, or x-ray. However the examiner is trained to give you all the information
that you need so do not waste time asking for a long list of irrelevant tests.
The examiner’s job is to give you NO feedback, so don’t look for any clues on how you
are doing.
The day of your exam, you will join a number of nervous people and have a briefing by
someone from the Board, who in general will try to answer questions and provide some
reassurance. They will also give you a 3-session exam schedule (your exam may begin
immediately or several hours later), and will remind you to fill out the change of
address card (if applicable). Avoid engaging in a lot of pre- or post-exam talk with other
examinees, particularly if you are prone to becoming more anxious. There are no
mandatory failures, despite urban myths you may have heard. This means that it is well
within the realm of possibilities that all applicants within the entire country could
become certified.
The questions are generally not the esoteric “zebras” but more often the routine
situations where there is usually good consensus on management. The examiners
68
just need to know that you can think well enough to be safe as a surgeon. Imagine
that you are in the situation they give you, caring for that patient, so you can think
more clearly. You know that you have all the information you need to pass your oral
examination, because you’ve already passed your written exam. Just show them you
can work under pressure and care for patients (just as you do every day).
If you don’t know the answer to a question, ask for a consult, call “a friend specialist on
the phone” for emergency assistance, or say you don’t know. Do not overuse this
option. If you can not demonstrate the necessary breadth of knowledge, you will not be
judged a candidate for Board certification. They will go on to the other questions that
you may know more about. Don’t make things up! Give solid, conservative, safe
treatment options, the kind you might have used your first year in practice when you
were being cautious. Respond in the amount of detail you would use explaining your
plan of action to an intern.
Consider studying Norton’s
Surgical Decision Making,
9
or develop your own algorithm
treatment plans for cardiogenic shock, lung lesions, melanoma, hyperparathyroidism,
neck mass, thyroid lesion, ischemic leg, gastric and duodenal ulcers, major fractures,
bone tumors, ovarian tumors, head injury, pediatric abdominal pain and GI bleed, etc.
Safe Answers
10
and Cameron’s
Current Surgical Therapy
11
are also good references.
You may find it helpful to practice ahead of time with others, or sign up for a review
course. Although pricey, most courses focus on the “drill” of answering questions and
may be beneficial if you generally are not good at oral exams. Practicing out loud is
very important. Many training programs offer mandatory mock orals. Ask your
department to start them if they don’t already have them. You may also be able to
participate in mock orals at an outside institution with advance notice. Your
performance reflects on the quality of your program, so the Program Director should be
receptive to this suggestion. There are courses like Osler
12
for those who feel extremely
intimidated by this process, and they are strongly encouraged for those who have failed
the oral exam once.
PRACTICE OPTIONS
Your biggest decision during residency will be whether you plan to be in a private
fee-for-service practice, a salaried position, or academic practice. How health care
reform will affect these options remains in flux. Talk to as many people as you can
in these different areas, and find out all the pros and cons. Check out the AWS
Website for more information on each area in the Career Development Resource.
The site also includes a Powerpoint presentation on how to negotiate your first job.
Here is a brief outline of the basic options
1
:
Private Practice
Private practice (solo or group)
1
gives you a lot of freedom, but requires you to be a
business owner as well as market your skills and expertise. The practice
69
management aspects can become very time-consuming, and are annoying to some.
Others view it as a challenge and an opportunity to do things their own way. This
option gives the greatest geographic freedom, the greatest opportunity for financial
remuneration (in most cases), but also the greatest risk. The viability of your
practice is dependent upon the type and number of referrals, marketing, whether
you are a self-promoter, and also on the level of insurance reimbursement and
overall financial climate of the region. Some regions have low costs of living but
stifling malpractice rates and poor reimbursement. Making a profit may mean longer
hours, more ER calls and being “readily” available to referring physicians.
Academic Practice
Academic surgical practice can be an immensely rewarding career choice, and it
offers an opportunity to stretch beyond the clinical practice of medicine into
discovery and creativity. “Academics”, as it is called, can encompass a wide variety
of practice types, but there are a few common themes:
1. Advanced training
2. Clinical practice
3. Research
4. Education
5. Administration
Advanced Training
For general surgery, advanced training in the form of a fellowship is common, though
not mandatory. Among the general surgical specialties, advanced surgical training is
becoming the standard in academic practice. Certain specialties
require
additional Board
Certification and/or training:
Additional Certification:
required
• Cardiac & Thoracic Surgery
• Hand Surgery
• Pediatric Surgery
• Surgical Critical Care
• Vascular Surgery
Additional Training:
not all are required, but additional training is
encouraged
• Surgical Oncology
• Colorectal Surgery
• Hepatobiliary Surgery
• Transplantation
• Minimally Invasive Surgery
• Breast Surgery
• Endocrine Surgery
• Trauma Surgery
• Acute Care Surgery
• Rural Surgery
• Foregut Surgery
• Bariatric Surgery
• Geriatric Surgery
• Aesthetic Surgery
Clinical Practice
One of the challenges of academic practice is balancing clinical surgery with teaching,
administrative commitments, and research. Academic clinical practice typically does not
vary strikingly from community or private practice. However, certain differences may be
found. Some academic medical centers are referral centers for difficult or challenging
cases, so that the volume of typical “bread and butter” cases may be less. Academic
surgeons may perform fewer operations over the course of a year than physicians in
community practice, though volume is highly variable. Community surgeons, on the
other hand, may have more flexibility in the scope of their practices. Some general
surgeons in remote areas perform Caesarian Sections and simple orthopedic
procedures. Due to specialization at academic centers, this kind of practice would be
very unusual.
Research
Research is really the
sine qua non
of academic surgery. Some sort of ongoing research
and publication is typically required for success and advancement. Though it is the
expectation that all academic surgeons participate in research, whether it be basic
science, translational, or clinical, the commitment towards research varies widely. The
amount of time devoted to research depends on factors such as funding, practice
partnerships, and department and hospital priorities. An academic surgeon may spend
anywhere from zero to 100% of his/her time on research activities. Some funding
mechanisms, such as NIH-sponsored Mentored Research Awards (the “K” series)
actually require at least 75% of time to be spent in research. For surgeons with a heavy
interest in clinical research (patient-based), these proportions also might be different.
Research and research training can begin during residency or fellowships, and there
should be a plan to continue with research after completion of clinical training.
Advanced Degrees (PhD, MBA and MPH were discussed under
Research
above)
Some residents have obtained degrees in Public Policy, Masters of Clinical Science,
Masters of Public Health, or a PhD. It is important to discuss these options with
research mentors and department heads to determine the best path for you.
Education
Academic medical centers are the institutions that train the coming generations of
physicians and surgeons. Academic surgeons must be committed not only to quality
patient care and scientific inquiry, but also effective, innovative, evidence-based
surgical education. Surgical education is increasingly recognized as a foundation of
academic practice. There are many opportunities for improving effective teaching skills,
as well as for research in this growing field. An excellent Website resource is
www.surgicaleducation.com.
Participation or leadership in medical student and/or resident education can be
rewarding and enriching, and academic surgeons should pursue some sort of education-
related activity. Examples that require a smaller time commitment would be education
70
committee service or mentoring responsibilities. Somewhat larger time commitments
include heading educational conferences, student clerkship directorships, or even
serving as Program Director. Often, with more seniority comes more responsibility.
For those interested in teaching opportunities without the research responsibilities there
are opportunities at some academic centers in the “Clinical Instructor” track. These
positions may be very structured, full-time or part-time, and may allow greater flexibility
and career options for those with different career interests. It is generally the
expectation that documentation of effective teaching must occur for advancement. This
could be in the form of teaching awards, publications, etc.
Administration
There are many rungs on the academic ladder, and ascending to each subsequent level
usually involves some combination of publications, national or international prestige,
funding, and administrative service. Typically, administrative service includes two
general categories: institutional service and national/international service. More senior
academic physicians will be expected to have leadership roles in either or both of these
areas.
Home Institution
As a young faculty member, you may be pressed into service for any number of
committees. In general, you should try to select committees that hold your
interest so that you will be an active, valuable participant, realizing that you may
not have a choice in selecting committees. Some examples of hospital or
university committees include Institutional Review Board service, Benefits
Committee service, Quality Assurance Committees, and Faculty Organizations. Be
careful in accepting these responsibilities. While some are necessary, others will
add little to your personal gain or support your goals for promotion/tenure.
National/International Service
Ideally, you should participate on local, regional, and national levels (to varying
degrees) in your area of interest. For example, as a trauma surgeon in Chicago,
you might be a member of the Chicago Committee on Trauma, the Eastern
Association for the Surgery of Trauma, or the American Association for the
Surgery of Trauma. Membership to societies is only the first step. Appointment to
national committees should be sought. With more seniority and experience,
committee chairs, executive counsels, and officer positions are all available and
should be pursued. In addition, you should participate in parent organizations,
such as the American College of Surgeons, or (again using Chicago as an
example) the Chicago Surgical Association. The key is finding organizations that
interest you and committees that might make a difference. You may need to ask
your department head or Chair to nominate you to a particular committee, or
you may simply put in a word yourself. Working within these organizations can
be tremendously rewarding and a great way to meet colleagues, mentors, and
71
leaders within your field. Many societies will ask for volunteers for committees.
Do not hesitate to put your name in for a position.
Summary
Academic surgery can be taxing, requiring a delicate balance between all the
various commitments of your career, but it can also be tremendously rewarding,
and if you have any interest in the above-mentioned areas, it is an avenue at
least worth exploring. The more information you gather, the better perspective
you will obtain on what situation is right for you. There are jobs available almost
everywhere if you are willing to look. Create your own opportunity.
Salaried Employee Positions
In these types of practices, you are the direct employee of a hospital, HMO, or
government organization. In exchange for a salaried income that typically averages
somewhat below that of a surgeon in private practice, you have income security and
malpractice coverage, a predictable work schedule that includes paid vacation time,
and are relieved of the headaches of managing a practice, securing reimbursements,
etc. Salaried positions are becoming more common in the era of health care reform
efforts as physicians seek refuge from the twin perils of medical malpractice liability
and dwindling reimbursement. Different situations have different contractual
arrangements, so check the details carefully before signing on. Refer to the Career
Development Resource on the AWS Website for additional details about HMO, VA,
and military options and for a Powerpoint presentation on negotiating your first job.
1
Making Choices
So how do you decide? The first thing to do is to make a list of priorities for yourself,
both personal and professional. What kind of job syncs best with these? Try to imagine
exactly how you would like to see yourself five or ten years from now. Discuss your
thoughts with your family because the “perfect” job for you may leave your significant
others very unhappy. Many marriages experience stress in the transition after residency
because of unrealistic expectations, such as “my husband will just have to go wherever
I decide,” or “I thought after her residency my wife would be able to spend a lot more
time at home!”
Here are some questions to ask yourself:
• Personal: Where do I want to live? What kind of leisure activities do I need to stay
happy? Is there work for my spouse and schools for my children? How much free
time do I need for family and recreation? What kind of weather do I like?
• Professional: What kind of cases do I want? Do I want a lot of subspecialists
around? Do I want to make all my own decisions about finances, or will I be content
to draw a salary and let someone else run the show? How much am I willing to go
into debt? Do I want to do lots of endoscopy? Do I want to do my own critical care?
Does this community keep up to date? What are the promotion tracks? Can I get
72
time off the clock for maternity/paternity leave? Is the equipment I need there? If
not, will they get it for me? Can I possibly go solo, or do I need a guiding hand and
ready advice if I’m faced with a tough case?
For the specifics of finding a position, there are a number of options suggested below.
• Use a headhunter. Some will work for you to find just exactly the job you want.
Others will check a list of open positions to see if it is something you may be
interested in, and if you meet the criteria of the potential employer. (Usually the
employer will pay the recruiter’s fee.) Check the classified ads in prominent journals
for your field. Websites, particularly industry sites, also list potential positions. Ask
for references from previously placed physicians before signing any agreements.
In many cases, your travel expenses will be paid. A good recruiter will also save you
time by eliminating places that would be a “bad match” for your needs and wants.
• Find a negotiator. In addition to a recruiter or headhunter, you may want to
consider investing in a medical contract negotiator who can help decipher the fine
print, fight for the most favorable salary and benefits package, and ensure other
amenities that might otherwise be overlooked by a naive beginner.
• Pick a geographic area. If you know where you would like to live, write the
hospital administrator(s) of that community or the Department Chair to ask about
job opportunities. If he or she refers you to another surgeon in town, keep in mind
that person may not want more competition. They can answer your questions about
the hospital and OR conditions, but you may get some different answers on
community needs for surgeons by talking to someone in internal medicine or family
practice. You will also get an idea of the quality of the surgeons there. If you are a
good technical surgeon, have a good bedside manner, and can get along with
referring physicians, you can succeed almost anywhere if you are willing to work at
it for a few years. Beware of local politics. Sometimes talking to physicians in the
adjacent community will give you some wonderful insights into the medical
community in which you are interested.
• Talk to the surgeons in your training hospitals. Find some of your attending
surgeons who have been in practice for several years and ask their advice on
opportunities, local competition, academic vs. private practice, etc. Do not shy away
from asking financial questions, since you do not want to starve for the first five
years of practice. If you have a good working relationship with those surgeons, they
will usually be flattered you sought them out for advice. Many times they will let you
come into their offices to observe the mechanics of their practice, and talk to their
office managers about how to set things up.
• Attend a seminar. Several com
panies (e.g. Conomikes
13
) provide one- or two-day
seminars on setting up a practice, which may be helpful in alleviating anxieties
about the business aspects. Many seminars also give advice about negotiating your
best contract options. Beware of “no compete” clauses in contracts if you decide to
leave the first group you join but want to stay in the same area.
• Consider locum tenems. Locum tenems firms will place you temporarily in a
73
practice to replace a surgeon who is on vacation, ill, or retiring. They will take care
of credentialing issues, malpractice, housing, and will generally pay for a spouse to
accompany you. Such an arrangement can give you an opportunity to explore
different practice settings, climates, and geographic areas. It is also worth
considering for periods of time when you are between residency and fellowship, or
other professional “down” time where you need to maintain an income. Do contact
the placement firm early, though, because the credentialing process can be lengthy.
REFERENCES
1. Association of Women Surgeons Career Development Resource,
https://www.womensurgeons.org/home/Career_Planning.asp. Accessed 6.7.12
2. American College of Surgeons. http://www.facs.org/ Accessed 6.8.12
3. Association of American Medical Colleges. https://www.aamc.org/
Accessed 6.8.12
4. Association for Academic Surgeons. http://www.aasurg.org/ Accessed 6.8.12
5. Association for Surgical Education. http://www.surgicaleducation.com/
Accessed 6.8.12
6. Accreditation Council for Graduate Medical Education (ACGME)
http://www.acgme.org/acWebsite/home/home.asp. Accessed 6/6/12
7. National Residency Matching Program http://www.nrmp.org/fellow/index.html
Accessed 6.8.12
8. American Board of Surgery http://www.absurgery.org/. Accessed 6.6.12
9. Surgical Decision Making, 5
th
Edition. (Lawrence Norton et al., 2004, W.B.
Saunders, Inc.)
10. Safe Answers http://safeanswers.org/home.html. Accessed 6.8.12
11. Current Surgical Therapy, 10
th
Edition. (John Cameron, 2010, B.C. Decker.)
12. Osler Review Courses. www.osler.org Accessed 6.8.12
13. Conomikes http://conomikes.com/. Accessed 6.8.12
Additional Reading
Chen H. et al. Success in Academic Surgery. Springer 2012.
74
Chapter 8: FOR THE MEDICAL STUDENT
So, you want to be a surgeon!
Congratulations! You wouldn’t be reading this now if you weren’t considering a career in
surgery or a surgical subspecialty. Those of us writing this book believe there is no
more rewarding specialty choice you could make.
THIRD-YEAR SURGERY CLERKSHIP
Overview. A third-year (“Junior”) clerkship in Surgery typically consists of a number of
weeks of clinical experience, divided between general surgery, subspecialties (which
may or may not be elective), and, in many medical schools, an exposure to Anesthesia.
Your final grade will be a composite of evaluations from each clinical rotation, and
typically a standardized test (“shelf exam”) administered at the end of the rotation.
Some rotations in the clerkship may be highly structured, with welcome letters, reading
lists, and even exams at the end. On others, expectations may not be as explicit. On
each rotation it is imperative that you ascertain to whom you are primarily responsible,
who will be writing your final evaluation, and what the expectations are. Either the
Clerkship Director or the Clerkship Coordinator should give you this information at
Orientation. Generally, the information will also be accessible on a Website.
Hierarchy. You will be assigned to a clinical team typically headed by a senior or Chief
Resident (clinical post-graduate year 4 or 5) and consisting of a junior resident (PGY 2-
3) and an intern (PGY-1). The Chief Resident in turn reports to a number of attending
surgeons. At many institutions the hierarchy is very strict, and it is best to always go up
the chain of command to one's intern first, then juniors, then Chief, unless there are
emergency/extenuating circumstances. You should think of yourself as an integral part
of this team, and function accordingly. You will be assigned to inpatients on your team.
You will be expected to familiarize yourself with these patients, to round on them in the
morning and prior to afternoon rounds, and present them to the team. Ask the Chief
about the preferred presentation format and expectations for the service, as this varies
by rotation. Morning rounds are typically “work” rounds (as opposed to teaching
rounds), and in some cases the night duty resident may be the person presenting the
patient. Also ask about the policy for writing progress notes, as some institutions do not
allow students to enter information in the permanent patient record, whether this is an
electronic or paper record. If this is the policy, keep your own progress notes and ask a
resident to critique them for you. You should read the progress notes on your patient
daily and follow their lab and test results. Generally, you can expect to follow the
patients admitted to your team when the team is on call, and all cases that you scrub.
Conferences and clinic responsibilities are variable, but again, expect to stick with your
team. Always advise the Chief or senior resident of any mandatory clerkship lectures
that you are required to attend that will pull you away from your ward duties.
75
Functioning on the Wards. There is a certain amount of “work” inherent in running a
surgical service. Find ways to be efficient and useful to your team, such as:
• Do labs as soon as rounds are over if you are not in a case, and then go to
breakfast. Most hospitals will have a phlebotomist or technician to draw the
scheduled labs. It is worth shadowing them to learn this skill as it may be
your responsibility to draw the labs out of normal hours.
• Always be prepared to change dressings with supplies stocked in your jacket
pocket.
• On morning rounds, be the student who puts on gloves in every patient’s
room and assists with dressing changes.
• In the afternoon, after cases, be sure to check vitals, results of tests that
were done during the day for all patients, see your patients before afternoon
rounds, and volunteer for anything that a senior resident might need
assistance with.
Operating Room - Exposure to surgical cases in the Operating Room is a priority on
surgical rotations, as this is the defining event that distinguishes our specialty. You
must prepare for elective cases by reading about the operation, the pathophysiology of
the disease process, the pertinent surgical anatomy, and familiarizing yourself with the
patient. Expect to field questions on any of these topics in the OR. If you are permitted
to write Brief Op Notes on these patients in the medical record, the minimum typical
format is to note the date, the operation performed, surgeon, presence or absence of
drains, the IV fluids administered and estimated blood loss (the anesthetist will tell you
these), and whether or not a specimen was sent to pathology.
Do recognize that surgery is a specialty that involves much more than the technical
aspects of performing an operation. All of us are excited about what we do, and feel
privileged to work as surgeons. It is not the purpose of the third-year clerkship rotation
to teach you
to operate
. Rather, its goal is to introduce you to the discipline of surgery,
the work-up of surgical conditions, pre- and post-operative care, the surgical approach
to problem-solving, and to the essential aspects of medicine that our expertise
encompasses (i.e. breast, acute abdomen, trauma, fluids and electrolytes, wound care,
and surgical nutrition). What every surgery student should take away from the clerkship
-- and what your final exam will test -- are the following: work-up, pre- and post-
operative care, indications, contraindications, and complications of common surgical
conditions.
That said, we fully recognize that what “jazzes” a surgeon most happens in the
Operating Room. On your junior clerkship you may be permitted to assist with closing
skin incisions, sewing in drains, etc. Students should clarify early on in their clerkships --
and ask the resident before going into the OR -- what is expected of an MS3. As a
student you should be practicing two-handed knot tying and simple suturing, so that
when given an opportunity to participate, you are prepared. All residency training
programs have a surgical skills lab, and you should ask if a basic surgical skills course is
available for the medical students.
76
• The more confidence and skill you demonstrate, the more you may be
allowed to do.
• It is useful for students even at the beginning of their clerkships to start to
learn the names of common surgical instruments.
Oral Presentations - Perhaps no skill is as worth developing and honing as the skill of
oral presentation, as it is the “first impression” you will be making in countless
encounters with other clinicians for the duration of your career. The oral presentation
follows a highly stylized format, with which you must familiarize yourself, and from
which you must not stray. You will be presenting inpatients daily on your team work
rounds, and the efficiency of the team depends upon the clarity and economy of your
presentation. You will be presenting patients as you see them in the outpatient setting
to your preceptor. You will be presenting in Attending Rounds. Each team/preceptor
may prefer a different style of oral presentation. See if you can pick up on the team's
style early on in the rotation and adapt your presentation accordingly. While it is a good
idea to prepare for the next day's work, try to set a time limit for how much time you
spend preparing oral presentations that you will be giving on the next morning on
rounds. As an intern, you will be required to make oral presentations "on the fly", and
third year can be a good opportunity to develop this skill. Be sure to read Chapter 1 in
this book, “Rounds”, for more tips on oral presentations.
Reading. The assigned text may be available through your school library in electronic
format. Read some of it every day. Read the textbook
before
reviewing the “practice
question” type books. Read prior to scheduled lectures. Read about your patients. Do
not relegate reading solely to your evenings at home; there is some “down time” every
day, which may be spent reading and quizzing your fellow students. Again, one of the
best ways to study for the mini-board is with a question bank, but reserve practice
questions for the last few weeks of the rotation after reading texts. Some of our
favorite review resources are:
•
Carlos Pestana Review Notes for Surgery
1
-- found online, this is a high-yield
resource for acing the Surgery clerkship shelf exam.
• Case Files Surgery (Lange Case Files, 4
th
Edition)
2
: 56 real-life cases that
illustrate essential surgical concepts; each case includes a complete discussion,
clinical pearls, references, definitions of key terms, and review questions.
• Kaplan Medical USMLE Step 2CK Q-book
3
: question book geared toward Step
2CK, with separate sections for each of the disciplines (i.e. Surgery, but also
OB/GYN, etc.).
• NMS Surgery Casebook, by Bruce Jarrell
4
: structured subject review, practice
questions, and an opportunity to work through clinical cases.
Feedback. The clerkship director should meet with all students at the start of the
rotation to establish expectations. This can be very helpful in terms of receiving
targeted feedback. It is important to request feedback early on in your clerkship – at

77
the very latest by the middle of the clerkship (faculty are required to do this mid-
clerkship but sometimes need some encouragement) – as you will derive the most
benefit from understanding your strengths and weaknesses sooner, and can use it as a
point from which to grow and improve. It is entirely appropriate, and in fact is a
hallmark of the better students, to request feedback at any point in any rotation. Do not
assume if you have not received feedback that you are doing “A” work! Ask your
preceptor on a regular basis, “tell me how I can improve my [write-up/presentation/
clinical assessment].”
Tips for Success
• Take Notes – The best students are seen taking notes in conferences, morning
report, and rounds. Write down words and acronyms you don’t understand, and
ask someone or look them up later. Write down “pearls” and review them at
night. Organize notes in a small notebook that you can keep in your white coat.
Consider purchasing a pocket-guide for surgery (such as the Washington
Manual
5
) and taking notes in it, like a work-book, in pertinent sections.
• Consider what you learn on the clinical services and what you need to know for
the “shelf” exam as complementary but not totally overlapping elements.
• Be an active learner – Ask questions. Listen actively. Don’t doze in conference
or lectures. If you feel yourself getting sleepy in conference, stand up, or
practice tying knots on your coat buttons.
• Immerse yourself in the surgical experience. For example, ask to accompany
the surgeons to talk to the family after a case.
• Be enthusiastic! – Teaching and learning are synergistic experiences. The
more you appear to want to learn, the more energetically your preceptors will
want to teach you.
• Expect to work hard – Recurring comments in the evaluations of the very best
students include “he is exceptionally dedicated to his patients.” Do not be
negative – ever. Complaining is unprofessional and brings the whole team down.
Do not complain about working hard or about being tired. Do not ask to leave
early.
• Be a team player – We are all in the business of excellent patient care as a
priority, with medical education as a close second. There is a certain amount of
“work” that is associated with running a surgical service; find ways to make
yourself useful to your team in any capacity that you can that is appropriate to
your level of training. Do not be afraid to get involved or to ask how you can
help. You will learn from the experience and your team will be appreciative.
• Be punctual: Show up early for rounds, conferences, and meetings. Get to the
hospital early enough so that you can figure out what is going on with your
patients and what happened overnight. If you allow yourself time to get
organized, it will undoubtedly help you perform better and look better. “On time
is late, 15 minutes early is on time.”
• Don’t neglect your own well-being – review the tips in Chapter 6, “Taking
Care of Yourself.” The same principles apply to you as a student.

78
• Don't forget to enjoy the process! If at any point you find yourself fatigued
from the day or a little discouraged, remind yourself how much of a privilege it is
to train in this profession and your reasons for choosing this path.
Other Third-Year Concerns
• Surgery is a very competitive specialty. The Step 1 USMLE score is
unquestionably important for many surgical specialties, and it can play a huge
role in determining an applicant’s interview yield (number of interviews
offered divided by the number of programs applied to, often cited as the best
measure of an applicant’s competitiveness) and ultimate rank list position.
You want to do well on this test. The NRMP Webpage (National Resident
Match Program)
6
contains some useful information on how program directors
value test scores and other factors as well as the relationship between
matching into a given specialty and your USMLE score.
• You want to do well in ALL your clinical rotations, not just the Surgery
clerkship.
• You should try to get involved with research in some capacity while you are a
student, particularly if you are applying to an academic program. With the
possible exception of some of the surgical subspecialties, it is typically not
required that a student’s research experiences be in the surgical field during
medical school. Research experiences and productivity (i.e., publications and
presentations) are generally seen as a positive regardless of the field. There
are a number of opportunities to present your work in Poster format during
the Medical Student Forum of a national meeting, e.g. the American College
of Surgeons Clinical Congress
7
and the Annual Meeting of the Association of
Women Surgeons.
8
FOURTH YEAR CONCERNS
The final year of medical school is distinct from the junior clerkship year in that you will
primarily be thinking about applying for internship positions, as well as choosing
elective rotations that will optimize your success in residency.
Choosing a Residency
It is helpful to have an idea of the career path you would like to pursue at the time you
begin looking at residencies and deciding which ones you want for interviews and
applications. For example, if you see yourself pursuing an academic career, you
definitely will want to apply to university-based programs. If you have in mind
becoming a missionary surgeon or joining a rural practice, you will probably be better
served by a community-based program where you will have a broader exposure to
urology, orthopedics, and obstetrics. If you have a military obligation, your contract
may mandate that you apply to military residencies (see Chapter 7, “Practice Options”).
The e-format version of So You Want to Be A Surgeon: An Online Guide to Selecting
and Matching with the Best Surgery Residency (the “little red book”), published by The

79
American College of Surgeons, is a helpful resource and is updated on a continuous
basis.
9
Also seek advice from the program director/chairman at your home program,
from your mentor/mentors, and from upper classmen (graduating MS4s and interns).
Beyond those caveats, the most important thing to look for in a residency program is a
good “fit” for you. Each residency program has a unique personality and its own
strengths and weaknesses. It is important to trust your instincts, as the residency
program you select ultimately figures far more significantly in your career than where
you went to medical school. The founder of AWS said it best:
Preparing for the Application Process
Most residency programs in the United States utilize the Electronic Residency
Application Service (ERAS), which includes a universal application form, personal
statement, transcripts from your medical school, USMLE scores, and letters of
recommendation.
10
It is important to have your application completely ready to submit
on September 1st. The “Charting Outcomes in the Match” document
6
is a resource for
information on average scores, number of interviews, number of research projects, etc.
Selecting Fourth-Year Electives
One of the best ways to see if a residency program is a good “fit” for you is to do an
elective rotation there in your fourth year. These “audition” rotations, usually
subinternships, are typically done in the summer and fall months and afford you and
the program an opportunity to learn more about each other. These electives are also
good opportunities to get letters of recommendation if done early enough in the fourth
year. It is advisable to choose your externships wisely during this time, as your time will
be best spent at programs for which you are competitive on paper. The only downside
to doing an “audition interview” is that you may have limited exposure to key
attendings during the summer months when many people are on vacation. If possible,
check that they will be in town before you make your plans.
“I find students agonize over getting into "the best program". There is no
such thing. Programs have unique characteristics, are in different locations
and have different faculty. The
fit
is what you need. It may well be more
important to be near family and friends than many characteristics of the
program. There are also no bad programs, but there are bad fits, so the
advice about talking to the residents or even talking to the other students
you meet on the trail about the program at their school is important.”
-- Patricia Numann, MD, FACS, Founder, Association of Women Surgeons
80
Personal Statement
Many students agonize over the personal statement part of the residency application.
As you compose this document, remember that it should showcase characteristics of
yourself that aren’t “visible” in your CV and transcript. You should address what has
prompted you to select surgery. Beyond that, what makes you tick? What unique life
experiences have you had that inform your interest in surgery and/or predict your
success? What do you see yourself doing after residency? There is no one “right” way
to write a personal statement. Give yourself plenty of time to write and revise this
document, and be sure to review it for typos and grammatical errors. Ask your advisor
to read and critique your statement before you submit it.
Letters of Recommendation
The ERAS application requires two faculty letters of recommendation; individual
residency programs may require more and/or require that they be authored by board-
certified surgeons. Some programs ask for a letter from the Department Chair. Even
though you may have worked more closely with a Chief Resident during your clerkship,
you do not want house staff writing a letter of recommendation for you under any
circumstances. Be cognizant of the need for letters of recommendation during your
clinical rotations; the best time to request a letter is when your exemplary clinical
performance is fresh in the mind of the individual faculty member, even if it’s very early
in the year. As letters of recommendation are uniformly laudatory, the only true
advantage you have in this realm is if the letter author is known personally to the
Program Director or Chair of the program where you are applying. Most letter-writers
will ask for copies of your transcript, CV, and personal statement. It is helpful to the
writer to give them a short paragraph highlighting your unique accomplishments,
particularly if these are not immediately apparent from the more formal CV. Offer to
meet with the letter-writer in the summer of your 4th year (well in advance of the
submission deadline) to refresh his or her memory and provide these documents. Be
sure to write a thank-you note to each letter-writer, and follow-up with them after the
Match.
Interviewing
Interviews take place in the fall and early winter months prior to the Match. Spend as
much time as you possibly can at each program you are considering, especially if you
do not have an opportunity to do a rotation there. Do your homework before each
interview; review the American Board of Surgery
11
pass rates for the program at which
you are interviewing. Review the department Website and read about key faculty. If
you know which faculty will interview you, check out their special interests and training
background as potential talking points during the interview.
In your interview, look beyond the obvious statistics about a program (caseload of
graduates, where rotations take place, American Board of Surgery exam pass rate,
etc.); although certainly you will want to know these things. Recognize that the
personality and culture of a given residency program originate, to a large extent, with
81
the Program Director, the service Chief, and the Department Chair and their particular
philosophies of graduate medical education. This is what distinguishes the programs
seen as “family-friendly”, for example. As you interview, it is appropriate to ask the
Program Director to articulate his or her philosophy. Find out how long he or she plans
to remain in the Program Director position, and, if planning to leave, who the likely
successor will be. (Remember you are applying for a position that will last four to six
years, or more!) Ask what the Program Director sees as the biggest challenges of the
residency, as well as its strengths. Find out how many residents drop out of the
program (anything more than 25% attrition is a big danger signal), and what becomes
of them. Ask for an accounting of recent graduates: how many go into private practice,
how many on to fellowship? Ask about the results of the last Surgery Residency Review
Committee Site Visit
12
and if the program received any citations at that time. If citations
were received, ask if these deficiencies been corrected. Ask to see the Surgical Skills
Lab and skills curriculum.
Your interview will include meeting some of the current residents, which gives you an
opportunity to discuss the strengths and weaknesses of the program with a peer.
Inquire about the residents’ attitudes toward each other, and toward their faculty. What
is their perception of faculty availability and level of commitment to teaching? What
would they most like to see changed about the residency? Keep in mind that feedback
about
you
will inevitably be solicited from the resident as well, and the interview is still
two-way. Remember that you, as the applicant, are being evaluated from the very first
e-mail you send to the Program Director’s secretary. Know that anything you say or do
in the presence of faculty/residents/staff during your entire interview visit can be
reported back to the Program Director. Never let your professional guard down.
After each program visit, make notes about your impressions while they are still fresh in
your mind. Be sure to write (hand-written) thank-you notes to all of the programs that
interview you.
Other MS-4 Electives
Beyond subinternships, fourth-year electives should be chosen to optimize your
preparation for residency. While it is tempting to fill the fourth year with “Dermatology
at Waikiki”-type electives, remember this priority. Definitely do an ICU rotation. Do a
Cardiology rotation if you never learned how to read an EKG. A month spent in
Anatomic Pathology may be invaluable, particularly if the residency you choose does
not include it among their required rotations. Other helpful rotations: Pulmonary,
Anesthesia, Radiology, Trauma, and Infectious Disease. Remember that from the very
first day of your internship you will be called “Doctor” (scary but exhilarating!), and will
be expected to have the commensurate knowledge and skills. Consider learning medical
Spanish, as language skills will endear you to your colleagues and your patients.
82
FAQs FOR MEDICAL STUDENTS
As surgical educators we hear the same questions again and again from medical
students who are considering a surgical career.
How do I know if surgery is right for me?
Surgery offers the opportunity to serve, to heal, and to relieve suffering, and is unique
in that the feedback about an intervention is immediate. That said, medicine remains a
calling, and this is no less true of surgery. There are certainly easier ways to make
money, but very few that are as personally rewarding.
Can I do surgery and still have a family/pursue other interests/”have a life”?
Of course! For starters, distinguish in your mind the training years from the rest of your
career. In residency, even “only” 80 hours per week is still a lot of time, and you should
not underestimate the physical and emotional demands that will be made on you, and
the level of commitment required. If you never,
ever
want to get out of bed at 2:00
a.m., then please don’t go into surgery. Even so, many surgical residents maintain
happy marriages, start families, or pursue other goals concomitantly. A knack for
organization and a willingness to accept that some lower-priority things in your life will
need to slide are extremely helpful. Read more in Chapter 6, particularly “Life Balance”.
After residency, your lifestyle will reflect to a large extent what kind of practice you
choose. Clearly, some specialties afford more lifestyle control than others: a surgeon
whose practice is 100% breast, for example, is likely to have more predictable free time
than a transplant surgeon. Call tends to be less demanding for ENT surgeons and
urologists.
Recognize that your college classmates who are in investment banking or who are
junior associates in a law firm are asking themselves these same questions. Balancing
work and family is a front-burner issue for all young people just entering a time-
consuming and demanding career field, and is not unique to surgery.
Can a surgeon work part-time?
Many surgeons have found satisfying less-than-full-time positions. Women surgeons
may be particularly interested in doing this when their children are little. It is easier to
negotiate a part-time position in academic and hospital-based practices, and much
harder to do in private practice, as a surgeon working part-time must still pay “full-
time” malpractice premiums. It is, however, almost impossible to
train
on a part time
basis, but the American Board of Surgery has become more lenient about allowing time
off for family reasons.
11
How important is a mentor, and how do I find one?
A mentor may be defined as “an influential senior sponsor or supporter.” Mentors serve
as role models, and as such, may exhibit some characteristic that helps you particularly
83
to identify with them, such as race or sex. Ideally, a mentor will nurture your
developing talents in surgery, and offer guidance and advice. A good mentor can
suggest research projects to pursue, training programs to consider, and provide
sustenance through personal hardship. AWS maintains a searchable database for
mentors, for the benefit of its members.
While finding the perfect mentor may seem to be the holy grail, realize that different
individuals can serve as mentors at different points in your career. You may have one
surgical faculty member whose mentoring of you involves primarily counseling about
research, while you seek another faculty member’s opinion on personal matters.
What are the biggest problems facing surgery?
There is no question that two of the biggest issues facing not just surgery, but all of
organized medicine, are rising malpractice costs and declining reimbursements. Surgical
specialties pay disproportionately high malpractice insurance premiums, and in some
states this has reached crisis proportions where surgeons and obstetricians are closing
their practices and leaving the state.
The American College of Surgeons
7
is the voice of organized surgery, and has been an
active political force on these and other issues of particular interest to surgeons,
lobbying Congress and working with the American Medical Association.
13
As a medical
student you are eligible to join the ACS as a medical student member ($20), and you
are encouraged to do so.
REFERENCES
1.
Carlos Pestana Review Notes for Surgery
.
http://www.uky.edu/~amwill7/Pestana%20SURGERY%20REVIEW.pdf Accessed
6.12.12
2. Case Files Surgery (Lange Case Files, 4
th
Edition. McGraw Hill 2004)
3. Kaplan Medical USMLE Step 2 CK Qbook
. (5
th
Edition 2008. Kaplan Publishing
New York)
4. NMS Surgery Casebook (National Medical Series for Independent Study, 5
th
Edition 2007. Lippincott, Williams and Wilkins)
5. The Washington Manual of Surgery. (Klingensmith ME et al. 6
th
Edition.
Lippincott, Williams and Wilkins.)
6. National Resident Match Program (NRMP). http://www.nrmp.org/ Accessed
6.12.12.
7. American College of Surgeons http://www.facs.org/ Accessed 6.12.12
8. Association of Women Surgeons http://www.womensurgeons.org Accessed
6.12.12
9. American College of Surgeons “Little Red Book”
http://www.facs.org/residencysearch/ Accessed 6.12.12
10. Electronic Residency Application Service https://www.aamc.org/services/eras/
Accessed 6.12.12
84
11. American Board of Surgery http://www.absurgery.org/ Accessed 6.12.12
12. ACGME Surgery Residency Review Committee
http://www.acgme.org/acWebsite/navPages/nav_440.asp Accessed 6.12.12
13. American Medical Association Resources for Medical Students
http://www.ama-assn.org/ama/pub/medical-students/medical-students.page?
Accessed 6.12.12
RESOURCES FOR MEDICAL STUDENTS
1. http://www.facs.org/memberservices/medicalstudent.html The ACS Website.
Additional information and advice about selecting and applying for residencies is
available here.
2. http://www.acgme.org/acWebsite/home/home.asp. The ACGME Website, which lists
all accredited residency programs in the US.
3. http://www.ama-assn.org/ama/pub/category/2997.html. The Fellowship and
Residency Interactive Data Base, maintained by the AMA, allows a search of residency
programs by specialty, location, and additional criteria, such as size or whether part-
time/shared positions are available.
4. http://www.nrmp.org/ Information about the National Resident Match Program.
5. http://www.aamc.org/students/eras/start.htm The home page of the Electronic
Residency Application Service.
6. http://www.aamc.org/students/cim/ Run by the AAMC, this is an online career
planning program designed to help you choose a medical specialty and select and apply
to a residency program.
7. http://www.womensurgeons.org/ Home page of the Association of Women Surgeons.
Member benefits include access to an electronic searchable mentor database.
8. http://www.nrmp.org/data/index.html
the annual “Charting Outcomes in the Match”
report.

85
APPENDIX
The appendix is organized as follows:
• ELECTRONIC RESOURCES
• ABSITE
o Review Courses
o Texts
o Websites
• SURGICAL BIBLIOGRAPHY
o Textbooks
o Operative Texts
o Atlases
o Surgical References Available in Electronic Format
o Handbooks
o Supplementary Resources
o Subspecialty Texts
• SURGICAL ORGANIZATIONS, SPECIALTY SOCIETIES, AND
ASSOCIATIONS
• CAREER DEVELOPMENT RESOURCES
ELECTRONIC RESOURCES
Working knowledge of computer technology in medicine is essential for all surgical
residents. From the operating room to the office, the surgeon is faced with constant
technologic advances in equipment as well as the challenges of learning new technical
skills and communicating with Internet-savvy patients. Computer tools can also improve
your quality of life during a surgical residency by improving efficiency. Most hospitals
have an IT department that can assist you with use of the electronic medical record
that may vary with each facility.
Internet Resources
During your resident orientation make sure to stop by the medical library and gain
access to the resources it offers. Most programs will allow you free online access to
many surgical journals and provide you with a search engine for literature review.
Books and journal articles can be requested online and sent by e-mail from your
university library. Often, librarians can perform literature searches for you and e-mail
the results, to make the research process less tedious for you.
86
Literature Searches and Surgical Information Websites
The National Library of Medicine (NLM - www.nlm.nih.gov) is the world’s largest
medical library. MEDLINE is the NLM database most physicians use. The NLM Website
has two different search engines for MEDLINE: PubMed and Internet Grateful Med.
Most medical library computers have a shortcut icon for one or the other. Each is a little
different in the way information is entered, limited and combined, but the tutorials and
trial and error will help you become efficient very quickly. Keep in mind that you can
search by text word, author or journal, and the abstracts can be retrieved for review.
Reading the entire article is always best, but a quick read through an abstract can be
very useful just before conferences and lectures. MEDLINEplus is another NLM site, and
is more directed toward providing medical information to the general public. MEDLINE,
a medical dictionary, a directory of doctors and hospitals, current clinical trials and drug
information can all be accessed from MEDLINEplus.
Ovid.com is a separate site that provides online journals in full text. Most medical
libraries subscribe to Ovid and keep a current list of the journals that participate. Ovid is
the most convenient way of reviewing and copying articles, and can be utilized remotely
by logging-on to the library’s computer system. Ask your librarian for details.
WebMD.com offers quite a bit of consumer information. If you are willing to pay a fee,
there are physician-specific pages, including
Scientific America Medicine
online, CME
credits online, advice for office management, and drug information including
mechanism of action. Access to reviews by subspecialty of recently published articles is
available for free.
MDConsult.com is also available for a fee and is similar to WebMD. It provides access
to items such as multiple online reference books, recent medical news, and literature
searches.
Emedicine.medscape.com is a free Website that offers medical information written
by MDs in various specialties. It’s a great way to obtain information quickly and even
includes a “how to” for certain procedures, along with simplified anatomy images.
MDlinx.com is a free service that provides medical news and information updated
throughout the day. In addition, you can specifically choose surgerylinx.com for news
and information related to surgery.
Vesalius.com is a very useful site with access for a nominal fee. It has an emphasis on
providing case studies by subspecialty. Geared toward surgical education, the cases
include illustrations and operating room photographs pertinent to the cases. There are
also excellent anatomic illustrations.
87
Websurg.com is an excellent free Website that focuses on laparoscopic surgery, and
includes educational sessions and videos.
Besttrial.intumed.com is a surgical training Website geared toward ABSITE
preparation for PGY1 and PGY2 residents. Upon purchasing a subscription, users gain
access to a vast collection of tutorial sessions and practice questions.
Achoo.8media.com is one of the most user-friendly, comprehensive directories of
Internet medical sites available. The main gateway to the site is divided into Business
and Finance, Organizations and Sources, Human Health and Disease Directory and
Reference Sources. The site is indexed by search, news, commerce and communities.
In a matter of minutes you can locate online CTs, surgical atlases, patient support
groups, and even the latest projects in surgical robotics.
Uptodate.com is an evidence-based knowledge system authored by physicians to help
clinicians make the right decisions at the point of care. All UpToDate.com content is
written and edited by a global community of 4,800 physicians, world-renowned experts
in their specialties.
Portable Electronic (“Smart”) Devices
Smartphones and electronic tablet devices are great alternatives to the standard laptop
computer since they are lightweight and can readily fit into your white coat pocket.
Each year, more “classic” surgical textbooks and journals become available in electronic
format, making it easier to have many references at your fingertips. Moreover, many
excellent software programs are available free of charge, including animations or
simulations of surgical procedures that may be hard to comprehend just by reading
text. Check your university bookstore as they may offer discounts on these devices as
well as other computers and software.
More hospitals are transitioning to electronic medical records, and some offer secure
applications for use with your portable electronic device. You can check patient charts,
enter orders, and check radiologic imaging from the comfort of your home on your
personal device. Check with your hospital IT department for details.
CNET.com is an excellent consumer resource to compare the various electronic devices
available on the market, including tablets, laptops and phones available on the market.
It covers general computer technology and gives a detailed breakdown of the different
devices in table format. Consumer reviews are available and are very informative.
PDAmd.com is a Website dedicated to mobile personal hand-held computers for
physicians. Reviews of the various products compare them based on memory, operating
systems, software, size, battery life and speed. Software and medical apps are listed by
device.
88
Epocrates.com has a free comprehensive drug list app for the hand-held computer
that includes mechanism of action, pregnancy and lactation, pediatric dosing, etc., and
it has a function for auto updates when you synchronize it with your PC. The site also
sells other downloadable medical apps, indexed by device brand.
Med-ia.ch/medcalc is an app designed for use in small-screen mobile devices for
rapid calculation of common equations used in clinical medicine, including
anesthesiology, pediatrics, emergency, intensive care and internal medicine.
Skyscape.com is a comprehensive resource for mobile medical references. You can
search by medical specialty, and a variety of classic texts in electronic format are
available for purchase.
ABSITE
Review Courses
The ABSITE Review Course (http://www.absitereview.com) is a 2-day intensive course
that is specifically targeted to surgery residents taking this exam. You get a nice
handbook to utilize during the course, which then serves as a great review tool one to
two months before the exam. It is not directly intended to prepare you for written or
oral boards. You can decide when you want to take the course; it is taught four times
during the year at different locations throughout the United States. Take it in October if
you’d like to take the course early in your study process to help you set up a study plan.
If you’d like to study first by yourself, and use the course as a concentrated review/
testing tool for yourself towards the end of your study period, then take it in December
or January. This course is not suitable for everyone, so talk to a colleague who has
attended it before investing the time and money in the program.
ABSITE Texts
Our favorites are indicated by asterisks (**).
ABSITE Combat Manual
, The Red Manual for the Surgery Boards, and Surgery 101:
Basic Science Review, Volumes I&II. (Hratch and Raffy Karamanoukian, 2000,
Magalhaes Scientific Press.) The Combat Manual
gives bullet statements hitting testable
topics, while the other two have questions with answers. They are OK, but are not the
best study resources. ($89.00, $49.00, and $39.00 per volume respectively.)
**ABSITE Review Manual
. (Richard E. Dean, 2005, Instructional Media Center at MSU.)
This review manual is published annually by the Michigan State University Department
of Surgery specifically for review for the ABSITE exam. They essentially take the
question topics for the exam and provide pertinent information about each topic. Great
for last minute review, you can only obtain it from MSU at 517-353-9929 or
[email protected]/imc. ($49.95)
89
ABSITE Review Manual – Junior (by Richard E. Dean, Michigan State University)
ABSITE Review Manual – Senior (by Richard E. Dean, Michigan State University)
Rush University Review of Surgery, 5th edition. (Deziel et al., 2011, W.B. Saunders,
Inc.) A good paperback review of surgery in question-and-answer format; it is great
for bedside reading. ($48.29)
SESAP: Surgical Education and Self-Assessment Program (American College of
Surgeons.) Reduced pricing for residents and ACS members. This study guide is in a
self-assessment and learning format, with lots of pictures and clinical situations. A
new edition is released every few years. Questions cover all of the 15 major content
areas of general surgery addressed in ABS examinations and include short
bibliographies and a syllabus, with discussion of the correct responses and evidence-
based explanations. It is very useful for studying for the ABSITE and especially for
Boards, particularly if you are tired of reading from a textbook. For more information
look online at www.facs.org. ($200.00 for residents; print or electronic format)
PASS the ABSITE (Rafael Azuaje)
ABSITE Killer (Adam P. Lipkin)
The Surgical Review: An Integrated Basic and Clinical Science Study Guide. (Atluri P.
et al, 2005, Lippincott Williams.)
The Senior ABSITE Review (Steven Fiser, 2006, Lippincott Williams & Wilkins.)
The Practice ABSITE Question Book (Steven Fiser, 2010, Lippincott Williams &
Wilkins.)
General Surgery ABSITE and Board Review (Pearls of Wisdom) (Matthew J. Blecha
and Andrew Brown.)
ABSITE Websites
absite.org – $75.00 for 3 months of access to review material as separate
PowerPoint-based clinical tutorials and a question bank. Offers full-length practice exam
and separate junior and senior review sections. Site created by surgery residents. Does
NOT offer a free trial.
absitereviews.com – $199 for 60 days. Offers basic review and an additional ABSITE
High Yield Series (also $199). Ordering both series at the same time can save you $50.
Primarily a review question bank. Reportedly offers high yield facts and buzzwords.
Does NOT offer a free trial. Prepared and maintained by a group of three physicians.
90
intumed.com – Access available in 3 separate payment groups: 3 months at $225 to
one year at $600. Does offer a demo. Primarily geared for PGY 1 and 2. A collaborative
project between Harvard Medical International and the Royal College of Surgeons in
Ireland, with programming developed by the manufacturer of eLearning environments.
Provides case studies, testing bank and interactive tutorials. Very well designed and
user friendly, however, quite expensive. Good overall resource, not just for ABSITE.
apextesting.com/absiterx – $125 and up. Designed by a professional testing
preparation company. Offers a variety of packages, with study centered around
available online tutorials in PowerPoint format, as well as a question bank. Question
bank has too many USMLE Step One and Two type questions and not enough questions
that are similar to what is actually seen on the ABSITE. Difficult to navigate and no free
trial.
clinicalreview.com – Offers 4 textbooks and a 1000-question bank. Has free demo;
several packages starting at $99 for renewal memberships (with yearly updated review
book) and $175 for a comprehensive course that comes with a review book series. Well
put together and appears easy to use.
passabsite.com – FREE. Offers questions divided into junior and senior level or by
topic. Most answers are correct; a select few that are questionable. Explanations are
available on every question. Great for practice questions while reviewing, and the price
can not be beat!
SURGICAL BIBLIOGRAPHY
Surgical Textbooks
The following list is not exhaustive by any means. These are the books AWS members
most commonly felt were helpful during their residencies. The annotations will help you
decide which will be most useful to you, depending on your program and interests. At a
minimum, we recommend that you buy at least one major text and one atlas. Many of
the books are accessible through medical school bookstores, online, and often at
discount prices. Amazon, Barnes and Noble, and eBay often have cheaper prices, and
sometimes also have used textbooks available. Prices listed may have changed. Our
favorites are indicated by asterisks (**).
These are generally considered the classic surgery textbooks and it is generally
understood that you will study from one of the three. Check with your program to see if
they work from a specific textbook, or have review sessions based on specific chapters
from a text. Other textbooks are available and are listed below under “Supplementary
Resources”. They may be helpful for clinical decision-making or for reviewing disease
processes.

91
**Principles of Surgery, 9
th
Edition. (Seymour I. Schwartz, et al., 2009, McGraw Hill
Text.) This is the most widely-used of all the major surgery textbooks. New chapters
include trauma, transplant, and surgical oncology. Ideally, you should read it cover to
cover during your residency, preferably more than once. If you know the information in
this book, you will do well on all your written exams. ($150.00)
Principles of Surgery: Companion Handbook (Seymour I. Schwartz, et al., 2009,
McGraw Hill Text.) Many residents find the handbook useful to keep at the hospital for
ready reference, but don’t rely on the pocket edition to pass exams.
Principles of Surgery: Pretest and Self-Assessment (Seymour I. Schwartz, et al., 2009,
McGraw Hill Text.) This is useful practice for the In-Service Exams and Boards
preparation.
Principles of Surgery: Pretest and Self-Assessment CD-ROM. (Seymour I. Schwartz, et
al., 2009, McGraw Hill Text.) This includes the text, 27 videos of surgeries (including
laparoscopic surgeries), as well as pretest questions and reviews.
Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 19
th
Edition.
(David Sabiston and H. Kim Lyerly, 2012, W.B. Saunders, Inc.) This is also an excellent
textbook, though somewhat less widely-used and perhaps not quite as readable as
Principles of Surgery. Greater emphasis is placed on the basic sciences. ($165.00)
Textbook of Surgery: Pocket Companion (David Sabiston and H. Kim Lyerly, 2012, W.B.
Saunders, Inc.)
Textbook of Surgery: The Biological Basis of Modern Surgical Practice CD-ROM. (David
Sabiston and H. Kim Lyerly, 2012, W.B. Saunders, Inc.)
Surgery: Scientific Principles & Practice, 5
th
Edition. (Lazar J. Greenfield, 2010,
Lippincott, Williams & Wilkins.) This is a newer entry into the textbook arena, and it is
loaded with photos and diagrams. There is a fairly heavy emphasis on the basic science
aspects, but it is written by some of the same academic surgeons who write Board
questions. The book includes a CD-ROM that contains text from the book as well as a
review (sold separately as a hard copy). ($200.00)
Surgery: Scientific Principles & Practice Study Guide for Surgery. (Lazar J. Greenfield,
2010, Lippincott, Williams & Wilkins.)
Surgery: Mastering Surgical Principles and Techniques CD-ROM for Windows and
Macintosh (Greenfield and Nyhus). This includes the Greenfield textbook and review
book plus Nyhus’ mastery atlas (see below).

92
Current Surgical Therapy, 10
th
Edition. (John Cameron, 2010, B.C. Decker.) This is an
excellent reference for the practicing surgeon and is good preparation for the oral
surgery Boards. It has a stronger emphasis on clinical management and decision-
making, and it is updated every 2-3 years. It does not cover pediatric or transplantation
surgery. ($160.00)
Current Surgical Diagnosis and Treatment, 13
th
Edition. (Doherty, 2009, Appleton &
Lange.) This text is also more clinically oriented, emphasizing major diagnostic features
and descriptions of surgical disease processes. It reviews procedures for evaluation and
management in a concise, practical format. This book includes chapters on essentially
all surgical subspecialties, particularly as they apply to the general surgeon. It is a good
review text before In-Service and Board exams. ($60.00)
Care of the Surgical Patient: Perioperative Management and Techniques. (Scientific
American Medicine.) This is essentially a textbook-subscription combination that
provides continuing quarterly updates to its chapters. It is an excellent reference, and
provides many useful algorithms, comprehensive discussions explaining physiologic
principles, and explanations of the diagnostic and therapeutic recommendations. It is
very well written. This is a large two-volume loose-leaf format publication, though, so it
is much more useful as a home or library reference. Information is available at 1-800-
545-0554 or via mail at P.O. Box 647, Yorktown Heights, New York, NY 10598. (The
basic manual is $299.00 for the first year; renewal is $149.00 per year)
Scientific American Care of the Surgical Patient, 2001. This textbook was prepared in
cooperation with the American College of Surgeons. Previously a loose-leaf text, this
now comes as an annual bound edition ($249.00) or as a CD-ROM that is updated
quarterly ($395.00). Extremely practical in its information, it also gives thorough
explanations of the rationale and physiology for its recommendations. It includes
multiple authorship by some of the finest surgeons in each specialty. It is fairly
expensive, but you may find you like it better than the other standard texts.
Operative Texts
It is very important that you have a reference for technical skills and procedures. Your
program may have a specific one it recommends. There are many good ones; here are
some suggestions:
Dr. Milton T. Edgerton, a plastic surgeon admired for his fine technique, has
written an excellent text, The Art of Surgical Technique
, which beautifully
describes the basics of how to suture, tie, cut, etc. If your professors do not
have the time or patience to instruct you in the nuances of the art of surgery,
this book is a must-read.
Chassin’s Operative Strategy in General Surgery
, edited by Carol Scott-Connor,
describes the basics that most attendings will assume you already know or have
93
read about before any procedures. It is in an algorithm format and is easy to
read, with excellent pictures.
Principles of Surgical Technique: The Art of Surgery, by Gary G. Wind and
Norman M. Rich, is an older but elegantly illustrated volume that describes the
basics of surgical technique.
There are also some very basic tips outlined at the end of Abernathy’s Surgical
Secrets
.
Atlases
**Atlas of Surgical Operations, 9
th
Edition. (Robert Zollinger, 2010, McGraw-Hill.) This
atlas is very popular, has short, concise text, and good illustrations, and it can be
scanned in a few minutes if you are short on time before a case. The latest edition
includes 20 laparoscopic procedures. ($191.00)
Atlas of General Surgery.
(David Sabiston Jr., 1993, W.B. Saunders, Inc.) This newer
entry to the market may supplant the previous “old standards.” It covers nearly
everything but thoracic procedures. ($185.00)
Mastery of Surgery, 6
th
Edition. (Fischer.) This is an excellent two-volume atlas covering
most of the procedures you will encounter. See if it is available in your medical library.
($325.00)
Maingot’s Abdominal Operations Volumes I & II, 10
th
Edition. (Michael Zinner, 1997,
Appleton & Lange.) This is probably THE classic multi-volume set of abdominal surgical
technique. With illustrations and detailed descriptions of techniques, it covers
information on disease processes, diagnostic evaluation, indications for surgery, plus
which technique to use and when. This should be in most hospital libraries, but you
may want to purchase it in your more senior years of residency. ($325.00)
Operative Strategy in General Surgery: An Expositive Atlas, 3
rd
Edition. (Jameson L.
Chassin, 2001, Springer-Verlag.) This is one program’s approach to most types of
general surgical cases, including tips on pitfalls to avoid, anatomic hints, and pre- and
post-operative management. ($212.00)
Atlas of Laparoscopic Surgery. (Garth Ballantyne, 2000, W.B. Saunders, Inc.) If you
need additional insight into laparoscopic techniques, this is a good supplement to your
library. ($134.00)
**Surgical Anatomy and Technique: A Pocket Manual, 3
rd
Edition. (John Skandalakis
et al., 2008, Springer-Verlag, Inc.) This excellent pocket manual is especially good for
you to keep in your locker as an intern. It will give you the basic information you need
to get through operations when you are assigned at the last minute and haven’t had a
chance to read more thoroughly about them. ($39.00)
94
Surgical References Available in Electronic Format
This is a small sample of titles that are available in electronic format. Titles of classic
surgical and medical texts are constantly being released in electronic format; check the
Internet for the most recent updates.
Pocket Surgery contains brief synopses of 110 common operative procedures, including
operative patient positioning, and pre- and post-operative care.
Washington Manual Surgery Survival Guide is a guide for interns that includes handling
intern floor calls, organizing your day, caring for surgical drains, etc.
MD Anderson Surgical Oncology Handbook, 3
rd
Edition is an excellent organ-based
reference for the diagnosis, intra-operative, and management of surgical oncology
patients.
Washington Manual of Surgery, 4
th
Edition is a useful reference regarding common
surgical diseases.
Current Consult: Surgery has clinical answers for common surgical consults; it is very
handy in the ER when seeing consults.
Current Essentials of Surgery has concise descriptions and explanations of common
surgical diseases.
SAGES Manual is a reference for the fundamentals of laparoscopy and GI endoscopy.
Surgical Recall is a good review for inevitable pimp sessions.
Schwartz Principles of Surgery PDA Edition
is a classic reference available for PDA ease-
of-use.
Tarascon Pharmacopoeia
is a popular drug reference that updates automatically when
hot-synching.
Sanford Guide to Antimicrobial Therapy
is the standard reference for antimicrobial
selection and administration.
Netter’s Anatomy Flashcards for PDA
has original Netter drawings for your PDA. It’s a
great review before you step into the OR.
Pocket Advisor - ICU Management
covers the full range of issues that a clinician might
face when treating a patient in the ICU. This includes diagnoses that require ICU care
such as shock, myocardial infarction, cardiac arrest and thromboembolic disorders.

95
Mont Reid Surgical Handbook is a great pocket-ready reference that provides you with
succinct information.
Handbooks
**The Mont Reid Surgical Handbook, 6
th
Edition. (Scott Berry et al., 2008, Mosby
Yearbook, Inc.) Written by residents at the University of Cincinnati and first published in
1987, many students and residents have found this to be an invaluable aid to patient
care and improving the initial management of common surgical problems. The book is
small enough to fit into your white coat or scrub pocket, and is written in an outline
format with an extensive index. The basic principles behind many techniques and the
pertinent anatomy are illustrated with simple black and white drawings. It is highly
recommended. ($52.65)
**Handbook of Surgical Intensive Care: Practices of the Surgery Residents at the Duke
University Medical Center, 5
th
Edition. (Bryan M. Clary et al., 2000, Mosby Yearbook,
Inc.) This book assists in both pre- and post-operative management of SICU patients. It
is another pocket guide written by surgery residents for their colleagues. ($35.95)
Abernathy’s Surgical Secrets, 6
th
Edition. (Alden H. Harken, 2008, Mosby Yearbook Inc.)
A book of “pimp” questions that you may want to review prior to rounds on specific
cases, particularly if the diagnosis is a new one for you. It is also useful as a different
way to review for Oral Surgery Boards. ($40.50)
Surgical Recall and Advanced Surgical Recall. (Lorne H. Blackbourne, 4
th
edition, 2005,
Williams & Wilkins.) Written in question and answer format, these are filled with
questions that you will be asked in the operating room and on rounds. Surgical Recall
covers basic information that may be more appropriate for medical students. Advanced
Surgical Recall contains more in-depth information and covers some subspecialty
surgery services; it does not include the basic information found in Surgical Recall
.
($40.00/$60.00)
Supplementary Resources
**Selected Readings in General Surgery. A subscription to what was originally the
Parkland Papers
, from the University of Texas Southwestern Medical Center and is now
administered through the ACS, it provides you with a packet of 45 to 60 articles from
assorted specialty journals (11 times per year), accompanied by a summary of the
current trends and thinking on a particular body system. The cycle takes about three
years to complete. Reading the summary each month is an excellent way to study on a
regular basis. A 30-day free trial to the online premium service is available.
Subscriptions can be obtained through the ACS Website ($285 annually for the print
edition, $255 for CD-ROM).
96
**The Art of Surgical Technique. (Milton T. Edgerton, 1988, Williams & Wilkins.) This
book beautifully describes the basics of knot-tying, suturing techniques, making
incisions, etc. If no one seems to have the time to demonstrate good surgical technique
to you, this book is a must. ($79.99)
**Operative Dictations in General and Vascular Surgery: Operative Dictations Made
Simple. (Jamal J. Hoballah and Carol E.H. Scott-Conner 2003, Springer.) This book
outlines 155 general and vascular surgery operations, including set-up, steps and
potential pitfalls. It is an excellent resource for case preparation as well as dictating
after the case. It also comes with a handy PDA application. ($50.00)
**The Physiologic Basis of Surgery, 4
th
edition. (J. Patrick O’Leary, editor, 2007,
Williams & Wilkins.) This is everything you should have learned in the first two years of
med school in one book. It has essential information for the ABSITE exam. ($130.49)
Surgical Decision Making, 5
th
Edition. (Lawrence Norton et al., 2004, W.B. Saunders,
Inc.) This is a book of algorithms that can help you work your way through a variety of
clinical situations. It is very helpful in your more senior years or when preparing for
conferences. ($600)
**Cope’s Early Diagnosis of the Acute Abdomen, 22
nd
Edition. (William Silen, 2010,
Oxford University Press.) This is the classic guide to physical diagnosis. It is a great
concise and small book that will hone your history-taking and physical examination
skills. Changes have been made from the classical writings to modernize the book,
including a new discussion of CT findings and the elimination of obsolete practices and
diagnoses. The whole book can be read cover-to-cover in the course of a quiet night on
call. You should read it in toto as a medical student, intern, and at least two more times
during your residency. ($33.48)
**Residents as Teachers: A Guide to Educational Practice
. Send $12.00 for the 84-page
book to Dr. Neal Whitman, Department of Family and Preventive Medicine, University of
Utah School of Medicine, 50 N. Medical Drive, Salt Lake City, UT 84132.
Subspecialty Texts
Critical Care, 4
th
Edition. (J.M. Civetta et al., 2008. Williams & Wilkins.) If you will be
doing a lot of ICU work as a resident or in practice, this is the finest text available. If
not, borrow a copy for reference while doing your ICU rotations. ($225.00)

97
The ICU Book, 3
rd
Edition. (Paul Marino, 2006, William & Wilkins.) This is a great
paperback resource for any resident doing an ICU rotation. It has a problem-based
approach to ICU, with a good review of principles of basic science, calculations,
treatments and dosing regimens that will come in handy. ($75.99)
Trauma Handbook. (E.E. Moore, 2001, Appleton and Lange) and Manual of Trauma
Critical Care Procedures. (E.E. Moore et al., 2001, Mosby Yearbook.) These two books
are written by the authors of Trauma
, the premier textbook on the subject, which is no
longer in print. If your program has a high volume trauma service, they may be worth
considering.
SURGICAL ORGANIZATIONS, SPECIALTY SOCIETIES, AND ASSOCIATIONS
There are a variety of organizations that oversee the world of surgery outside the
operating room. Some were established to ensure quality education, some set the
standards for licensing, and others represent surgeons to governmental agencies.
Below are descriptors of the major organizations likely to play a role in your world as a
surgical trainee.
Most medical associations have Websites detailing the mission of the organization,
contact and membership information and news about upcoming meetings. Some of the
subspecialty associations also include information about fellowship programs.
• Association of Women Surgeons (www.WomenSurgeons.org
-
our personal
favorite).
This site provides a full online copy of this
Pocket Mentor
as well as
conference information, membership, etc. Check out the Career Development
Resources (CDR) section for articles on various career aspects.
• Association for Academic Surgery (www.aasurg.org) This site is dedicated to
research-based academic surgery. They strongly encourage resident
participation.
• Association for Surgical Education (www.surgicaleducation.com) This site is
dedicated to improvements in teaching the art and science of surgery to medical
students and residents.
• Society of American Gastrointestinal Endoscopic Surgeons
(www.sages.org) This site is for surgeons interested in minimally invasive
surgery and endoscopy. They have a candidate member group for residents.
• American Society of Colon and Rectal Surgeons (www.facrs.org)
• American Society of Breast Surgeons (www.breastsurgeons.org)
• American Society of Plastic Surgeons (www.plasticsurgery.org)
• Society of Surgical Oncology (www.surgonc.org)
• Society of Thoracic Surgeons (www.sts.org)
• American Society of Transplant Surgeons (www.asts.org)
• American College of Obstetricians & Gynecologists (www.acog.org)
• American Academy of Orthopaedic Surgeons (www.aaos.org)
• American Association of Neurological Surgeons (www.neurosurgery.org)
98
• The Residency Review Committee for Surgery (RRC) inspects residencies
on a regular basis (at least once every five years), for purposes of accreditation.
Approval or disapproval is based on the quality of surgical education,
documentation of adequate case volume for each surgical resident, passage rate
of the Board examinations, the number and academic activity of the faculty, etc.
This is the organization that oversees the quality of the educational experience at
each program. If you ever want to know the requirements for all types of
residencies, you can check the Common Program Requirements and the Program
Requirements for each specialty on the ACGME Website. Prospective applicants
MUST be informed if a program is on probation and should be informed of
citations from their most recent RRC site visit. Your Program Director is the one
responsible for ensuring your program and each surgical resident meet the
requirements of the RRC. You must complete a surgical residency approved by
the RRC in order to sit for your surgical Boards. (www.acgme.org)
• The American Board of Surgery (ABS) is the certifying organization for
general surgery. Based in Philadelphia, this group administers the two Board
exams (Qualifying or written and Certifying or oral). You become Board Certified
by passing these two examinations. (If you have completed and approved
residency but have not yet passed these examinations you are considered Board-
eligible.) In your Chief year, you need to contact them for an application for the
Board exams (see Chapter 6 on “Board Certification”). The ABS also sells the
ABSITE or in-service exam to surgical programs. (www.absurgery.org)
• The American College of Surgeons (ACS), the premier organization
representing surgeons in the United States, is based in Chicago. You can and
should join as a resident member for $25 per year. This allows you to buy SESAP
for a much-reduced price, admits you to the annual Clinical Congress held each
October for free if you can attend, puts you on their mailing list, and provides
you with the monthly
Bulletin
, which will open your eyes to some of the
socioeconomic and political issues facing surgeons. A Fellow is a full member of
the ACS. You must be Board certified, in practice for at least one year in the
same location, and pass interviews by Fellows active in your state’s chapter.
Membership of the American College of Surgeons entitles you to write FACS after
your MD. The main governing body of the ACS is the Board of Regents. There
are 21 Regents plus the President of the ACS. A number of committees, as well
as the Board of Governors, advise the Regents. The Board of Governors consists
of 264 representatives – from each area of the country, the major subspecialty
organizations and international organizations. They are elected by the Fellows
and are the voice of the practicing surgeon to the ACS. (www.facs.org)
• The American Medical Women’s Association (AMWA) is the largest women’s
medical organization in the U.S. They have been active for many years in trying
to improve the status of women in the medical profession, as well as women’s
healthcare overall. Their journal (JAMWA) contains many articles of interest to
women physicians. (www.amwa-doc.org and www.jamwa.org)
99
• The Association of American Medical Colleges (AAMC) oversees medical
teaching institutions. This organization generally has a Women’s Liaison Officer
(AAMC-WLO) assigned as the contact person between each of the teaching
hospitals and medical schools and the AAMC. Usually, this person has the most
reliable information on your institution’s policies about gender-related issues,
from sexual harassment to maternity leave, so identify this person early on.
Some of these people are great resources, and can be very helpful to you. The
AAMC has been very active in promoting fair working environments for women in
the medical teaching institutions. (www.aamc.org)
Below are additional organizations that play a major role in “organized” surgery and are
good contact points. This list is by no means inclusive of all the associations. For the
most part, the capital letters in each title form the acronym for that association.
• American Academy of Facial Plastic and Reconstructive Surgery
(www.aafprs.org)
• American Academy of Ophthalmology (www.aao.org)
• American Academy of Otolaryngology-Head & Neck Surgery, Inc.
(www.entnet.org)
• American Academy of Pediatrics, Surgical Section
(www.aap.org/sections/surgery)
• American Association for Hand Surgery (www.handsurgery.org)
• American Association for the Surgery of Trauma (www.aast.org)
• American Association for Thoracic Surgery (www.aats.org)
• American Association of Genitourinary Surgeons (www.aagus.org)
• American Association of Plastic Surgeons (www.plasticsurgery.org)
• American Burn Association (www.ameriburn.org)
• American Gynecological and Obstetrical Society (www.agosonline.org)
• American Head and Neck Society (www.ahns.info)
• American Laryngological Association (www.alahns.org)
• American Medical Association (www.ama-assn.org)
• American Ophthalmological Society (www.aosonline.org)
• American Orthopaedic Association (www.aoassn.org)
• American Otological Society (www.americanotologicalsociety.org)
• American Pediatric Surgical Association (www.eapsa.org)
• American Surgical Association (www.americansurgical.info)
• American Urological Association (www.auanet.org)
• American Society for Aesthetic Plastic Surgery (www.surgery.org)
• American Society for Bariatric Surgery (www.asbs.org)
• American Society for Surgery of the Hand (www.assh.org)
• Association of American Medical Colleges (www.aamc.org)
• Association of Program Directors in Surgery (www.apds.org)
• Association of VA Surgeons (www.vasurgeons.org)
• Association of Women Surgeons (www.WomenSurgeons.org)

100
• Central Association of Obstetricians and Gynecologists (www.caog.org)
• Central Surgical Association (www.centralsurg.org)
• Congress of Neurological Surgeons (www.neurosurgeon.org)
• Eastern Association for the Surgery of Trauma (www.east.org)
• International Society for Cardiovascular Surgery (www.isvs.com)
• Midwest Surgical Association (www.midwestsurg.org)
• National Medical Association (www.nmanet.org)
• New England Surgical Society (www.nesurgical.org)
• North Pacific Surgical Association (www.nopacsurg.org)
• Pacific Coast Surgical Association (www.pac-coast-surg.org)
• Peripheral Vascular Surgery Society (www.pvss.org)
• Royal College of Physicians and Surgeons of Canada (www.rcpsc.medical.org)
• Society for Clinical Vascular Surgery (www.scvs.vascularweb.org)
• Society for Pediatric Urology (www.spuonline.org)
• Society for Vascular Surgery (www.vascularweb.org)
• Society for Surgery of the Alimentary Tract (www.ssat.com)
• Society of Gynecologic Oncologists (www.sgo.org)
• Society of Neurological Surgeons (www.societyns.org)
• Society of Thoracic Surgeons (www.sts.org)
• Society of University Otolaryngologists (www.suo-aado.org)
• Society of University Surgeons (www.susweb.org)
• Society of University Urologists (www.suunet.org)
• Southeastern Surgical Congress (www.sesc.org)
• Southern Neurosurgical Society (www.southernneurosurgery.org)
• Southern Surgical Association (www.southernsurg.org)
• Southern Thoracic Surgical Association (www.stsa.org)
• Southwestern Surgical Congress (www.swscongress.org)
• Surgical Infection Society (www.sisna.org)
• Triological Society (www.triological.org)
• Western Surgical Association (www.westernsurg.org)
• Western Thoracic Surgical Association (www.westernthoracic.org)
CAREER DEVELOPMENT RESOURCES
Organization and Setting Goals
Time Power
. (Charles R. Hobbs, Harper & Row, 1987.) One of many time management
schemes available for increasing your productivity. This one is designed to work best
with a Day-Timer, Day-Runner, Franklin Planner, or similar daily planner calendar.
The Seven Habits of Highly Effective People: Restoring the Character Ethic. (Steven R.
Covey, Simon & Schuster, 1989.) This is a principle-oriented book that demonstrates
how to achieve balance in your life and profession by better understanding yourself and
101
your own motivations. It provides a step-by-step outline for becoming a more effective
person by improving communication and cooperation.
First Things First.
(Stephen R. Covey, A. Roger Merrill, and Rebecca R. Merrill. Simon &
Schuster, 1994.) This is a very practical guide to setting priorities, finding balance in
your life and time, and getting things done most efficiently.
Understanding Differences Between Women and Men
**You Just Don’t Understand: Women and Men in Conversation
. (Deborah Tannen,
PhD, William Morrow & Co., 1990.) This has observations by a sociolinguist on how
men and women communicate, and why they so often do not understand one another.
This can help to decipher what men and women are really saying, and how you can
better communicate with them to avoid misunderstandings.
**Hardball for Women
. (Pat Heim, PhD, Plume Books, 1993.) Written primarily from a
business point of view, this book is an excellent explanation of the stereotypical
behaviors of men and women that create conflicts and misunderstandings. Heim’s basic
premise is that boys and girls learn the lessons of life from the games they play, and
expect adulthood to follow the same rules. You will recognize a multitude of situations,
and Heim offers very concrete strategies to succeed.
Men: A Translation for Women
. (Joan Shapiro, New American Library-Dutton, 1992, or
Avon 1993.) This is another highly-readable book on understanding the differences in
communication styles between men and women.
Dealing with Attitudes
Forgive and Remember. (Charles Bosk, The University of Chicago Press, 1979.) This
covers the psychology of residency and the hierarchy in surgery. It helps you
understand some of the indoctrination process of residency.
The Gentle Art of Verbal Self-Defense
. (Suzette Elgin, Reston Press, 1985.) An excellent
guide to defending yourself against verbal attacks without jeopardizing your own
situation, it includes suggestions for redirecting and deflecting a verbal assault.
**They Can Kill You...But They Can’t Eat You
. (Dawn Steel, Pocket Books, 1993.) A very
entertaining look at one woman’s battle to succeed in the film industry, this also
provides a number of useful insights into how to succeed in a man’s world.
How to Win Friends and Influence People
. (Dale Carnegie, Pocket Books, Reissue
1994.) This classic book on communicating uses vignettes from real life to illustrate
effective leadership. It’s easy and fast reading, and well worth the time.
102
Conflict Management
There are many helpful tomes on conflict management and resolving interpersonal
conflict in the professional and personal arenas. Some of our favorites are:
Tongue Fu!: How to Deflect, Disarm, and Defuse Any Verbal Conflict. (Sam Horn,
1997, St. Martin's Griffin.) A delightful book full of practical tips on specific
techniques and skills that can be put to immediate use in everyday situations.
Coping with Difficult People: The Proven-Effective Battle Plan That Has Helped
Millions Deal with the Troublemakers in Their Lives at Home and at Work.
(Robert M. Bramson, 1988, Dell.) This book teaches how to identify difficult,
destructive, problematic behavior in people, and how to cope with it.
Getting Past No: Negotiating in Difficult Situations
.
(William Ury, 1993, Bantam.)
Along with the best-selling companion book, Getting to Yes: Negotiating
Agreement Without Giving In (re-released in 2011), these works offer proven
steps to negotiating personal as well as professional disputes.
Pregnancy and Residency
The May/June 1993 issue of the
Journal of the American Medical Women’s Association
was devoted to maternity and medicine. It includes articles on the pregnant resident,
colleagues’ attitudes, and the rights, rules and regulations regarding maternity leave.
Single copies are available for $5.00 by writing to AMWA, 801 North Fairfax Street,
Alexandria, VA 22314. (www.amwa-doc.org)
Medicine and Parenting. This is a booklet prepared by the AAMC that covers the timing
of pregnancies in relation to residency, legal rights, leave policies, how to handle
queries about childbearing plans during interviews, child care options, and more. Copies
are available through the Women’s Liaison Officer at your medical school, or by sending
$11.00 to AAMC, 2450 N Street NW, Washington, DC 20037-0400. (www.aamc.org)
“A Pregnant Surgical Resident? Oh My!”
(Emina Huang, MD, and Olga Jonasson, MD.
JAMA
1991;265;2859-2860.) This article discusses how one residency program dealt
with the issue in a purposeful and constructive manner, and is very helpful with
suggestions for maintaining good communications.
Sexual Harassment and Gender Discrimination
Step Forward: Sexual Harassment in the Workplace. What You Need to Know! (Susan L.
Webb, 1991. Mastermedia Publications.) This is a fairly concise book that explains the
differences in harassment and discrimination, and how to deal with problems that arise.
103
Guidelines for Establishing Sexual Harassment Prevention and Grievance Procedures.
(Prepared by the AMA.) Copies are available by writing to AMA, 515 North State Street,
Chicago, Illinois 60610. This brochure is an excellent reference if you wish to help your
program establish a specific policy on these issues, or even just to understand
definitions and the hazards of amorous relationships between people of unequal status.
While most medical schools and universities do have such policies, it is still very
common for residency programs not to have them.
Spiritual Aspects
Healing Words: The Power of Prayer and the Practice of Medicine. (Larry Dossey, MD,
1993, Harper Collins.) An internist reviews the scientific evidence that prayer
complements, though does not replace, good medicine. It includes studies
demonstrating that belief in a treatment by doctors and patients increases its efficacy.
Beyond the Relaxation Response
. (Herbert Benson, MD, 1984, Times Books.) This
reviews various ways to meditate and the physiologic changes that occur with awake
relaxation techniques.
Fire in the Soul: A New Psychology of Spiritual Optimism.
(Joan Borysenko, PhD, 1993,
Warner Books.) Several methods of prayer and meditation are explained by a
psychophysiologist. It will appeal to a variety of people’s styles and belief systems. The
author has several other books available that also describe the “mind/body connection”,
and she helped found The Mind/Body Clinic at Harvard. Her original research dealt with
investigations into the neurophysiology and immunology of somatic ailments such as
migraine, irritable bowel syndrome, etc.
Final Exam: A Surgeon's Reflections on Mortality. (Pauline W. Chen, MD, 2007, Knopf.)
A brilliant young transplant surgeon brings moral intensity and narrative drama to the
most powerful and vexing questions of medicine and the human condition.
Women in Surgery
Forged by the Knife: The Experience of Surgical Residency from the Perspective of a
Woman of Color. (Patricia L. Dawson, 1999, Open Hand Pub.)
The Woman in the Surgeon’s Body. (Joan Cassell, 1998, Harvard University Press.)
Walking Out on the Boys. (Frances K. Conley, 1999, Farrar Straus & Giroux.)
Academic Careers
Why So Slow?: The Advancement of Women
. (Virginia Valian, Reprint 1999, MIT Press.)

104
“Career development in academic medicine.” (W. Applegate.
Am. J. Med
1990;88:263.)
“The status of women at one academic medical center: Breaking through the glass
ceiling.” (
JAMA
1990;264:1817.)
JAMWA
(Journal of the American Medical Women’s Association) has many articles that
you may find helpful. You can get a subscription to the magazine by joining AMWA.
Write to 801 North Fairfax St., Suite 400, Alexandria VA 22314. (www.amwa-doc.org)
“Meeting the challenges of research and a family.” (W.A. Hsueh.
JAMWA
1993;48:55.)
Annotated Bibliography of Women in Medicine 1983-1993. (Beverly Walters, MD, and
Irene McNeill, OMA.) Published by the Ontario Medical Association, this is an excellent
base for easily finding articles related to women, medicine, and associated issues.
Available by mail order through OMA, 525 University Ave, Suite 300, Toronto, Ontario
M5G 2K7, Canada. Enclose a check for $48.15, which includes postage and handling.
(www.oma.org)
105
QUOTES
The following quotes may help pull you through from time to time. Some are humorous,
and some are motivational. When you are feeling glum or discouraged, flip back to
these pages to help get you back into a more positive frame of mind.
Always put the patient first, despite what might be going on in your day or life...It’s not
just the knowledge you have as a physician but the bedside manner you develop and
the way you treat patients that has a lasting effect on them.
-- Stephanie Altobellis, MD,
(quoted in
Life in Medicine
, Vol. 1, No. 5, 1993, p. 15.)
The difference between a successful person and others is not a lack of strength, not a
lack of knowledge, but rather is a lack of will.
-- Vincent Lombardi
Accept the challenges so that you may feel the exhilaration of victory.
Success is a journey, not a destination.
The man on top of the mountain did not fall there.
Do not follow where the path may lead; go instead where there is no path and leave a
trail.
-- Ralph Waldo Emerson
In the middle of every difficulty lies opportunity.
When you aim for perfection, you discover it’s a moving target.
-- George Fisher
There are no secrets to success. It is the result of preparation, hard work, and learning
from failure.
-- Gen. Colin L. Powell
Blessed is the person who is too busy to worry in the daytime and too sleepy to worry
at night.
-- Leroy Aikman
Talent is a flame. Genius is a fire.
-- Bern Williams
Ability will never catch up with the demand for it.
-- Malcolm S. Forbes
A stumble may prevent a fall.
-- English proverb
Some folks pay a compliment like they went down in their pocket for it.
-- Kim Hubbard
The man who removes a mountain begins by carrying away small stones.
-- Chinese
proverb
Be tough-minded but tender-hearted.
106
The Four “A’s” to success in surgery: accountability, availability, affability, and ability
(and usually in that order).
Laugh a lot -- a good sense of humor cures almost all of life’s ills.
Strive for excellence -- not perfection.
Your mind can only hold one thought at a time, make it a positive and constructive one.
Try not to become a man of success but a man of value. --
Albert Einstein
Every artist was first an amateur. --
Ralph Waldo Emerson
Work spares us from three evils: boredom, vice, and need. --
Voltaire
Every failure brings with it the seed of an equivalent success. --
Napoleon Hill
One who fears failure limits his activities.
Failure is only the opportunity to more intelligently begin again. --
Henry Ford
Life isn’t all beer and skittles. --
Thomas Hughes
There is a certain relief in change, even though it be from bad to worse; as I have
found in traveling in a stage-coach, that it is often a comfort to shift one’s position and
be bruised in a new place. -- Washington Irving
Be fair with others, but keep after them until they’re fair with you. --
Alan Alda
Happiness is a conscious choice. --
Mildred Barthel
Everyone must row with the oars he has. --
Dutch proverb
Trust yourself. You know more than you think you do. --
Benjamin Spock
Who makes timid requests, invites denial. --
Seneca
When you reach the end of your rope, tie a knot and hang on. --
Franklin D. Roosevelt

