
Medicaid Managed Care
Provider Investigative Report
Reporting Instructions & Guidelines
Revised January 2024

2
Purpose
The terms of the Medicaid Managed Care/Family Health Plus/HIV Special Needs Plan/Health and
Recovery Plan Model Contract, section 18.5(a)(viii)(F), require Managed Care Organizations (MCOs)
to submit a Provider Investigative Report to the Office of the Medicaid Inspector General (OMIG) and
the Department of Health (DOH) monthly.
The Provider Investigative Report informs OMIG and DOH of any Medicaid provider investigative,
educational, or re-educational activities performed by the MCO or its subcontractors, including all
overpayments recovered. In addition to reporting investigative activities, the MCO must also upload
copies of all Medicaid-related settlement agreements.
This guidance has been updated and is current with the March 1, 2019, Medicaid Managed
Care/Family Health Plus/HIV Special Needs Plan/Health and Recovery Plan Model Contract, and
subsequent agreements.
Report Submission Schedule
The Provider Investigative Report must be completed and submitted monthly. Each monthly report is
due in accordance with the following submission schedule. Note: When the due date falls on a non-
business day, the report is due on the following business day.
Provider Investigative
Report
Submission Schedule
# For the Report Period (2024) Report Submission Due Date
1
January
February 2
9
2
February
April
1
3
March
April 30
4
April
May 31
5
May
Ju
ly 1
6
June
July 31
7
July
September 3
8
August
September 30
9
September
October 31
10
October
December 2
11
November
January 2
12 December January 31
Reporting Instructions and Data Definitions
GENERAL INFORMATION
The Provider Investigative Report is a monthly report of Medicaid funds the MCO identified or
recovered, and any educational or re-educational activities performed. MCOs can request an
extension but will only be allowed a maximum of two extension requests per calendar year.
Medicare or commercial funds the MCO identified or recovered should not be reported on the
3
Provider Investigative Report. Please note information included in the report should be selected from
the drop-down menu options wherever possible. Information should not be copied and pasted from
another source where drop-down menu options are provided.
REPORT COMPONENTS
MCOs are required to submit each monthly report through the Health Commerce System’s (HCS)
Healthcare Financial Data Gateway application’s Universal Data Collection System (UDCS) software,
and report the following:
(A) Detail of All Medicaid Audit or Investigative Activities
MCOs will utilize the Provider Investigative Report to provide case-level detail about any
Medicaid recoveries or educational activities they have undertaken during the relevant
reporting period. This includes unique identifiers for the provider, information related to the
allegation and scope period, as well as recovery amounts when applicable.
(B) Copies of Settlement Agreements (as separate attachment(s))
The MCO will provide copies of all Medicaid-related settlement agreements executed with a
provider during the reporting period. Settlement agreements must be uploaded to HCS as
PDF files (or in the case of multiple files, a zip file containing PDF files of the settlement
agreements). All PDF files must be in a searchable format.
In addition, each individual settlement agreement must be named in the following format:
MCO Name_Settlement_Agreement_[Unique Case ID].
(C) Attestation
The MCO’s Chief Financial Officer is required to attest to the accuracy of the Provider
Investigative Report by approval and signature.
REPORT VALIDATION AND ACCEPTANCE
OMIG may contact MCOs seeking clarification or additional information about the report after the
MCO’s submission. MCOs are required to submit corrected reports and/or attachments within 10
business days of OMIG’s request.
REQUIRED FIELDS
All relevant fields should be completed. For example, all identifying ID numbers for the provider
should be included and in the correct columns. While certain provider types may not have a particular
type of ID, all known ID numbers should be included on the report. All amount fields should also be
completed, if relevant. If there was no Medicaid-related settlement agreement for a case, then that
4
field is not required. Information about any educational activities should also be included on the
report.
For reviews of an individual provider, the required fields for all submissions that must be completed
are:
1. MCO Case ID
2. Line of Business
3. Provider Name
4. Provider Type
5. NPI
6. Action Type
7. SIU vs. Non-SIU
8. Allegation Category
9. Allegation
10. Scope Period Dates
11. Scope Period Type
12. Date Identified
13. Completed Date
14. Fraud, Waste, or Abuse
15. Reviewed Amount
16. Identified Amount (include only for the month the unique case was completed)
For reviews of multiple providers included in one larger project, the required fields that must be
completed for all submissions are:
1. MCO Case ID
2. Line of Business
3. Provider Name (identify the type of project)
4. Action Type
5. SIU vs. Non-SIU
6. Allegation Category
7. Allegation
8. Scope Period Dates
9. Scope Period Type
10. Date Identified
11. Completed Date
12. Fraud Waste or Abuse
13. Reviewed Amount
14. Identified Amount (include only for the month the unique case was completed)
DEFINITIONS AND GUIDANCE ON FIELDS
Action Type – The post-payment action undertaken by the MCO. This may consist of an audit,
investigation, educational, or re-educational activity conducted by the MCO. If the MCO identifies the
Action Type as “Other,” the MCO is required to provide a detailed explanation in the report’s
“Comments” section for the unique case. The action type “CAF Payment Suspension” refers to OMIG
requests for either a withhold or suspension of payments to participating providers where OMIG has
determined the provider is the subject of a pending investigation of a credible allegation of fraud
(CAF). “Education” or “Re-Education” refers to any educational activity, regardless of whether it is
5
related to a Corrective Action Plan (CAP). The Action Type “Self-Disclosure” should be used to report
network provider self-disclosures made directly to the MCO.
Allegation – The narrative explanation must describe the allegation pertaining to the unique case or
the cause of the overpayment or educational activity. This should be a description that will be
informative as to the subject matter of the post-payment review (e.g., inappropriate billing is not
sufficient).
Allegation Category – This field is used to quantify the type of provider activity that is under review.
If none of the options listed are appropriate, please select “Other.” When using “Other,” please add an
explanation in the Comments field.
Cash Amount (In Period) – The total amount of cash recovered from the provider in the reporting
period for the unique case. This may include a check, Electronic Funds Transfers, or other forms of
direct payments made by the provider to the MCO.
Cash Amount (Total) – The total (cumulative) amount of cash the MCO recovered from the provider
to date (from the completion of the review through the current reporting period), for the unique case.
Comments – Includes any narrative by the MCO to offer additional details related to the unique case
(e.g., an explanation about an “Other” Action Type or Allegation Category, or why the MCO is unable
to collect from the provider).
Completed Date – The date the MCO’s review, investigation, audit, or educational activity was
completed. This should be a date during the initial reporting period the MCO case appears. This is not
the date the MCO finishes collecting the related overpayment.
Federal Employment Identification Number (FEIN) – The federal tax identification number
assigned to a participating or non-participating provider.
Finalized Date – The date the MCO collected the entirety of the Medicaid overpayment for the
review, investigation, or audit, and no further action or activity will occur.
Fraud, Waste, or Abuse – MCOs must indicate whether the recovered overpayment or educational
activity was related to fraud, waste, or abuse, for the unique case.
Identified Amount – The total overpayment amount identified by the MCO from the audit, review, or
investigation of the unique case. This amount should only be reported for the month the unique case
was completed.
Initiated Date – The date the MCO’s review, investigation, audit, or educational activity began.
Effectively, the date the case was opened.
License # – The six-digit New York license number issued for a provider.
Line of Business – This field denotes which of the MCO’s lines of business the provider’s claims
review or educational activity related to—Mainstream, HARP, or HIV/Special Needs Plan.
MCO Case ID – The MCO is required to provide case-level detail about the recovery or educational
activity. This field is the unique case identifier for each audit, review, or investigation performed by the
6
MCO of a participating or non-participating provider that resulted in a post-payment recovery,
Medicaid-related settlement agreement, or educational activity.
MMIS # – The eight-digit NYS Medicaid Management Information System identification number
assigned to a provider, if applicable.
National Provider Identifier (NPI) – The unique identification number for covered health care
providers for use in the administrative and financial transactions adopted under the Health Insurance
Portability and Accountability Act of 1996 (HIPAA). The NPI is a 10-digit, intelligence-free numeric
identifier.
Offset Amount (In Period) – The total amount of offset claims resulting from an MCO’s post-
payment audit, review, or investigation, in the reporting period, for the unique case.
Offset Amount (Total) – The total (cumulative) amount of offset claims to date resulting from an
MCO’s post-payment audit, review, or investigation, for the unique case (from the completion of the
review through the current reporting period).
Provider Name – The name of the participating or non-participating provider associated with the
MCO Case ID.
Provider Type – The enrollment category or category of service of the provider under review (e.g.,
Dentist).
Recovered Amount (In Period) – The total aggregate amount recovered by the MCO from the
provider in the reporting period, for the unique case, including Cash, Offsets, and Voids.
Recovered Amount (Total) – The total (cumulative) amount recovered by the MCO from the
provider to date since first reported, for the unique case, including Cash, Offsets, and Voids.
Refund Amount (In Period) – The total amount returned or refunded to the provider due to an
overpayment to the MCO, in the reporting period, for the unique case.
Refund Amount (Total) – The total (cumulative) amount returned or refunded to the provider by the
MCO to date since first reported, for the unique case.
Reviewed Amount – The total dollars of claims reviewed by the MCO as part of the review
regardless of whether any claims were later determined to be inappropriate.
Scope Period Start – The start date of the review, audit, investigation, or educational activity
reviewed by the MCO, for the unique case.
Scope Period End – The end date of the review, audit, investigation, or educational activity reviewed
by the MCO, for the unique case.
Scope Period Type – The type of provider activity the MCO reviewed. This may include the date the
service was performed by the provider (Date of Service), the date the provider received a payment
from the MCO related to the claim for the service performed (Date of Payment), or both conditions
(Both).
7
Settlement Amount – At the conclusion of the MCO’s audit, review, or investigation, if a Medicaid-
related settlement agreement is reached, the settlement amount is the agreed-upon amount between
the MCO and the provider, related to the unique case. The MCO is required to provide copies of the
corresponding settlement agreements for all such cases indicated in the report.
SIU vs. Non-SIU – Indicates who conducted the post-payment audit, investigation, or educational
activity. There are three options—the activity was conducted by the MCO’s SIU, a unit outside the
MCO’s SIU, or the MCO’s vendor.
“Subcontractor” – An individual or entity that has a contract with the MCO that relates directly or
indirectly to the performance of the MCO’s obligations under its contract.
Voided Amount (In Period) – The total amount of voided claims resulting from an MCO’s post-
payment audit, review, or investigation, in the reporting period, for the unique case.
Voided Amount (Total) – The total (cumulative) amount of voided claims to date resulting from an
MCO’s post-payment audit, review, or investigation, for the unique case (from the completion of the
review through the current reporting period).
ADDITIONAL INFORMATION ON FIELDS
Amount Fields
The amounts reported should only include Medicaid funds that were identified or recovered.
Action Type
There has been some confusion regarding whether to select “Audit” or “Investigation” when
completing the Action Type. To some extent this is a judgement call, however, an Investigation is
typically a result of some sort of referral and references a deeper dive into a strong suspicion of
wrongdoing on the part of the provider. An audit is a systemic/regular review that may be conducted
in a key problem area(s) of concern. If the MCO is conducting an educational activity, the MCO
should select “Education” or “Re-Education” as the Action Type. Please include any additional
information in the Comments column, if applicable. The Action Type “Self-Disclosure” should be used
to report network provider self-disclosures made directly to the MCO.
Even if an MCO does not recover Medicaid funds after a review, audit, or investigation, the MCO
should include any educational and re-educational activity undertaken on the Provider Investigative
Report.
Cases to Report
The Provider Investigative Report is intended to capture the results of the MCO’s audits or
investigations. Closed cases can result in a recovery or the provider will be educated after a Medicaid
review, audit, or investigation. The case should be initially reported in the month the review was
completed. For cases that involve a recovery, the case must be reported on any subsequent reports
until the entire balance of the recovery has been received or the educational activity has been
completed. Within each reporting period, the MCO should update the “In Period” totals, where
8
applicable, with the funds that were recovered from the provider during that reporting period as well
as the “Total” fields with the amount of the cumulative receipts for that case.
As required by federal law, section 22.7(e) of the Model Contract (effective March 1, 2019), and 18
NYCRR § 521-2.4(f), the MCO must have policies and procedures for providers to report, return, and
explain overpayments to the MCO. Any monies recovered as a result of such a report by a provider to
the MCO must also be reported on the Provider Investigative Report.
Non-SIU Cases
When the MCO is reviewing multiple providers for minor improper payments, the MCO may report
this as a single project on one line of the report with the total recoveries or educational activities listed
for that project. For example, if the MCO conducted a review of their entire network of providers or a
particular provider type for improper use of a modifier, that review can be reported as one project.
This would not be the case when the MCO conducted a focused review of a specific provider. Please
see the “Required Fields” section to view which fields are required for this scenario.
Recovered Amounts
If the MCO selects “CAF Payment Suspension” as the Action Type, then amounts withheld (both in
period and total) should be entered in the “Recovered Amount (In Period)” and “Recovered Amount
(Total)” fields.
Settlement Agreements
If the MCO executed a Medicaid-related settlement agreement with the provider, the settlement
agreement should only be uploaded for the initial reporting period. This is the case even if the
payments carry over multiple reporting periods. Please do not upload a settlement agreement more
than once. The settlement agreement must be reported and submitted during the period the
agreement is signed. If the settlement agreement is submitted during a reporting period more than a
month after the agreement is signed, it will be considered not timely submitted.
Vendor/Subcontractor Activities
Any recovery or educational activities conducted by an MCO’s vendor or subcontractor should also
be included for the relevant reporting period.
ADDITIONAL INFORMATION
Inability to Collect from Provider
If the MCO is unable to collect the recoveries from a provider for a reported case, the MCO will need
to identify the reason for the difficulty in the "Comments” column (e.g., the provider has filed for
bankruptcy or left the state). Once the MCO has reported that they are unable to collect the
recoveries and the reason why, the case will no longer need to appear on the Provider Investigative
Report, even if the recovery has not been completed. In the future, if the MCO can initiate recovery
efforts related to that specific case, that case should be included again on the appropriate report(s)
until such time as the recovery has been completed.

9
Nothing to Report
If there were no cases closed, no ongoing collection activity, or no educational activity during the
reporting period, the report should still be filed with the Data Control information filled in and a note in
the first “Comments” field of the report stating there is no activity to report in this period.
OMIG Withholds
If a case was created to withhold funds on an OMIG-initiated case during the reporting period, but
there were no withholds during that month, the MCO should include the case in the report with a $0
amount and a note in the “Comments” column outlining this situation.
Downloading the Reporting Software (UDCS)
MCOs must download the Universal Data Collection Software (UDCS) and the Provider Investigative
Report from the Heath Commerce System’s Healthcare Financial Data Gateway application.
Users that do not already have access to the Healthcare Financial Data Gateway application must
request access on the application’s landing page, as shown below:
To download the UDCS, select the “Software” tab, located on the Healthcare Financial Data Gateway
toolbar. Next, download the software by clicking the “Software” button.

10
After clicking the “Software” button, the option for the “Report Manager and Shell” will appear with the
option to download.

11
Download the software by saving the file to your computer. The file is a zip file, which includes a
“UDCS Installation Guide” with additional information.

12
Downloading the Provider Investigative Report Template
To download the Provider Investigative Report, users must follow similar steps taken to download the
UCDS software, as noted above. First, click the “Software” tab on the Healthcare Financial Data
Gateway page. This time, select “Reports.”
A Matrix Reports screen will appear, where the relevant Submission Period must be selected. Select
“OMIG Managed Care Organizations” as the Organization Type.
Select “Monthly” under Submission Schedule.

13
Next, select the applicable Submission Year and Submission Period, depending on the reporting
period, then select Search.
Download the report template to the computer.
Open the report template using the recently downloaded UDCS software.

14
Completing the Report
ADDING DOWNLOADED REPORT TO UDCS
Once the Report File has been downloaded to your computer, open the saved UDCS software. Select
“Add Downloaded Reports.”
A browser window will open. Locate the report saved on your computer. Select the appropriate report.
Next, select “Open.”

15
CREATING A NEW REPORT
After downloading the report file to the software, open the report by clicking “Select A Report” from
the UDCS’s drop-down menu. Select “Monthly Provider Investigative Report.” Next, click the “Open
Selected Report” button.

16
For new reports, select “Start New Report” in the pop-up window. To resume editing an existing
report, select “Open Existing Report.”
Select the correct MCO name from the “Organization” drop-down menu. Next, select “Statewide” from
the “Region” drop-down menu. Click “Ok.” A blank report will open to begin a new report.

17
COMPLETING RESPONSIBLE PARTY INFORMATION
Each report must include a completed “Data Control Form,” which must note the person who
completed the form, as well as the MCO’s Chief Executive Officer and Chief Financial Officer. The
following pop-up window for the Control Data Form appears after starting a new report. The Control
Data Form requires identifying/contact information for each of these individuals.
Users who prefer to complete this information after starting the report can return to the Control Data
Form by selecting the appropriate icon on the report’s main toolbar:
Upon completion of the Control Data Form, return to the main report by clicking “Save” at the bottom
of the form. To ensure all required fields are completed, click the “Validate” button, which will indicate
if any information is missing.
COMPLETING THE REPORT
Each report contains columns with the fields listed in the “Definitions and Guidance on Fields”
section.

18
Please note the MCO Case ID number and all provider identification numbers should be
entered as numbers only—hyphens, slashes, N/As, and spaces should not be entered in these
fields.
Some of the identification fields are hard-coded, which means the information must be a certain
length. If the number entered is shorter than the required length, an error message will pop up.

19
The following columns contain a fixed number of digits:
FEIN 9 digits
NY License # 6 digits
MMIS 8 digits
NPI 10 digits
There are seven columns that have pre-set options for completion (Line of Business, Provider Type,
Action Type, SIU vs. Non-SIU, Allegation Category, Scope Period Type, and Fraud, Waste, or
Abuse). These fields utilize a List Box function. To select the appropriate response, double-click in the
empty field below the column title. A box will pop up with the options for that field’s completion.
REPORT FUNCTIONALITY
The Provider Investigative Report has some Excel-like functions, including “Wrap Text,” adjustable
column width, and a default date format.
PROVIDER INVESTIGATIVE REPORT TOOLS
Two icons located on the top toolbar allow for exporting the report as either a PDF or an Excel file.

20
There is also the ability to add and save notes to the report using the “Notepad” feature.
Notes can also be opened by clicking “Notes” on the top toolbar.
21
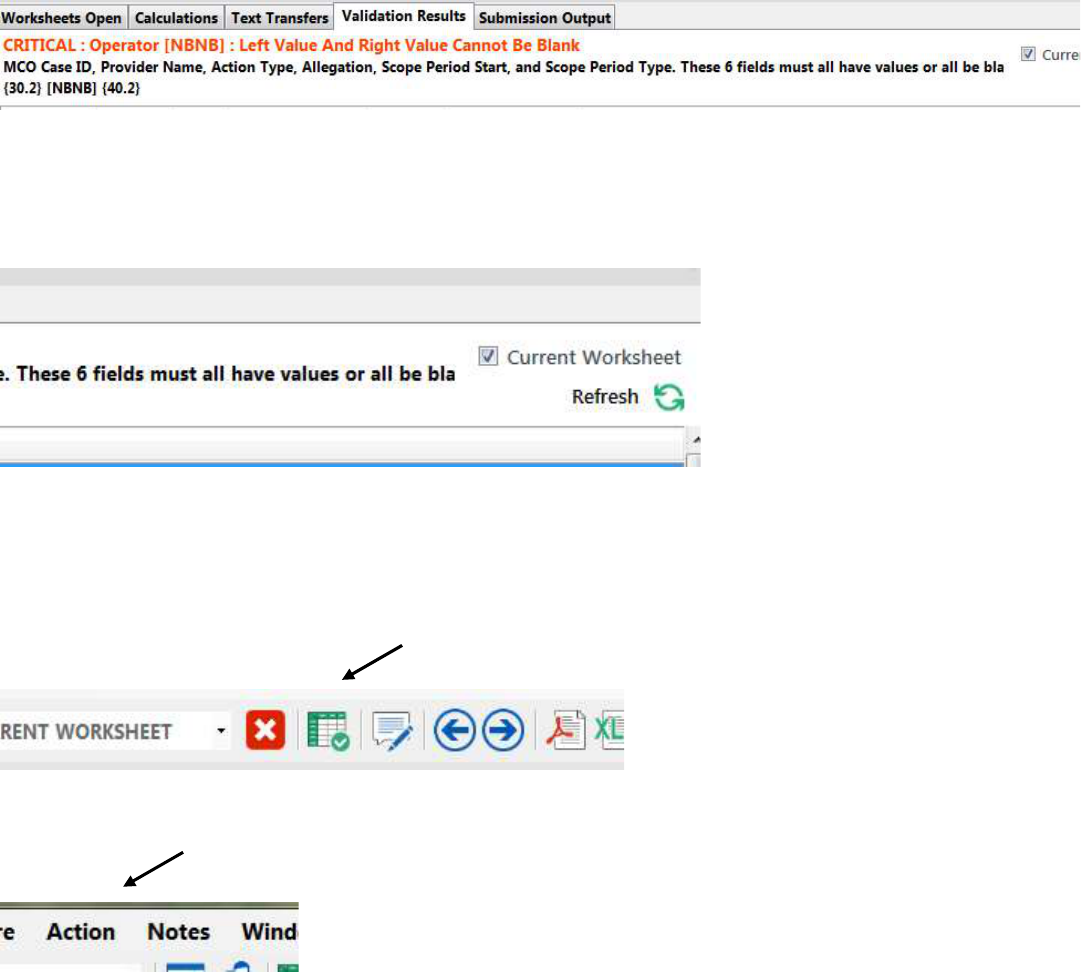
VALIDATION ERRORS/FINALIZING THE REPORT
There are certain required fields for completion of the Provider Investigative Report. Once all the
information is entered into the report, check the Validation Results at the bottom of the report in
UDCS. If there are any errors, the program will not allow the report to be finalized.
As errors are corrected, click “Refresh” to remove them from the list of Validation Results.
Once all errors are corrected and the report is complete, finalize the report to upload the results to the
Healthcare Financial Data Gateway. Two options are available to finalize the report. The first is a
symbol of a table on the icon toolbar, as shown below:
The second option to finalize the report is to select the “Action” tab on the top toolbar, where one of
the options is to “Finalize the Report.”
Once “Finalize the Report” has been selected, a pop-up window will appear to allow users to browse
for the location the completed report will be saved. Once a file location has been designated, another
pop-up window will notify users the file has been saved and the report is closed.

22
CORRECTING REPORT ERRORS
If there is an error(s) in the Provider Investigative Report, OMIG will contact the MCO and request the
report be corrected within 10 business days. Errors may include the CFO not certifying the report,
required fields not being completed, or information being added to the wrong column in the report. If
the MCO does not correct the error(s) within 10 business days of OMIG returning the report, the MCO
will have one more opportunity to correct the problem. If the MCO fails to correct the issue after the
second notification, the errors will remain part of the official Provider Investigative Report for that
month.
HELP COMPLETING THE PROVIDER INVESTIGATIVE REPORT
Any questions regarding the completion of the Provider Investigative Report should be addressed to
the mailbox [email protected]. Please include “ProvIR Question” in the subject line of the
email.
Additionally, a “Help” function is available in the UDCS that outlines the functionality of the UDCS
itself (it is not specific to the Provider Investigative Report).
Uploading the Completed Report to HCS
Once the report has been completed and finalized, use the “Submission” tab in the Healthcare
Financial Data Gateway to submit the Provider Investigative Report and any Medicaid-related
settlement agreements, if applicable. Select “MPIR” as the Submission Type and the correct MCO
from the Organization drop-down menu. Click the Search button and the “Choose File” option will
appear. (There are two types of submissions on this page: MPIR, which is the report; and
SETTLMNT, which is any Medicaid-related settlement agreements.)
Next, use the “Browse” button at the end of the “Upload File” box to select the relevant file(s)
(Provider Investigative Report or Settlement Agreements). After selecting the file(s), click the “Submit”
button to upload the file(s) to the Gateway.

23
Once the Provider Investigative Report is successfully submitted, the CFO will then be able to certify
the report. If, after reviewing the report in the Gateway, the CFO would like changes made to the
report prior to certification, the Submitter may make changes to the report in the UDCS and then
upload a new copy of the report to the Gateway.
*Note – If an individual needs to be included on the PIR monthly email distribution list, please send
the individual’s name and email address to OMIG through mmcreporting@omig.ny.gov. If an
individual needs to be added to the Healthcare Financial Data Gateway in the User Role of Submitter
or CFO, please send the individual’s name, Gateway User ID, and User Role to OMIG using the
same email address as above.
Reminder
Under Medicaid Managed Care Model Contract section 18.5(a)(vii), any potential fraud, waste, or
abuse must be referred to OMIG, through the Fraud, Waste, and Abuse Referral process, within 10
business days of identifying the potential fraud, waste, or abuse. Additional information can be found
at https://omig.ny.gov/information-resources/medicaid-managed-care-fraud-waste-and-abuse-
prevention-programs-guidance-and
