
Division of Health Policy
November 17, 2022
Rural Health Care in Minnesota: Data Highlights

Section Slide
State of Rural Minnesota
What are the demographic characteristics of rural Minnesota?
6
Structure of Rural Health System: An Overview
How do people in rural areas access health care? Where are health care facilities in the state?
11
Rural Health Care Workforce
What is the composition, demographics and geographic distribution of the state’s licensed health care workforce?
19
Availability of Health Care Services in Rural Minnesota
What health care services are available to people living in rural Minnesota, and has it changed over time?
27
Health Care Use in Rural Minnesota
What is the health status of people in rural Minnesota? What are the barriers they face to receiving health services,
and what are their health outcomes?
33
Financing
What level of competition do we see among rural health care providers? Do we pay more for health care different in
rural areas? How are providers doing financially?
45
Table of contents

• A summary of all data sources and notes are available on the MN Rural Health Care Chartbook webpage
(https://www.health.state.mn.us/facilities/ruralhealth/docs/summaries/index.html)
• There are a number of ways to report on rurality and geography. This chartbook uses the following constructs (defined in subsequent
slides). The use of a particular construct is informed by the availability of the data.
• Rural-Urban Commuting Area codes (RUCA codes)
• Based on zip code, census tract, or county, as noted in each slide
• State Community Health Services Advisory Committee (SCHSAC) regions
• When possible, the most up-to-date data are used. Therefore, the data year(s) presented may vary across the chart book.
• View the MN Rural Health Care Chartbook webpage (https://www.health.state.mn.us/facilities/ruralhealth/docs/summaries/index.html)
to access the alternative text for this chartbook.
• Direct links are listed on each slide.
Technical notes

Source: MDH. RUCAs were developed by the U.S. Department of Agriculture, Economic Research Service, and the
University of Washington’s WWAMI Rural Health Research Center. This map is based on census tract.
Summary of Slide
• Rural-Urban Commuting Areas or RUCAs are one of many
ways to measure rurality.
• RUCAs take into account population density, urbanization
and daily commuting patterns to identify urban and rural
regions of the state.
• Current definitions are based on 2010 census data. More
areas of the state became urban between the 2000 and
2010 census.
• For slides with two categories, unless otherwise noted:
• urban = metropolitan
• rural = large town + small town rural + isolated rural
• RUCA codes are based on zip code unless otherwise noted
each slide.
4
Defining rural: Rural-Urban Commuting Area
(RUCA) Codes

What are the demographic characteristics of rural Minnesota?
State of Rural Minnesota

• Minnesota is projected to gain nearly 900,000 residents between 2018 and 2053.
• The seven-county metro region is projected to gain about 924,000 residents, while Greater
Minnesota will shrink by approximately 27,000 residents during this time.
• Top 5 counties with the largest decline in population by 2053 will be Saint Louis (-28,238), Winona
(-8,960), McLeod (-8,425), Freeborn (-7,078), and Martin (-6,541).
• Minnesota’s oldest residents, aged 85 and above, are expected to more than double in the
next 35 years—from the current 120,000 to over 270,000.
• Population growth in the state will be driven by communities of color.
Source: Minnesota Demographer’s Office, “Long-term Population Projections for Minnesota” October 2020”.
7
Key points – Minnesota rural demographics

Source: Image is from Minnesota State Demographic Center, October 2020, Report: Long-Term Population Projections for Minnesota page 17. Data is from https://mn.gov/admin/demography/data-by-
topic/population-data/our-projections/ (vintage February 2021).
Summary of Slide
• Within the next decade, the
total number of older
adults (65+) is anticipated
to outnumber children in
Minnesota age 0 to 14.
• In 2033, 32% of residents
of rural Minnesota counties
are projected to be 65 years
of age or older vs. 19% for
urban counties.
8
The population of Minnesota is aging

Source: MDH/Health Economics Program analysis of the American Community Survey Five-Year Estimate 2015 to 2019.
RUCA based on census tract
Summary of Slide
9
People living in rural Minnesota are more likely to have household
incomes below the statewide median income
25.0%
65.3%
80.6%
89.9%
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Urban Large Rural City Small Town
Rural
Isolated Rural
More than three out of four people living in
rural areas have household incomes below
the statewide median income

Note: The percentages are not statistically different by geographic category.
Source: MDH/Health Economics Program analysis of the American Community Survey Five-Year Estimate 2015 to 2019. RUCA
based on census tract
Summary of Slide
‘Concentrated poverty’ is
defined here as having more
than one in five residents
living in poverty at the census
tract level.
There are an estimated 122,000
people living in concentrated
poverty areas in rural Minnesota.
10
Areas of concentrated poverty occur in both
rural and urban areas of the state
9.1%
11.7%
11.6%
10.5%
0.0% 2.0% 4.0% 6.0% 8.0% 10.0% 12.0% 14.0%
Urban
Large Rural City
Small Town Rural
Isolated Rural
Percent of Population Below Poverty

How do people in rural areas access health care? Where are health care facilities in the state?
Structure of Rural Health System: An Overview

• Rural residents are more likely to get health care through public sources, such as
Medicare, Medicaid and MinnesotaCare.
• While health care facilities are distributed throughout the state, they are more spread
out in rural areas.
12
Key points – Access to health care

Source: Minnesota Health Access Survey, 2021; Geographies based on RUCA zip-code approximations.
*Indicates significant difference from Metropolitan at the 95% level.
Summary of Slide
Reasons for higher rates of public health
insurance among rural Minnesotans:
1. Age: people over 65 are more likely to have
Medicare;
2. Lower Incomes: more likely to be eligible for
state public programs; and
3. Less access to employer coverage: fewer
people are connected to an employer that
offers coverage.
13
Rural Minnesotans are more likely to have public health insurance
coverage, such as Medicare, Medicaid or MinnesotaCare

1
Source: MDH Health Economics Program analysis of 2021 hospital annual reports, October 2022.
2
There are 77 Critical Access Hospitals in Minnesota; however, one is an Indian Health Services Hospital. This is not included in the count
of community hospitals, which are limited to non-federal short-term general and other special hospitals, and are accessible by the
general public. https://www.health.state.mn.us/facilities/ruralhealth/flex/mnhospitals.html
3
Outpatient clinics are designated by the hospital and may not be co-located with the hospital, but are billed to Medicare under the
hospital’s provider identification number.
4
Source: Minnesota Department of Health, Health Economics Program analysis of 2022 Directory of Registered, Licensed and/or Certified
Health Care Facilities and Service, Table 11. https://www.health.state.mn.us/facilities/regulation/directory/docs/2022mdhdirectory.pdf
.
Summary of Slide
• Of the 127 community hospitals in Minnesota,
76 are designated Critical Access Hospitals.
1,2
• In total, 90 hospitals are located in rural areas.
1
• Around one-third of all hospital outpatient
clinics in the state, 138 of 408 total clinics, are
in rural areas.
1,3
• All but one county, Red Lake, has at least one
nursing home as of 2022.
4
14
Hospital and nursing home services are
available throughout the state

Map Notes: Dots represent the number of clinics, and do not account for patient population or number of practicing physicians. Locations are plotted by zip code and may not be exact. Primary Care includes
general family medicine, general internal medicine, and general pediatrics; Specialty Care includes one or more non-primary care specialty. 74.3% of the population lives in urban areas, and 25.7% of the
population lives in rural areas based on 2019 5-year population estimates and census tract RUCA codes.
1
Source: MDH Health Economics Program analysis of the Minnesota Statewide Quality Reporting and Measurement System 2022 Physician Clinic Registry; also source for maps.
2
Source: https://www.mnachc.org/what-is-a-community-health-center
Summary of Slide
• 37% (240) of all primary care
clinics (642) are located in
rural areas.
1
• 20% (196) of all specialty
care clinics (957) are located
in rural areas.
1
• Minnesota's 17 Community
Health Centers care for
nearly 200,000 low-income
people.
2
15
Primary and specialty clinics are available throughout Minnesota

Person-centered, coordinated primary care
available to most Minnesotans
16
• MDH certifies primary care clinics and
clinicians as health care homes, known
nationally as a patient centered medical
home.
• The health care home clinic team
coordinates care with the patient and
their family to ensure whole person
care and to improve health and well-
being.
• 79% of MN counties have at least one
health care home clinic.

Source: https://mn.gov/emsrb/assets/Analysis%20and%20Trends%20of%20the%20Minnesota%20EMS%20Workforce_tcm1116-526101.pdf
Summary of Slide
• Minnesota's mirrors in the nation
in seeing decreases in the EMS
workforce.
• There is an alarming gap between
the numbers of EMS certifications
issued vs. those expiring.
• In 2021, the state lost 2,916
certified EMS providers.
17
Rural Emergency Medical Services (EMS) workforce is in crisis!

Source: MDH Trauma System August 2022; MDH Stroke System June 2022
Summary of Slide
• Minnesota has 126 designated trauma hospitals across four adult and two
pediatric designation levels.
• 99% of Minnesotans live within 60 minutes of a trauma hospital.
• 76% of Minnesotans live within 60 minutes of a Level 1 or 2 trauma hospital.
• 72% of Minnesota children live within 60 minutes of a pediatric trauma
h
ospital.
• 92% of Minnesotans live within a 30-m
inute drive of a designated stroke
system hospital.
18
Access to critical trauma and stroke care is available throughout the state

What is the composition, demographics and geographic distribution of the state’s licensed health care workforce?
Rural Health Care Workforce

• Nurses make up the largest share of the state’s licensed providers and are the
foundation of the health care system.
• There is a maldistribution of providers in the state—the majority work in the urban
areas. Consequently, the more rural parts of the state face a severe shortage of all
provider types, especially in primary care and mental health.
• 80% of Minnesota counties qualify as mental health professional shortage areas.
• Rural providers are older and closer to retirement.
20
Key points – Health care workforce
Source: MDH Office of Rural Health and Primary Care analysis. Data provided by Health Licensing Boards, July 2022. Mental health providers include marriage and family therapists, social workers,
psychologists and counselors.
Summary of Slide
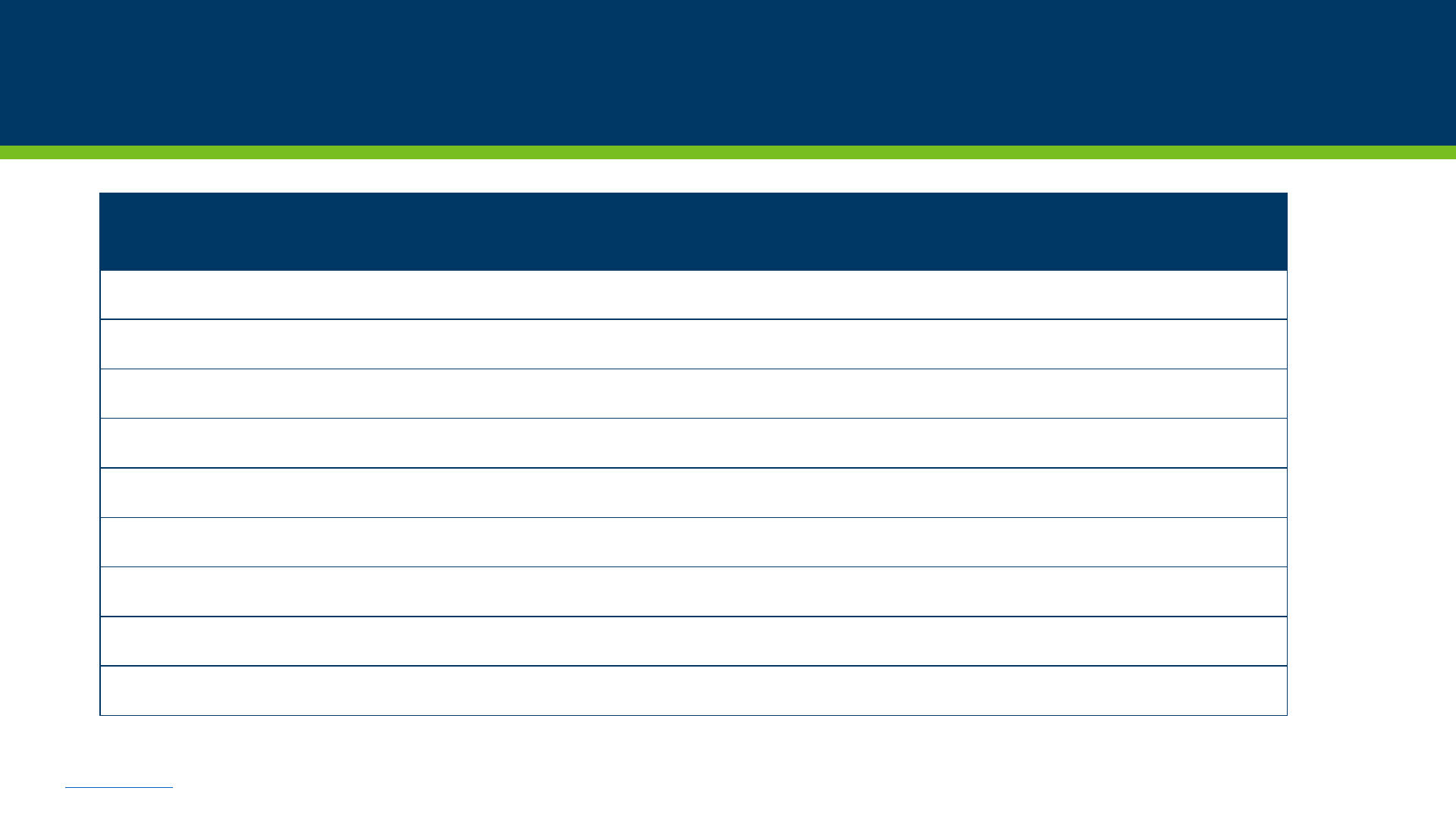
License Type Number of Providers
in Minnesota in 2021
Registered Nurses and Licensed Practical Nurses 130,484
Physicians 26,874
Mental Health Providers 25,758
Advanced Practice Nurses 10,946
Pharmacy Technicians 10,386
Pharmacists 9,584
Physical Therapy Professionals 8,035
Dentists 4,044
Physician Assistants 3,922
21
Registered nurses and licensed practical nurses make up the
majority of the health care workforce in Minnesota

Source: MDH Office of Rural Health and Primary Care analysis. Data provided by Health Licensing Boards, July 2022. Data includes: physicians, physician assistants, respiratory therapists, oral health
professions, pharmacy professions, physical therapy professions, and mental health professions.
Summary of Slide
4%
6%
10%
80%
8%
7%
11%
74%
Isolated Rural
Small Town Rural
Large Town
Metropolitan
Population Health Care Providers
Very few licensed health care
providers work in rural areas.
22
The majority of licensed health care providers
work in metropolitan areas

Source: MDH Office of Rural Health and Primary Care analysis. Data provided by the American Board of Medical Specialties and American Osteopathic Association. Counts by region are based on primary
practice address that physicians report to the Board of Medical Practice. July 2022.
Summary of Slide
49.4
43.9
13.1
20.3
8.8
6.6
59.9
21.6
10.0
9.6
6.1
8.1
87.0
13.6
5.6
2.3
2.6
10.0
36.1
1.8
0.5 0.5
0 1.1
Family Medicine Internal Medicine OB/GYN General Pediatrics General Psychiatry General Surgery
Number of Physicians per 100,000 people
Metropolitan
Large Town
Small Town Rural
Isolated Rural
OB/GYNs, Pediatricians, and Psychiatrists are in
short supply in rural parts of the state.
23
Rural areas face severe shortages of primary care physicians

Source: MDH Office of Rural Health and Primary Care analysis. Data provided by Health Licensing Boards, July 2022.
*Rural = isolated rural from Rural-Urban Commuting Area codes.
Summary of Slide
43.5
46
47
41
48
36
56
43
45 45
49
44
58
46
63
45
Advance Practice
Registered
Nurses
Dentists Licensed Pratical
Nurses
Pharmacists Physicians Physician
Assistants
Psychologists Registered
Nurses
Median Age of Health Care Providers
Urban Providers
Rural* Providers
24
Rural providers are older than their urban counterparts

One in three rural physicians plan to leave
the workforce within the next five years
Source: MDH Office of Rural Health and Primary Care, Physician Workforce Survey, (Oct 2021 – July 2022)
*Rural = isolated rural from Rural-Urban Commuting Area codes.
Summary of slide: https://www.health.state.mn.us/facilities/ruralhealth/docs/summaries/index.html
25
19%
18%
63%
33%
24%
43%
Plan to leave in 5 years or less Plan to leave within 6 - 10 years Plan to leave in more than 10 years
Urban Providers
Rural* Providers

What health care services are available to people living in rural Minnesota, and has it changed over time?
Availability of Health Care Services in Rural Minnesota

• The availability of services, especially in hospitals, has been changing over the past 10
years:
• Fewer services are available at rural hospitals, or the hospitals have closed.
• Non-metro counties have seen declines in obstetrics services and increases in
outpatient psychiatric services.
• More than half of the nursing home closures between 2012 and 2021 were in rural
counties.
28
Key points – Health care availability
Over the same
time period, rural
hospitals added
outpatient
psychiatric
services and
advanced
diagnostic
imaging services.
29
Rural hospitals saw declines in surgical services due to hospital
closures, consolidation, or service loss over the past decade
Source: MDH Health Economics Program analysis of hospital annual reports, October 2022; 2021 data is considered preliminary. Services are considered “available” when they are provided on site by
hospital staff, on site through contracted services, or off site through shared services agreement. No rural hospitals had open heart surgery or organ transplant services available in 2012 or 2021.
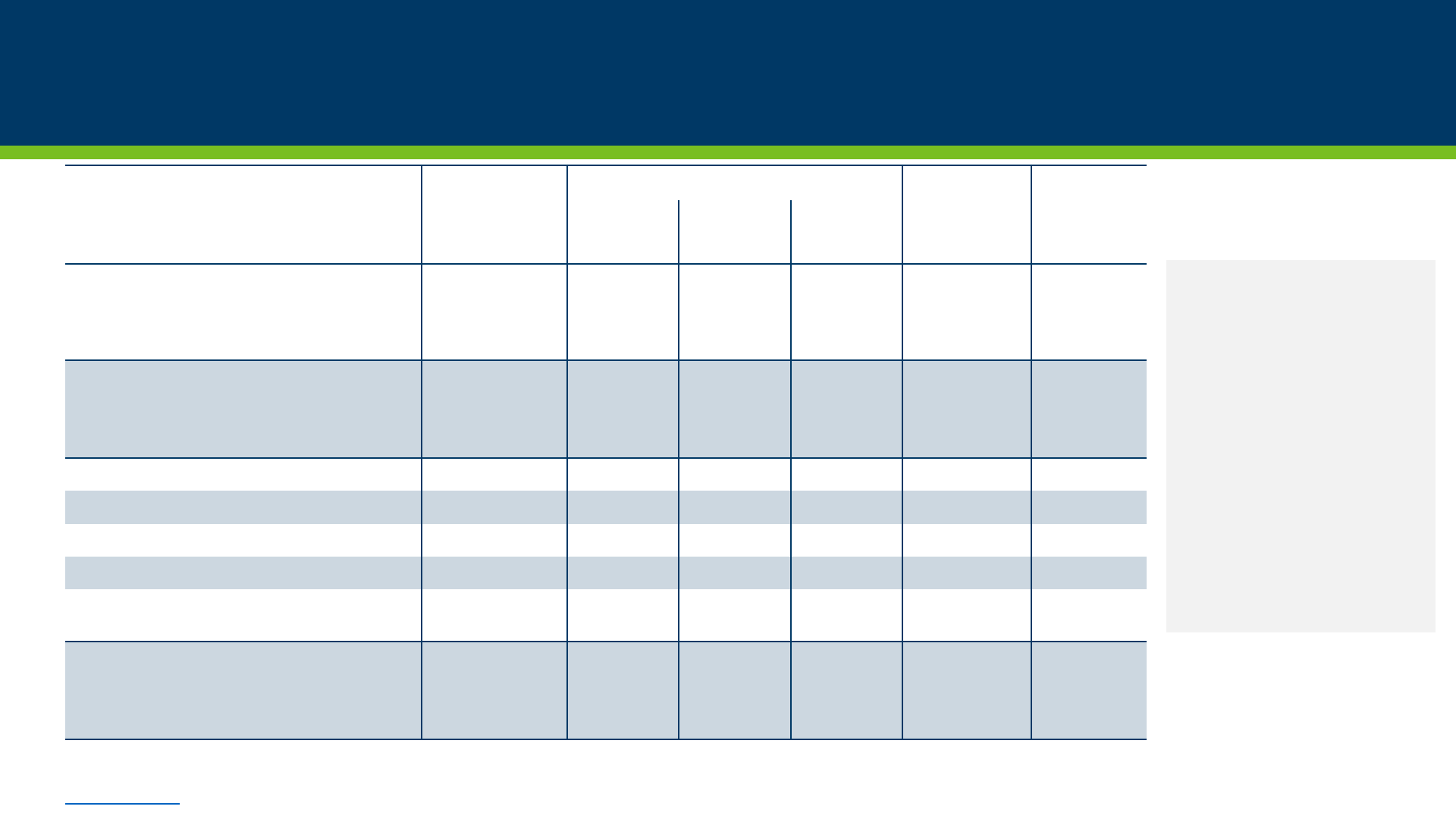
Summary of Slide
Hospitals with
service available
in 2012
Change in Service due to:
Hospitals with
service
available in
2021
Percent
Change 2012
to 2021
Closure or
Consolidation
Lost
Service
Added
Service
Surgery
Inpatient Surgery 86 2 6 1 79 -8.1%
Outpatient Surgery 91 2 1 1 89 -2.2%
Mental Health/Chemical Dependency Services
Outpatient Psychiatric 38 2 6 16 46 21.1%
Detoxification Services 9 1 4 5 9 0.0%
Diagnostic Radiology Services
Computer Tomography (CT) Scanning 92 2 0 0 90 -2.2%
Magnetic Resonance Imaging (MRI) 90 2 1 1 88 -2.2%
Positron Emission Tomography (PET) 3 0 2 2 3 0.0%
Single Photon Emission
Computerized Tomography (SPECT)
16 0 1 14 29 81.3%
Other Services
Renal Dialysis Services 14 0 3 2 13 -7.1%
Cardiac Catheterization Services 2 0 0 1 3 50.0%

Increases in pre-
term births have
been associated
with the loss of
hospital birth
services in rural
areas.
30
Nine Minnesota counties lost hospital birth services
between 2012 and 2021
Note: Due to a merger, the hospital in Mower County was no longer an independent licensed entity as of the end of 2014; however, birth services were offered at that site under the license of the
remaining corporate entity. The other hospital of the merger, in Freeborn County, no longer has birth services.
Sources: Minnesota Department of Health, Health Economics Program Analysis of hospital annual reports, October 2022; 2021 data is considered preliminary; U.S. Census Bureau (County Designations);
2022 closures: https://www.health.state.mn.us/about/org/hrd/hearing/index.html
Definition: Community hospitals were categorized as not offering birth services if they did not have at least one routine birth and had no licensed bassinets or stated that services were not available.
Summary of Slide

31
Other counties had changes in cardiac and
mental health beds over the past decade
Statewide,
between 2012 and
2021:
41 mental health
beds were lost.
49 cardiac beds
were lost.
Source: MDH Health Economics Program analysis of hospital annual reports, October 2022; 2021 data is considered preliminary.
Summary of Slide

• Rural counties
1
have about 30% of all nursing homes
but accounted for the majority of closed nursing
homes in the state between 2012 and 2021.
• In total, rural counties
1
lost 19 nursing homes, and
had a nearly 10% decline in nursing home beds.
• The nursing home population has been declining
since 1995, with alternative options for long-term
care, including home care and assisted living
becoming more common.
32
The relative decline in nursing homes and nursing home beds
was greater in rural Minnesota between 2012 and 2021
1
Rural counties are those that are either entirely rural, or a rural/town mix (49 counties), as defined by the Minnesota Population Center
in Greater Minnesota: Refined and Revisited (
https://mn.gov/admin/demography/reports-resources/greater-mn-refined-and-
revisited.jsp
), page 33.
Source: Minnesota Department of Health, Health Economics Program analysis of 2012 and 2021 nursing facility counts and capacity from
the Minnesota Department of Health, Health Regulation Division.
Summary of Slide

What is the health status of people in rural Minnesota?
What are the barriers they face to receiving health services, and what are their health outcomes?
Health Care Use in Rural Minnesota

• Rural and urban Minnesotans report similar health status, but rural Minnesotans experience
higher rates of suicide.
• Rural Minnesotans have to travel farther to receive inpatient health care services
– especially
mental health and obstetrics services.
• Rural Minnesotans are more likely to have problems getting appointments with primary care
providers when needed and finding dentists accepting new patients.
• Primary care providers work to fill “gaps” in care, especially in mental health, obstetrics, and
pediatric care.
• Rates of adolescent mental health screening are lower in rural areas, and there are higher rates
of opioid prescribing.
34
Key points – Health care access and use

• Most Minnesotans – 96.0% – use health insurance to help pay for health care services.
• Even with health insurance to help cover costs, many Minnesotans still face substantial
health care costs – 16.6% of Minnesotans struggle with medical bills, and 20.2% forgo
needed health care due to cost.
• Minnesotans in rural areas were less likely to have telephone or video visits with
providers in 2021.
35
How Minnesotans access health care services

1
Source: Minnesota Health Access Survey, 2021. Urban and Rural defined based on RUCA zip-code approximations. Difference was not statistically significant at the 95% level.
Differences in unhealthy days and chronic conditions were not statistically significant at the 95% level.
2
Source: Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death on CDC WONDER Online Database, released 2021.
Summary of Slide
• Minnesotans living in rural areas
reported frequent mental distress
at about the same rate (12.3%) as
those living in urban areas (12.7%).
1
• Age-adjusted suicide rate in greater
Minnesota (16.0) was higher than
the 7-county metro area (11.7) in
2020; this was primarily due to
higher firearm suicide rates in
greater Minnesota (7.9) compared
to the 7-county metro (4.6).
2
36
Rural and urban residents report about the
same number of unhealthy days

Source: MDH analysis of Minnesota hospital discharge inpatient records for medical-surgical care, obstetrics care, and mental health or chemical dependency care occurring in calendar years 2018-
2020. The analysis calculated the distance between the geographic centroid of each ZIP code to respective hospitals and excluded hospital stays that were transferred to another hospital to avoid
duplication. Patients with planned services, such as surgeries, may intentionally travel longer distances. Non-metropolitan ZIP codes are classified as ‘rural’ using RUCA.
Summary of Slide
• Rural patients seeking
inpatient mental health and
chemical dependency
treatment travel more than
three times longer than urban
patients.
• Patients receiving medical/
surgical care at Critical Access
Hospitals experience shorter
travel times than those
traveling to other types of
hospitals.
37
Minnesotans in Rural Areas have to travel longer to get
inpatient services – especially mental health services
82
28
27
25
17
21
81
43
69
37
23
35
Mental Health/Substance Abuse
Maternity/Neonatal Care
Other Medical-Surgical Care
Approximate Travel Time (Minutes)
Critical Access Hospitals Urban ZIP Codes Rural Zip Codes Statewide

Source: Minnesota Health Access Survey, 2021.
*Indicates significant difference from Urban at the 95% level.
Urban and Rural defined based on RUCA zip-code approximations.
Summary of Slide
38
Rural Minnesotans have fewer problems accessing providers
• 17% of rural
Minnesotans could not
see a provider as soon
as needed.
• Issues with providers
not being in network
were similar for urban
and rural Minnesotans.

Source: Minnesota Health Access Survey, 2021.
*Indicates significant difference from Urban at the 95% level.
Percentages for Type of Provider do not sum to 100 because respondents were able to select more than one type of provider. Urban and Rural defined based on RUCA zip-code approximations.
Summary of Slide
Among those who weren’t
able to get an appointment as
soon as needed: Rural
Minnesotans were more likely
to say they couldn’t get an
appointment with a
primary
care provider or a dentist
.
Rural Minnesotans also had
more problems finding
dentists that were accepting
new patients.
39
People in rural Minnesota had the most trouble getting primary
care appointments as soon as they were needed

Source: Minnesota Health Access Survey, 2021.
*Indicates significant difference from Urban at the 95% level.
Urban and Rural defined based on RUCA zip-code approximations.
Summary of Slide
40
Rural Minnesotans had lower telehealth use
• Rural Minnesotans had
lower utilization of
both phone and video
visits.
• Almost 20% of rural
Minnesotans lack
internet reliable
enough to use for a
video visit.

41
Most telehealth visits in the state were to primary care providers
• Mental health visits
made up a higher
percentage of video
visits than phone visits.
• Most people would do a
telehealth visit again.
• 78.5% for phone visits
• 80.8% for video visits
• This was similar for urban
and rural respondents.
Source: Minnesota Health Access Survey, 2021.
*Indicates significant difference from Urban at the 95% level.
1 Other providers include dentists, alternative medicine providers,
emergency rooms/urgent cares or COVID testing sites.
Percentages for Type of Provider do not sum to 100 because
respondents were able to select more than one type of provider.
Urban and Rural defined based on RUCA zip-code approximations.
Summary of Slide

Source: MDH-ORHPC Physician Workforce Survey, 2018.
* Rural = isolated rural from Rural-Urban Commuting Area codes.
** The most common “other” specialties listed include dermatology; emergency medicine; and orthopedics.
Summary of Slide
• Rural physicians often fill gaps in care when
there is a lack or absence in specialty
providers to serve rural populations.
• In areas of Obstetrics/Gynecology, Oral
Health, and Pediatrics, rural primary care
physicians are 15% more likely to provide
some level of care than urban primary care
physicians.
42
Rural primary care physicians are more likely to
fill gaps in care than their urban counterparts

1
Kessler, et al. “Lifetime Prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication.” Arch Gen Psychiatry, 2005 Jun; 62(6): 593-602.
Source: MDH Health Economics Program analysis of Adolescent Mental Health and/or Depression Screening data from the Minnesota Statewide Quality Reporting and Measurement System. Based on
adolescent patients aged 12-17 who had at least one telehealth or face-to-face well-child visit in a Minnesota clinic. White areas on the map had fewer than five patients for this measure.
US Preventive Services Task Force recommends mental health screening for all adolescents (see: Final Recommendation Statement: Depression in Children and Adolescents: Screening
(2016), U.S.
Preventive Services Task Force.
Summary of Slide
• Screening has increas ed over
time in both urban and rural
areas
• Rural adolescents are still
less likely to be screened
• Half of all mental health
conditions begin by age 14.
1
• Early treatment may lead to
better outcomes in the long
term.
Geography
2017
Screening
Rate
2020
Screening
Rate
Metropolitan
86% 92%
Small Rural Town
66% 86%
Isolated Rural
70% 85%
Statewide
83% 91%
43
Fewer adolescent patients in rural areas are screened for mental
health or depression problems, though rates are improving

Source: MDH Health Economics Program and Mathematica Policy Research “Patterns of Opioid Prescribing in Minnesota: 2012 and 2015,” April 2018.
https://www.health.state.mn.us/data/economics/docs/opioidbrief20185.pdf
Summary of Slide
64.6
74.0
77.8
77.8
57.0
64.5
71.2
70.4
-
20
40
60
80
Metropolitan Large Town Small Town Rural Isolated Rural
Opioid Prescriptions per 100 Covered Persons by RUCA
2012 2015
• Prescription opioid use has declined over
time – but is still higher in rural areas.
• Some counties in Northern Minnesota have
especially high rates of opioid prescriptions.
44
Prescription opioid use is higher in rural areas

What level of competition do we see among rural health care providers?
Do we pay more for health care different in rural areas? How are providers doing financially?
Financing

• More and more rural hospitals are affiliated with larger hospital and provider systems.
• CAH status is associated with higher net incomes for hospitals.
• Rural residents experience higher monthly cost sharing as compared to their urban
counterparts.
• Isolated rural hospitals provider higher levels of community benefit relative to
operating expenses.
• Community benefit in rural hospitals is more focused on keeping services available
than providing charity care.
46
Key points – Health care financing

Source: MDH/Health Economics Program calculation of Herfindahl-Hirschman competition (HHI) index based on net patient revenue from Hospital Annual Report Data, October 2022. 2021 data is
considered preliminary. Values in chart are subtracted from 2,500, or a highly concentrated market; positive values indicate a competitive market, negative values indicate a concentrated market.
For more information on this index, visit the US Department of Justice website at
www.justice.gov/atr/herfindahl-hirschman-index. SCHSAC Regions are defined on slide 5.
Summary of Slide
• Market
concentration can
lead to higher
prices.
• Three out of eight
regions had
moderately
concentrated
markets in 2021.
47
Many hospital markets in Minnesota are not competitive

Hospitals are classified based on RUCA zip code. Health care systems are ordered by total number of hospitals in descending order. Data
does not include urban hospitals. Locations are plotted by zip code and may not be exact.
Source: MDH Health Economics Program analysis of hospital annual reports, October 2022.
Summary of Slide
Hospitals that are part of
larger systems:
• May offer increased access
to specialty services only
available in urban areas.
• May increase financial
viability.
• Lead to consolidation of
services to fewer hospitals,
meaning some services
may be less available in
rural areas.
48
Over half of Minnesota’s rural hospitals were affiliated
with a larger provider group in 2021
Hospitals Available Beds
Sanford Health 15 409
Essentia Health 10 350
Mayo Clinic 7 244
CentraCare Health System 7 189
Avera Health 4 105
Catholic Health Initiatives 4 90
Allina Health System 3 109
HealthPartners, Inc./Park
Nicollet Health Services 3 77
M Health Fairview
2 114
Unaffiliated or Single Rural
Hospital in Hospital System
35 880
Total 90 2,567
▲
Critical Access Hospital
■
Non-Critical Access Hospital

*Preliminary data. Does not include urban hospitals.
Source: MDH Health Economics Program analysis of hospital annual reports, October 2022.
Summary of Slide
• All rural hospitals
saw an increase in
net income as
percent of revenue
in 2021, likely due
to COVID-19
funding.
• CAHs had higher
percentages of net
income than non-
CAHs.
49
Of rural hospitals, Critical Access Hospitals
have higher net income as a percent of revenue

Note: 2021 data is preliminary, numbers are based on charges for nursing homes reported by hospitals. Urban and Rural defined based on RUCA zip code designation.
Source: MDH Health Economics Program analysis of hospital annual reports, October 2022.
Summary of Slide
• Fewer urban hospitals
have attached nursing
homes.
• Having nursing home
services attached to
hospitals may lead to more
days at home for patients.
• However, it may cause
financial strain for
hospitals if nursing homes
are operating at low
capacity.
50
Rural areas have seen slight declines in nursing homes
attached to hospitals in the past 10 years

Monthly health care costs are higher in rural areas
for adults, lower for children
51
Per-member-per-month health care cost Statewide per-member-per-month health care cost
Source: MDH Health Economics Program analysis of All Payer Claims Database Public Use Files - Member (2018). Small town rural and isolated rural are combined. Monthly health care costs are based on total
dollars spent divided by number of months with enrollment across all types of coverage. For more information on the MNAPCD, or to get data: https://www.health.state.mn.us/data/apcd
.
Summary of Slide
$346
$331
$312
$0
$200
$400
$600
$800
$1,000
$1,200
Urban Large Rural City Small
Town/Isolated
Rural
Monthly Health Care Costs: 18 and Under
$771
$921
$872
$0
$200
$400
$600
$800
$1,000
$1,200
Urban Large Rural City Small
Town/Isolated
Rural
Monthly Health Care Costs: 19 to 64
$1,120
$1,075
$1,130
$0
$200
$400
$600
$800
$1,000
$1,200
Urban Large Rural City Small
Town/Isolated
Rural
Monthly Health Care Costs: 65 and older

$450
$480
$462
$1,140
$1,089
$1,060
$677
$661
$672
$0
$200
$400
$600
$800
$1,000
$1,200
Urban Large Rural City Small Town/Isolated
Rural
Urban Large Rural City Small Town/Isolated
Rural
Urban Large Rural City Small Town/Isolated
Rural
Commercial Medicare Minnesota Health Care Programs
Monthly Insurer Claims Cost
$72
$91
$97
$117
$131
$151
$3
$5
$6
$0
$40
$80
$120
$160
Monthly Member Cost
Sharing
Minnesotans in rural areas experience higher monthly cost sharing
regardless of health insurance coverage type
52
Source: MDH Health Economics Program analysis of All Payer Claims Database Public Use Files - Member (2018). Small town rural and isolated rural are combined. Monthly claims costs are based on payments
made by insurers for health care services received by members divided by number of months with enrollment in that type of coverage; monthly member cost sharing is based on cost sharing (deductible,
copayment or coinsurance) that was expected to be paid by member for health care services received divided by number of months with enrollment. For more information on the MNAPCD, or to get data:
https://www.health.state.mn.us/data/apcd
.
Summary of Slide
Higher cost sharing in
rural areas could be
related to:
• Provider network
differences.
• Health status
differences.
• Different health
plan options
available.

1
2021 data is preliminary.
2
Includes Medical Assistance and MinnesotaCare.
Percent shown is a percent of Hospital Patient revenue. Totals may not sum to 100% due to rounding.
Source: MDH Health Economics Program analysis of hospital annual reports, October 2022.
Summary of Slide
53
Rural hospitals rely more on Medicare revenue
than their urban counterparts
Critical Access Hospitals
Rural, Non Critical Access
Hospitals
Statewide Community
Hospitals
2012 2021
1
2012 2021
1
2012 2021
1
Medicare
42.6% 45.8% 33.9% 36.5% 30.6% 33.2%
State Public Programs
2
9.7% 11.4% 11.8% 11.7% 12.3% 13.6%
Private Insurance
41.7% 37.3% 48.7% 45.0% 51.4% 48.4%
Self-Pay
4.1% 2.7% 4.4% 3.3% 3.7% 2.4%
Other Payers
2.0% 2.8% 1.3% 3.5% 2.1% 2.5%
Hospital Patient Revenue, All
Payers
100% 100% 100% 100% 100% 100%

Source: MDH, Health Economics Program analysis of preliminary 2021 Hospital Annual Reports, October 2022, and MDH, Hospital
Community Benefit Spending in Minnesota, 2016 to 2019
Summary of Slide
• Non-profit hospitals provide community benefit as
part of their tax-exempt status.
• Community benefit spending can be categorized into
four broad categories:
• Direct patient care or unreimbursed services
• Research and education
• Financial and in-kind contributions
• Community activities
• Most community benefit is in the “direct patient
care” category.
54
Isolated rural hospitals devote a larger percentage of
operating expenses to community benefit

Source: MDH, Health Economics Program analysis of preliminary 2021 Hospital Annual Reports, October 2022.
Summary of Slide
• Isolated rural areas focus on
operating subsidized services –
such as keeping emergency
rooms open and staffed.
• State health care programs
underpayment – the difference
between the cost of care
provided to state program
patients and the actual payment
received – are greater in hospitals
located in metropolitan areas,
large towns, and small rural
towns.
55
Community benefit for direct patient care
is different across the state
Community Health
Services
Operating Subsidized
Services
State Health Care
Programs Underpayment
Charity Care

1
2021 data is preliminary.
Source: MDH, Health Economics Program analysis of Hospital Annual Reports, October 2022.
Summary of Slide
• The divide between rural and
urban hospitals has been
decreasing in the past 5
years, due to a decreasing
percentage of charity care at
urban hospitals.
• In 2021, the percentage of
uncompensated care that
was charity care decreased
for all hospital types.
• Bad debt is not considered
community benefit.
Bad Debt
(care provided,
payment
expected)
Charity Care
(care provided,
payment not
expected)
Uncompensated
Care
(Care provided but not
reimbursed)
56
Most uncompensated care in rural hospitals is bad debt

A summary of the charts and graphs contained within is provided at
https://www.health.state.mn.us/facilities/ruralhealth/docs/summaries/index.html
Direct links are listed on each page. If you need the information in a different format, please use the contact links above.
Health Economics Program
www.health.mn.state.us/healtheconomics
E-mail: health.hep@state.mn.us
Phone: 651-201-4520
Publications: heppublications.web.health.state.mn.us/
Health Care Markets Chartbook:
www.health.state.mn.us/data/economics/chartbook/
Office of Rural Health and Primary Care
www.health.state.mn.us/facilities/ruralhealth/
E-mail: health.orhpc@state.mn.us
Phone: 651-201-3838
Publications:
www.health.state.mn.us/data/workforce/reports.html
Appendix of Data Sources Available Here:
https://www.health.state.mn.us/facilities/ruralhealth/docs/summaries/index.html


