
SOUTH FLORIDA WATER MANAGEMENT DISTRICT
2024
EMPLOYEE
BENEFIT HIGHLIGHTS

South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
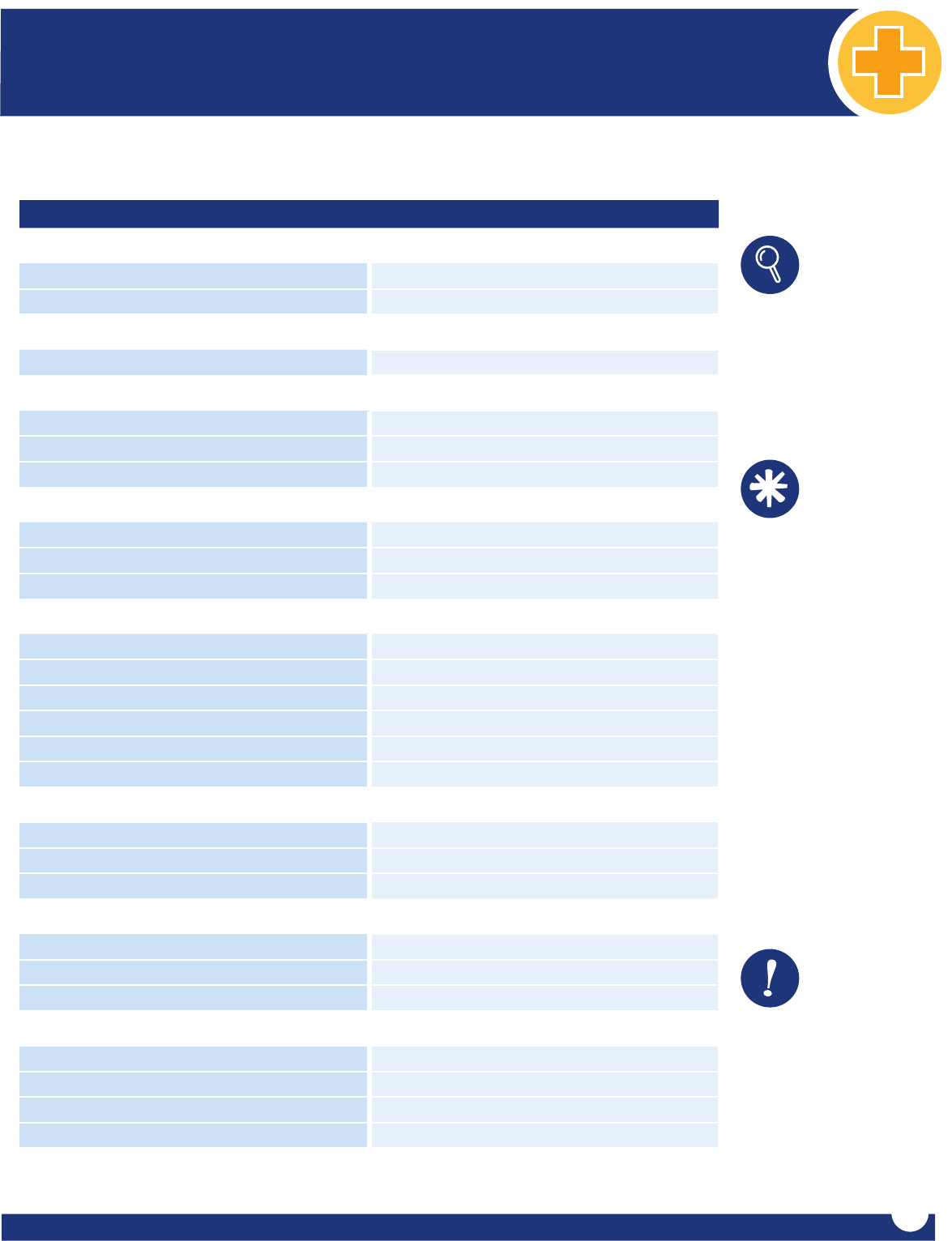
Contact Information
HR Benets Analysts SFWMD
Phone: (561) 686-8800
Email: HRBenetsT[email protected]
Online Benet Enrollment Bentek Support
Customer Service: (888) 5-Bentek (523-6835)
www.mybentek.com/sfwmd
Email: [email protected]
Wellness Cigna Healthcare
Onsite Cigna Well-Being Coordinator: Ratasha Iribarren
Phone: (561) 682-6086 l Cell: (954) 304-6865 | Email: riribarr@sfwmd.gov
Medical Insurance Cigna Healthcare
Customer Service: (800) 244-6224
www.mycigna.com
Onsite Cigna Representative: Sikander Khan
Phone: (561) 682-6052 | Email: [email protected]
Prescription Drug Coverage
& Mail-Order Program
Cigna/Express Scripts Pharmacy
Customer Service: (800) 835-3784
www.mycigna.com
Telehealth MDLIVE through Cigna
Customer Service: (888) 726-3171
www.mycigna.com
Dental Insurance Cigna Healthcare
Customer Service: (800) 244-6224
www.mycigna.com
Vision Insurance
Cigna Vision Care
Customer Service: (877) 478-7557
www.mycigna.com
Flexible Spending Accounts HealthEquity
Customer Service: (877) 924-3967
www.WageWorks.com
Employee Assistance Program Cigna
Customer Service: (877) 622-4327
Register On: www.mycigna.com
Basic Life and AD&D Insurance New York Life Group Benet Solutions
Customer Service (800) 362-4462
www.mynylgbs.com
Voluntary Life Insurance New York Life Group Benet Solutions
Customer Service (800) 362-4462
www.mynylgbs.com
Voluntary Short Term Disability New York Life Group Benet Solutions
Customer Service (800) 362-4462
www.mynylgbs.com
Long Term Disability New York Life Group Benet Solutions
Customer Service (800) 362-4462
www.mynylgbs.com
Supplemental Insurance and Discounts
Trustmark
New Enrollments - Customer Service: (888) 501-1280
Current Policy Holders - Customer Service: (800) 918-8877 | www.TrustmarkVB.com
Legal Club
Customer Service: (800) 305-6816
www.legalclub.com
Pet Benet Solutions
Customer Service: (800) 891-2565
www.petbenets.com/land/sfwmd
Retirement Plans
Florida Retirement System (FRS)
Customer Service: (844) 377-1888
www.myfrs.com
Fidelity Investments
Customer Service: (800) 343-0860
www.mydelitysite.com/SFWMD

South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Table of Contents
Introduction 1
Online Benet Enrollment 1
Group Insurance Eligibility 2-3
Qualifying Events and Section 125 4
Summary of Benets and Coverage 4
Ride the Wave to Wellness 5
Cigna Behavioral Programs 5
Medical Plan Resources 5-6
Medical Insurance 7-10
Cigna Network HMO Plan At-A-Glance 7
Cigna OAP In-Network Plan At-A-Glance 8
Dental Insurance 11-14
Cigna DHMO Plan At-A-Glance 12
Cigna DPPO Plan At-A-Glance 14
Vision Insurance 15-16
Cigna Vision Plans At-A-Glance 16
Flexible Spending Accounts 17-18
Employee Assistance Program 19
Basic Life and AD&D Insurance 19
Voluntary Life Insurance 20
Voluntary Short Term Disability 21
Long Term Disability 21
Supplemental Insurance and Discounts 22-23
Florida Retirement System 23
Voluntary Retirement Plan 24
Notes 24
This booklet is merely a summary of employee benets. For a full description, refer to the plan document. Where conict exists between this summary and the plan document, the plan document controls.
The South Florida Water Management District reserves the right to amend, modify or terminate the plan at any time. This booklet should not be construed as a guarantee of employment.

1
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Introduction
South Florida Water Management District provides a comprehensive
compensation package, which includes group insurance benets, wellness
programs and discounts. The Employee Benet Highlights Booklet provides a
general summary of the benet options as a convenient reference. Please refer
to The District’s Personnel Policies, applicable Contracts and/or Certicates of
Coverage for detailed descriptions of all available employee benet programs
and stipulations therein. If employee requires further explanation or needs
assistance regarding claims processing, please refer to the customer service
phone numbers under each benet description heading or contact the HR
Benets Team.
Whether you are new to the District or already a part of our team, please
take the time to review the valuable benets listed in this booklet. Be sure to
complete your online enrollment information carefully and choose the benet
options that best meet your needs.
Your enrollment period is the only time that you are permitted to make benet
changes outside of an IRS qualied change in status. During enrollment,
you can review your benet plans, update your beneciary and dependent
information and make necessary adjustments. You must designate your life
insurance beneciaries in the Bentek system. Throughout the year, you may
review your benet plans and make changes to beneciary designations.
We recommend that you log into the Bentek system well in advance of your
enrollment deadline. If you have a question or need more information, please
contact the HR Benets Team. For technical support only, please call Bentek.
Online Benet Enrollment
South Florida Water Management District provides employees with
an online benets enrollment platform through Bentek’s Employee
Benets Center (EBC). The EBC provides benet-eligible employees the
ability to select or change insurance benets online during the annual
Open Enrollment Period or New Hire Orientation.
Accessible 24 hours a day, throughout the year, employee may log
in and review comprehensive information regarding benet plans,
and view and print an outline of benet elections for employee and
dependent(s). Employee also has access to important forms and carrier
links and can review and make changes to Life insurance beneciary
designations.
To Access the Employee Benets Center:
9
Log on to www.mybentek.com/sfwmd
Please Note: Link must be addressed exactly as written. Due to security
reasons, the website cannot be accessed by Google or other search engines.
9
To create a Bentek account, remember to add two (2) zeros in
front of your Employee ID#. Example: 0012345
9
Sign in using a previously created username and password or
click "Create an Account" to set up a username and password.
9
If employee has forgotten username and/or password, click
on the link “Forgot Username/Password” and follow the
instructions.
9
Once logged on, navigate using the Launchpad to review
current enrollment, learn about benet options, and make
any benet changes or update beneciary designations.
For technical issues directly related to using the EBC, please
call (888) 5-Bentek (523-6835) or email Bentek Support at
suppor[email protected], Monday through Friday during regular
business hours 8:30am - 5:00pm.
To access Bentek using a mobile
device, scan code.

2
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Group Insurance Eligibility
The District’s group insurance calendar year is
January 1, 2024 through December 31, 2024.
Employee Eligibility
Coverage for District employees is eective the rst of the month following
one (1) full month of employment. For example, if employee is hired on April
11, coverage will be eective on June 1.
New Hire Enrollment
• Benet elections must be completed before the eective date of
coverage.
Please Note: Appropriate documentation is required for all dependents
covered under any District insurance plan. Deadline to submit dependent
documentation is 30 days from the eective date of employee elections.
Submit copies of documentation to the HR Benets Team.
• Benet-eligible employees, must elect coverage for any plan(s)
in which they would like to enroll. Employees will be responsible
for any and all premiums, deductibles, and copays that may apply.
Enrollment in EAP, Basic Life, AD&D and Long Term Disability core
coverage is automatic and paid for by the District.
• After the eective date of coverage, no changes, additions or
cancellations of employee insurance coverage can be made unless
the employee experiences a Qualifying Event, contacts the HR
Benets Team, and provides documentation within 30 days of
event. (See Qualifying Events and Section 125).
Job Changes
Some job changes result in gain, loss or change in insurance benets. See
Qualifying Event section or contact the HR Benets Team for more information.
Employees should check their payroll stub following a job change to ensure
payroll deductions continue without interruption.
Terminating and Retiring Employee
During the plan year, a terminating employee is covered until the last day of
the month:
• In which employment ends.
• In which employee ceases being in a benet eligible position.
• In which employee retires.
• However, Life and Disability insurance coverage ends with the last
payroll premium payment.
Please contact the HR Benets Team if further clarication is required.
Separation of Employment
If an employee separates employment from the District, medical insurance
and most other benets, will continue through the end of month in which
separation occurred. COBRA continuation of coverage may be available as
applicable by law. However, for Life and Disability insurance, coverage ends
with the last payroll premium payment.
Chard Snyder | Customer Service: (888) 993-4646 | www.chard-snyder.com
Dependent Eligibility
A dependent is dened as the legal spouse and/or dependent child(ren) of the
participant or spouse. The term “child” includes any of the following:
• A natural child • A stepchild • A legally adopted child
• A newborn child (up to the age of 18 months) of a covered
dependent (Florida State Statute)
• A child for whom legal guardianship has been awarded to the
participant or the participant’s spouse
Employees must provide supporting documentation to the HR Benets Team
when adding dependents to the plan. Dependents will be removed from
the coverage if required documentation, such as marriage license or birth
certicate, is not received by the District within 30 days of the Qualifying Event.
Dependent Age Requirements
Medical and Dental PPO Coverage: A dependent child may be
covered through the end of calendar year in which the child turns age
26. An over-age dependent may continue to be covered on the medical
plan to the end of the calendar year in which the child reaches the age
of 30, if the dependent meets all of the following requirements:
• Unmarried with no dependents; and
• A Florida resident, or full-time or part-time student; and
• Otherwise uninsured; and
• Not entitled to Medicare benets under Title XVIII of the
Social Security Act, unless the child is disabled.
Dental HMO Coverage: A dependent child may be covered through
the end of the calendar year in which the child turns age 26.
Vision Coverage: A dependent child may be covered through the end
of the calendar year in which the child turns age 26.
JANUARY
01

3
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Group Insurance Eligibility (Continued)
Disabled Dependents
Coverage for a dependent child may be continued beyond age 26 if:
• The dependent is physically or mentally disabled and incapable of
self-sustaining employment (prior to age 26); and
• Primarily dependent upon the employee for support; and
• The dependent is otherwise eligible for coverage under the group's
insurance plans; and
• The dependent has been continuously insured.
Proof of disability will be required upon request. Please contact the HR Benets
Team if further clarication is needed.
Taxable Dependents
Employee covering adult child(ren) under employee's medical and dental PPO
insurance plans may continue to have the related coverage premiums payroll
deducted on a pre-tax basis through the end of the calendar year in which
dependent child reaches age 26. Beginning January 1 of the calendar year
in which dependent child reaches age 27 through the end of the calendar
year in which the dependent child reaches age 30, imputed income must be
reported on the employee’s W-2 for that entire tax year and will be subject
to all applicable Federal, Social Security and Medicare taxes. Imputed income
is the dollar value of insurance coverage attributable to covering each adult
dependent child.
Contact the HR Benefits Team for further details if covering an adult
dependent child who will turn age 27 any time during the upcoming calendar
year or for more information.
Please Note: There is no imputed income if adult dependent child is eligible to be
claimed as a dependent for Federal income tax purposes on the employee’s tax return.
Medicare Eligible
As long as Employee continues to participate in the District's group health
insurance, Employee and/or spouse can delay enrollment in Medicare Part B
until employee's retirement/separation from the District. It is important to
contact Medicare to ensure enrollment in Part A.
Active employees turning age 65 should contact Social Security to sign up for
Medicare Part A at least four (4) months prior to their 65th birthday.
To learn more, visit http://medicare.gov or speak with a Medicare representative
1-800-Medicare, (1-800-633-4227).
Documentation Requirements
All dependents must have an established legal relationship to the employee to
be covered under the benet program. The types of documentation accepted
are as stated in the table below. Employees with dependents enrolled in the
group insurance plans are advised that they will be required to comply with
this process or continued coverage for such dependents may be jeopardized.
Dependent Relationship Documentation Required
Spouse
• Copy of legal government issued
marriage certicate
Dependent child(ren) under age 26
• Copy of State issued birth
certicate(s) OR copy of legal
guardianship court documents listing
the employee as legal guardian
Step-child(ren) under age 26
• Copy of State issued birth
certicate(s)
• AND the appropriate dependent
child documentation listed above
Child(ren) under legal guardianship,
or custody under age 26
• Copy of court documents showing
legal guardianship OR legal custody
documentation
Child(ren) adopted or in the process
of adoption under age 26
• Copy of court documents of the legal
adoption showing relationship to
and placement in the employee’s
house OR adoption certicate
Child(ren) age 27-30
• Copy of state issued birth
certicate(s) or legal guardianship
court documents, listing the
employee or spouse as parent/legal
guardian
• AND Overage Dependent Adavit
signed by employee
Please Note: Religious documents and registration cards are not acceptable proof.
Employee may “black out” nancial information.

4
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Qualifying Events and Section 125
Section 125 of the Internal Revenue Code
Premiums for medical, dental, vision insurance, contributions to Flexible Spending
Accounts (FSA), and/or certain supplemental policies are deducted through a
Cafeteria Plan established under Section 125 of the Internal Revenue Code and
are pre-taxed to the extent permitted. Under Section 125, changes to employee's
pre-tax benets can be made ONLY during the Open Enrollment Period unless
the employee or qualied dependent(s) experience(s) a Qualifying Event and the
request to make a change is made within 30 days of the Qualifying Event. Certain
benets, such as, Flexible Spending Accounts, cannot be changed outside of
enrollment, even if a Qualifying Event has occurred.
Under certain circumstances, employee may be allowed to make changes to
benet elections during the plan year if the event aects the employee, spouse
or dependent’s coverage eligibility. An “eligible” Qualifying Event is determined
by Section 125 of the Internal Revenue Code. Any requested changes must be
consistent with and due to the Qualifying Event.
Examples of Qualifying Events:
• Employee gets married or divorced
• Birth of a child
• Employee gains legal custody or adopts a child
• Employee's spouse and/or other dependent(s) die(s)
• Loss or gain of coverage due to employee, employee's spouse and/or
dependent(s) termination or start of employment
• An increase or decrease in employee's work hours causes eligibility or
ineligibility
• A covered dependent no longer meets eligibility criteria for coverage
• A child gains or loses coverage with other parent or legal guardian
• Change of coverage under an employer’s plan
• Gain or loss of Medicare coverage
• Losing or becoming eligible for coverage under a State Medicaid or CHIP
(including Florida Kid Care) program (60 day notication period)
• A change in the place of residence of the employee, spouse, or
dependent that aects eligibility to be covered under The District's plan,
which includes moving out of an HMO service area.
Please Note: Purchasing or dropping an individual policy for the employee or employee's
dependent IS NOT a Qualifying Event and does not permit adding or dropping coverage
for employee or employee's dependent from the group health plan outside of Open
Enrollment.
IMPORTANT NOTES
If employee experiences a Qualifying Event, contact the HR Benefits
Team within 30 days to make the appropriate changes to employee’s
coverage. Employee may be required to furnish valid documentation
supporting a change in status or “Qualifying Event”. If approved,
changes may be eective the date of the Qualifying Event or the rst
of the month following the Qualifying Event. Newborns are eective
on the date of birth. Qualifying Events will be processed in accordance
with employer and carrier eligibility policy. Beyond 30 days, requests
will be denied and employee may be responsible, both legally
and nancially, for any claim and/or expense incurred as a result of
employee or dependent who continues to be enrolled but no longer
meets eligibility requirements.
Summary of Benets and Coverage
A Summary of Benefits & Coverage (SBC) for the Medical Plan is provided on
SFWMD employee portal (iWeb). The summary is an important item in understanding
the benet options. A free paper copy of the SBC document may be requested or is
available as follows:
From: The HR Benets Team
Address: 3301 Gun Club Road
West Palm Beach, FL 33406
Phone: (561) 686-8800
Email: HRBenetsT[email protected]
Website: www.mybentek.com/sfwmd
The SBC is only a summary of the plan’s coverage. A copy of the plan document, policy,
or certicate of coverage should be consulted to determine the governing contractual
provisions of the coverage. A copy of the group certicate of coverage can be found on
the mysfwmd homepage under the "Benets tab".
If employees have any questions about the plan oerings or coverage options, please
contact the HR Benets Team.

5
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Ride the Wave to Wellness
Ride the Wave to Wellness is a program sponsored in partnership by the South
Florida Water Management District and Cigna to improve the health and well-
being of District employees.
This program focuses on whole-person health: physical, emotional, social,
nancial, and environmental.
Employees may participate in various wellness events and programs. The
program caters to all employees, at all levels and interests, and features
educational and engaging activities such as:
9
Annual Health Screenings
9
Cooking Demos
9
Fitness Classes
9
Lunch and Learn Seminars
9
Health and Wellness Fair
9
Omada Diabetes Prevention
Program
9
Chronic Condition Coaching
9
Cigna Total Behavioral Health
9
Active and Fit Direct
Omada Diabetes Prevention Program
Cigna has partnered with Omada Health who is the nation’s leading CDC-
recognized provider of the Diabetes Prevention Program (DPP). Through its
DPP, Omada delivers cost- eective prevention services for populations at
risk or in the early stages of developing type 2 diabetes and other chronic
conditions. This program is at no additional cost to employees and adult
dependents on the Cigna medical plan. Those who qualify will learn how to
adapt healthier eating habits, increase activity and reduce the risks of type 2
diabetes and heart disease. Contact your Onsite Cigna Well-Being Coordinator
for additional information.
Cigna Healthcare
Onsite Cigna Well-Being Coordinator: Ratasha Iribarren
Phone: (561) 682-6086 l Email: [email protected]v
Cigna Behavioral Programs
Whether you need help reducing stress, are feeling motivated to make a
change in your life, or need to talk to someone, Cigna oers a variety of
behavioral support tools and services to help ensure you get the support that
works best for you.
To learn more or access services, visit www.mycigna.com, Coverage, Employee
Assistance Program. You can also call (877) 231-1492 for referrals or go online,
search the provider directory and obtain an authorization.
For links to iPrevail and Happify programs, visit the Wellness Page-Emotional
Health on www.mycigna.com. You can also call Cigna's customer service at
(800) 244-6224.
Health Coaching
Did you know your health plan comes with chronic condition health coaching?
That means employees have access to a team of trained health professionals
– including nurses, nutritionists, dietitians and certied health educators. And
it’s at no additional cost.
If employee or covered dependents are living with a chronic condition – such
as diabetes, heart disease or depression – a health coach can work one-on-one
over the phone to assist with the following benets:
9
Understand and follow the treatment your provider prescribes.
9
Stay motivated to set and reach personal health goals.
9
Access additional health and wellness resources.
9
Get reliable answers and information based on specic health needs.
It's as easy as picking up the phone – either by answering when we call you, or
calling Cigna directly at (800) 244-6224.
Medical Plan Resources
Cigna oers all enrolled members and dependents additional services and discounts through value added programs. For more details regarding other medical plan
resources, please contact Cigna's customer service at (800) 244-6224, or visit www.mycigna.com.
24 Hour Help Information Hotline (800) CIGNA-24
The Cigna 24-Hour Health Information Line provides access to helpful, reliable
information and assistance from qualied health information nurses on a wide
range of health topics 24 hours a day, any day of the year. Not sure what to do
when a child has a fever in the middle of the night? Not sure if treatment from
a doctor is necessary for an injury? There are over 1,000 topics in the Health
Information Library that include free audio, video and printed information on
aging, women’s health, nutrition, surgery and specic medical conditions to
help member weigh the risks and advantages of treatment options. The call is
free and is strictly condential.
Cigna 90 Now
Employees taking maintenance medications which are prescribed for chronic
long-term conditions and are taken on a regular recurring basis, may now
ll these prescriptions at a Cigna 90 Now pharmacy or through Cigna Home
Delivery. Employees choosing to use a Cigna 90 Now pharmacy or through
Cigna Home Delivery will help keep costs down and allows the District not to
pass along additional cost to the employees. To nd a Cigna 90 Now pharmacy,
log on to www.mycigna.com.

6
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Medical Plan Resources (Continued)
The myCigna Mobile App
The myCigna mobile app is an easy way to organize and access important
health information. Anytime. Anywhere. Download it today from the App
Store
SM
or Google Play™. With the myCigna mobile app, member can:
9
Find a doctor, dentist or health
care facility
9
Access maps for instant driving
directions
9
View ID cards for the entire family
9
Review deductibles, account
balances and claims
9
Compare prescription drug costs
9
Speed-dial Cigna Home Delivery
Pharmacy™
9
Store and organize all important
contact info for doctors, hospitals,
and pharmacies
9
Add health care professionals to
contact list right from a claim or
directory search
Covered Treatment Options for Tobacco Cessation
The District oers coverage for tobacco cessation medications and nicotine
replacement therapy with a $0 Copay. A prescription from your physician is required.
Below is a list of covered products:
9
Bupropion SR
9
NicoDerm CQ
9
Nicorelief
9
Nicotrol
9
Nicorette
9
Zyban
Infertility Treatment
The District oers a basic benet option for infertility treatments. This benet
is at no additional cost to Cigna members, and provides coverage for the
following:
9
Testing to determine the cause of infertility
9
Treatment and/or procedures to restore fertility
9
Articial/intrauterine insemination
Healthy Rewards
Cigna’s Healthy Rewards is provided automatically at no additional cost and
oers access to discounted health and wellness programs at participating
providers. Member can log on to www.mycigna.com and select Healthy
Rewards to learn more about these programs or call (800) 870-3470.
9
Vision Care
9
Lasik Vision Correction Services
9
Fitness Club Discounts
9
Nutrition Discounts
9
Hearing Care
Telehealth
Cigna provides access to telehealth services as part of the medical plan.
MDLIVE is a convenient phone and video consultation company that provides
immediate medical assistance for a wide range of minor conditions, including
prescriptions. MDLIVE also provides access to Behavioral Virtual Health with
licensed counselors and psychiatrists who can diagnose, treat and prescribe
most medications for nonemergency behavioral conditions such as, addictions,
bipolar disorder, child/adolescent issues, depression, eating disorders, stress,
trauma/PTSD and many others.
The benet is provided to all enrolled members. This program allows members
24 hours a day, seven (7) days a week on-demand access to aordable medical
care with a board-certied doctor via secure video chat and phone, without
leaving your home or oce, when needing immediate care for non-emergent
medical issues. Telehealth should be considered when your primary care doctor
is unavailable, after-hours or on holidays for non-emergency needs. Telehealth
is a cost-eective alternative to a convenience care clinic, urgent care center or
emergency room. Many urgent care ailments can be treated with telehealth,
such as:
9
Sore Throat
9
Headache
9
Stomachache
9
Fever
9
Cold and Flu
9
Allergies
9
Rash
9
Acne
9
UTIs and More
Telehealth doctors do not replace employee's primary care physician. Members
should pre-register on MDLIVE through Cigna. Telehealth services are only
available for minor, non-life threatening conditions. A credit card is required
for a temporary charge until the claim is processed.
Service Type HMO Plan OAPIN Plan
General Medicine No Charge No Charge
Register On:
MDLIVE | Customer Service: (888) 726-3171 | www.mycigna.com

7
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Locate a Provider
To search for a participating provider,
contact Cigna's customer service or visit
www.mycigna.com. When completing
the necessary search criteria, select
Cigna Seamless HMO network.
Plan References
*The Cigna Seamless HMO network
provides access to a broader network of
doctors outside the standard Cigna HMO
network.
**Tier 1 Network Providers
may provide a higher level of network
benets if services are received from a
Tier 1 designated provider.
***LabCorp or Quest Diagnostics are the
preferred labs for bloodwork through
Cigna. When using a lab other than
LabCorp or Quest, please conrm they
are contracted with Cigna’s Seamless
HMO network prior to receiving services.
Important Notes
Members have direct access to care from the
following specialties without a referral:
No Limitations:
· OB/GYN · Mental Health
· Substance Abuse
6 Visit Limitations:
· Dermatology · Podiatry
· Chiropractic Care
Save money on select specialty
medications by enrolling into the
SaveonSP Program. Cigna will contact
members who are lling select specialty
medications that are eligible for the
SaveonSP program. Members enrolled
under this program may incur $0 cost for
specialty medications.
Cigna Network HMO Plan At-A-Glance
Network Seamless HMO*
Calendar Year Deductible (CYD) In-Network
Single $0
Family $0
Coinsurance
Member Responsibility 0%
Calendar Year Out-of-Pocket Limit
Single $2,500
Family $5,000
What Applies to the Out-of-Pocket Limit? Copays and Rx
Physician Services
Primary Care Physician (PCP) Office Visit (PCP Designation is Required) $20 Copay
Specialist Office Visit** Tier 1 Provider: $40 Copay / Non-Tier 1 Provider: $55 Copay
Physical Therapy $55 Copay
Non-Hospital Services; Freestanding Facility
Clinical Lab (Bloodwork)*** No Charge
X-rays No Charge
Advanced Imaging (MRI, PET, CT) No Charge
Outpatient Surgery in Surgical Center No Charge
Physician Services at Surgical Center No Charge
Urgent Care (Per Visit; Waived if Admitted) $50 Copay
Hospital Services
Inpatient Hospital (Per Admission) $250 Copay
Physician Services at Hospital No Charge
Emergency Room (Per Visit; Waived if Admitted) $200 Copay
Mental Health/Alcohol & Substance Abuse
Inpatient Hospital Services (Per Admission) $250 Copay
Outpatient Services (Per Visit) No Charge
Outpatient Office Visit $20 Copay
Prescription Drugs (Rx)
Generic $10 Copay
Preferred Brand Name $20 Copay
Non-Preferred Brand Name $40 Copay
Mail Order Drug (90-Day Supply) or Rx 90 Now Network
†
2x Retail Copay
†
Cigna 90 Now - Pharmacy Network for maintenance prescriptions. Visit cigna.com/rx90network to locate a pharmacy.
8
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Locate a Provider
To search for a participating provider,
contact Cigna's customer service or visit
www.mycigna.com. When completing
the necessary search criteria, select
Open Access Plus network.
Plan References
*Tier 1 Network Providers
may provide a higher level of network
benets if services are received from a
Tier 1 designated provider.
**LabCorp or Quest Diagnostics are the
preferred labs for bloodwork through
Cigna. When using a lab other than
LabCorp or Quest, please conrm they
are contracted with Cigna’s Open Access
Plus network prior to receiving services.
Important Notes
Save money on select specialty
medications by enrolling into the
SaveonSP Program. Cigna will contact
members who are lling select specialty
medications that are eligible for the
SaveonSP program. Members enrolled
under this program may incur $0 cost for
specialty medications.
Cigna OAP In-Network Plan At-A-Glance
Network Open Access Plus
Calendar Year Deductible (CYD) In-Network
Single $150
Family $300
Coinsurance
Member Responsibility 20%
Calendar Year Out-of-Pocket Limit
Single $2,500
Family $5,000
What Applies to the Out-of-Pocket Limit? Deductible, Coinsurance, Copays and Rx
Physician Services
Primary Care Physician (PCP) Office Visit $20 Copay
Specialist Office Visit* Tier 1 Provider: $25 Copay / Non-Tier 1 Provider: $40 Copay
Physical Therapy $40 Copay
Non-Hospital Services; Freestanding Facility
Clinical Lab (Bloodwork)** No Charge
X-rays No Charge
Advanced Imaging (MRI, PET, CT) 20% After CYD
Outpatient Surgery in Surgical Center 20% After CYD
Physician Services at Surgical Center 20% After CYD
Urgent Care (Per Visit) $35 Copay + CYD
Hospital Services
Inpatient Hospital (Per Admission) $250 Copay + 20% After CYD
Physician Services at Hospital 20% After CYD
Emergency Room (Per Visit) $200 Copay + CYD
Mental Health/Alcohol & Substance Abuse
Inpatient Hospital Services (Per Admission) $250 Copay + 20% After CYD
Outpatient Services (Per Visit) No Charge After CYD
Outpatient Office Visit $25 Copay
Prescription Drugs (Rx)
Generic $10 Copay
Preferred Brand Name $20 Copay
Non-Preferred Brand Name $40 Copay
Mail Order Drug (90-Day Supply) or Rx 90 Now Network
†
2x Retail Copay
†
Cigna 90 Now - Pharmacy Network for maintenance prescriptions. Visit cigna.com/rx90network to locate a pharmacy.

9
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Medical Insurance
The District oers medical insurance through Cigna Healthcare to benet-eligible employees. The costs for coverage are listed in the premium tables below. For more detailed
information about the medical plans, please refer to the carrier's Summary of Benefits and Coverage (SBC) document or contact Cigna's customer service.
Medical Insurance – Cigna Network HMO Plan
Payroll Deductions - Regular Premiums
Tier of Coverage
Employee
Bi-Weekly Premium
Employee
Monthly Premium
District
Monthly Contribution
Total
Monthly Premium
Employee Only $12.50 $25.00 $822.34 $847.34
Employee + 1 Child $122.50 $245.00 $1,595.29 $1,840.29
Employee + 1 Child (OAD)* $142.50 $285.00 $1,591.98 $1,876.98
Employee + Spouse $135.00 $270.00 $1,606.98 $1,876.98
Employee + Family $140.00 $280.00 $1,709.35 $1,989.35
Employee + Family
(Employee + Children)
$140.00 $280.00 $1,709.35 $1,989.35
Employee + Family (OAD)* $152.50 $305.00 $1,684.35 $1,989.35
Employee + Family (OAD)*
(Employee + Children)
$152.50 $305.00 $1,684.35 $1,989.35
*OAD (Overage Dependent) = Dependent Child Over-age 26
Medical Insurance – Cigna Network HMO Plan
Payroll Deductions - Managers and SES Premiums
Tier of Coverage
Employee
Bi-Weekly Premium
Employee
Monthly Premium
District
Monthly Contribution
Total
Monthly Premium
Employee Only $5.25 $10.49 $836.85 $847.34
Employee + 1 Child $18.41 $36.81 $1,803.48 $1,840.29
Employee + 1 Child (OAD)* $18.60 $37.20 $1,839.78 $1,876.98
Employee + Spouse $18.77 $37.54 $1,839.44 $1,876.98
Employee + Family $19.90 $39.79 $1,949.56 $1,989.35
Employee + Family
(Employee + Children)
$19.90 $39.79 $1,949.56 $1,989.35
Employee + Family (OAD)* $19.59 $39.17 $1,950.18 $1,989.35
Employee + Family (OAD)*
(Employee + Children)
$19.59 $39.17 $1,950.18 $1,989.35
*OAD (Overage Dependent) = Dependent Child Over-age 26
Cigna Healthcare | Customer Service: (800) 244-6224 | www.mycigna.com

10
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Medical Insurance
The District oers medical insurance through Cigna Healthcare to benet-eligible employees. The costs for coverage are listed in the premium tables below. For more detailed
information about the medical plans, please refer to the carrier's Summary of Benefits and Coverage (SBC) document or contact Cigna's customer service.
Medical Insurance – Cigna OAP In-Network Plan
Payroll Deductions - Regular Premiums
Tier of Coverage
Employee
Bi-Weekly Premium
Employee
Monthly Premium
District
Monthly Contribution
Total
Monthly Premium
Employee Only $17.50 $35.00 $839.86 $874.86
Employee + 1 Child $144.00 $288.00 $1,807.99 $2,095.99
Employee + 1 Child (OAD)* $188.25 $376.50 $1,841.03 $2,217.53
Employee + Spouse $161.25 $322.50 $1,895.03 $2,217.53
Employee + Family $169.50 $339.00 $2,011.53 $2,350.53
Employee + Family
(Employee + Children)
$169.50 $339.00 $2,011.53 $2,350.53
Employee + Family (OAD)* $195.75 $391.50 $1,959.03 $2,350.53
Employee + Family (OAD) *
(Employee + Children)
$195.75 $391.50 $1,959.03 $2,350.53
*OAD (Overage Dependent) = Dependent Child Over-age 26
Medical Insurance – Cigna OAP In-Network Plan
Payroll Deductions - Managers and SES Premiums
Tier of Coverage
Employee
Bi-Weekly Premium
Employee
Monthly Premium
District
Monthly Contribution
Total
Monthly Premium
Employee Only $5.42 $10.83 $864.03 $874.86
Employee + 1 Child $20.96 $41.92 $2,054.07 $2,095.99
Employee + 1 Child (OAD)* $25.47 $50.93 $2,166.60 $2,217.53
Employee + Spouse $22.18 $44.35 $2,173.18 $2,217.53
Employee + Family $23.51 $47.01 $2,303.52 $2,350.53
Employee + Family
(Employee + Children)
$23.51 $47.01 $2,303.52 $2,350.53
Employee + Family (OAD)* $29.67 $59.33 $2,291.20 $2,350.53
Employee + Family (OAD)*
(Employee + Children)
$29.67 $59.33 $2,291.20 $2,350.53
*OAD (Overage Dependent) = Dependent Child Over-age 26
Cigna Healthcare | Customer Service: (800) 244-6224 | www.mycigna.com

11
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Dental Insurance
Cigna DHMO Plan
The District oers dental insurance through Cigna Healthcare to benet-
eligible employees. The costs for coverage are listed in the premium table
below and a brief summary of benets is provided on the following page. For
more detailed information about the dental plan, please refer to the carrier's
summary plan document or contact Cigna's customer service.
Dental Insurance – Cigna DHMO Plan
Payroll Deductions - All Employee Premiums
Tier of Coverage
Employee
Bi-Weekly
Premium
Employee
Monthly
Premium
District
Monthly
Contribution
Total
Monthly
Premium
Employee Only $4.91 $9.82 $26.37 $36.19
Employee + 1 Child $15.95 $31.90 $40.65 $72.55
Employee + Spouse $15.95 $31.90 $40.65 $72.55
Employee + Family $24.65 $49.30 $63.63 $112.93
Employee + Family
(Employee + Children)
$24.65 $49.30 $63.63 $112.93
In-Network Benets
The DHMO plan is an in-network only plan that requires all services be received
by a Primary Dental Provider (PDP). Employee and dependent(s) may select
any participating dentist in the Dental Care Access network to receive covered
services. There is no coverage for services received out-of-network.
The DHMO plan’s schedule of benets is set forth by the Patient Charge Schedule
(fee schedule) which is highlighted on the following page. Please refer to the
summary plan document for a detailed listing of charges and benets.
Out-of-Network Benets
The DHMO plan does not provide benets for services rendered by providers or
facilities who do not participate in the Cigna Dental Care Access network or by
an in-network provider not designated as the primary dental provider (unless
referred by an employee's primary dental provider). Employee will pay out of
pocket if they utilize any out-of-network providers.
Calendar Year Deductible
There is no calendar year deductible.
Calendar Year Benet Maximum
There is no benet maximum.
IMPORTANT NOTES
• Children under age 13 may visit a pediatric dentist. Contact Cigna for a list
of pediatric dentists in the network. Once the child reaches age 13, a referral
with approved medical reasons by Cigna will be required prior to being seen
by a pediatric dental provider.
• Coverage and age limitations may apply to some services. Check the plan
summary or contact Cigna prior to having services rendered.
• The summary is provided as a convenient reference and additional charges
may apply. For a full listing of covered services, exclusions, and stipulations,
refer to the plan’s Schedule of Benets or contact Cigna’s customer service
for details specic to a procedure.
Cigna Healthcare
Customer Service: (800) 244-6224 | www.mycigna.com

12
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Cigna DHMO Plan At-A-Glance
Network Dental Care Access
Calendar Year Deductible (CYD) In-Network Only
Per Member
Does Not ApplyPer Family
Waived for Class I Services?
Calendar Year Benet Maximum In-Network Only
Per Member Does Not Apply
Class I Services: Diagnostic & Preventive Care Code In-Network
Office Visit Fee D9430 $0 Copay
Routine Oral Exam (4 Per 12 Months) 0150 $0 Copay
Routine Cleanings (2 Per Calendar Year) 1110/1120 $0 Copay
Bitewing X-rays (2 Films) 0272 $0 Copay
Complete X-rays (1 Set Every 3 Years) 0210 $0 Copay
Fluoride Treatments (Child to age 19; 2 Per Calendar Year) 1208 $0 Copay
Sealants - Per Tooth 1351 $0 Copay
Space Maintainers 1510 $0 Copay
Emergency Care to Relieve Pain (During Regular Hours) 9110 $0 Copay
Class II Services: Basic Restorative Care
Fillings (Amalgam) 2140 $0 Copay
Fillings (Composite; Anterior) 2330 $0 Copay
Fillings (Composite; Posterior - 3 Surfaces) 2393 $82 Copay
Simple Extractions 7140 $12 Copay
Surgical Extractions (Soft Tissue) 7220 $21 Copay
Root Canal Therapy* (Excluding Final Restoration) 3330 $280 Copay
Periodontal Maintenance (4 Per Calendar Year; Per Visit) 4910 $66 Copay
General Anesthesia (15 Minute Increments) 9223 $95 Copay
Repairs to Dentures* 5510 $65 Copay
Class III Services: Major Restorative
Bridges* 5213/5214 $575 Copay
Crowns* 2752 $355 Copay
Dentures* 5110/5120 $500 Copay
Class IV Services: Orthodontia
Lifetime Maximum Does Not Apply Does Not Apply
Benefit — Child* (Up to 19th Birthday) 8670 $2,184 Copay
Benefit — Adult* 8670 $2,904 Copay
Locate a Provider
To search for a participating provider,
contact Cigna’s customer service
or visit www.mycigna.com. When
completing the necessary search
criteria, select Cigna Dental Care Access
network.
Plan References
*Additional charges may apply for some
services. Please see the plan summary
or contact Cigna’s customer service for
details specic to the procedure.
Important Notes
• Each covered employee and family
member(s) may receive two (2) routine
cleanings per calendar year covered
under the preventive benet. Two (2)
additional cleanings are available at the
charge of a copay ($45 for adults/$30
for children).
• Referrals and prior authorizations are
required to see a specialist (oral surgeon,
periodontist, orthodontist, etc.) within
the network.
• Waiting periods and age limitations
may apply for some services.

13
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Dental Insurance
Cigna DPPO Plan
The District oers dental insurance through Cigna Healthcare to benet-
eligible employees. The costs for coverage are listed in the premium table
below and a brief summary of benets is provided on the following page. For
more detailed information about the dental plan, please refer to the carrier's
summary plan document or contact Cigna's customer service.
Dental Insurance – Cigna DPPO Plan
Payroll Deductions - All Employee Premiums
Tier of Coverage
Employee
Bi-Weekly
Premium
Employee
Monthly
Premium
District
Monthly
Contribution
Total
Monthly
Premium
Employee Only $5.00 $10.00 $63.50 $73.50
Employee + 1 Child $20.00 $40.00 $101.96 $141.96
Employee + Spouse $20.00 $40.00 $101.96 $141.96
Employee + Family $30.00 $60.00 $136.35 $196.35
Employee + Family
(Employee + Children)
$30.00 $60.00 $136.35 $196.35
In-Network Benets
The DPPO plan provides benets for services received from in-network and
out-of-network providers. It is also an open-access plan which allows for
services to be received from any dental provider without having to select a
Primary Dental Provider (PDP) or obtain a referral to a specialist. The network of
participating dental providers the plan utilizes is the Total Cigna DPPO network.
Employee will save money by utilizing a dental provider in this network. These
participating dental providers have contractually agreed to accept Cigna’s
contracted fee or “allowed amount.” This fee is the maximum amount a Cigna
dental provider can charge a member for a service. The member is responsible
for a Calendar Year Deductible (CYD) and then coinsurance based on the plan’s
charge limitations.
Please Note: Total DPPO dental members have the option to utilize a dentist that
participates in either Cigna’s Advantage network or DPPO network. However, members
that use the Cigna Advantage network will see additional cost savings from the added
discount that is allowed for using an Advantage network provider. Members are
responsible for verifying whether the treating dentist is an Advantage Dentist or a DPPO
Dentist.
Out-of-Network Benets
Out-of-network benets are used when member receives services by a non-
participating Total Cigna DPPO provider. Cigna reimburses out-of-network
services based on what it determines as the Maximum Reimbursable Charge
(MRC). The MRC is dened as the most common charge for a particular dental
procedure performed in a specic geographic area. If services are received from
an out-of-network dentist, the member will pay the out-of-network benet
plus the dierence between the amount that Cigna reimburses (MRC) for such
services and the amount charged by the dentist. This is known as balance billing
(does not apply for out-of-network Cigna DPPO providers). Balance billing is in
addition to any applicable plan deductible or coinsurance responsibility.
Calendar Year Deductible
The DPPO plan requires a $50 individual or a $150 family deductible to be met
for in-network or out-of-network services before most benets will begin. The
deductible is waived for preventive services.
Calendar Year Benet Maximum
The maximum benet (coinsurance) the DPPO plan will pay for each covered
member is $2,000 and the member will be responsible for all future charges
until the next calendar year for in-network or out-of-network services
combined. All services, including preventive services, accumulate towards the
benet maximum.
IMPORTANT
The summary is provided as a convenient reference and additional charges
may apply. For a full listing of covered services, exclusions, and stipulations,
refer to the plan’s Schedule of Benets or contact Cigna’s customer service for
details specic to a procedure.
Cigna Healthcare
Customer Service: (800) 244-6224 | www.mycigna.com

14
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Locate a Provider
To search for a participating provider,
contact Cigna’s customer service
or visit www.mycigna.com. When
completing the necessary search
criteria, select Total Cigna DPPO
network.
Plan References
*Out-Of-Network Balance Billing:
For information regarding out-of-
network balance billing that may be
charged by an out-of-network providers,
please refer to the Out-of-Network
Benets section on the previous page.
Important Notes
• Each covered employee and family
member(s) may receive up to two (2)
routine cleanings per calendar year
covered under the preventive benet.
• For any dental work expected to cost
$200 or more, the plan will provide a
“Pre-Determination of Benets” upon
the request of the dental provider.
This will assist with determining
approximate out-of-pocket costs
should employee have the dental work
performed.
• Waiting periods and age limitations
may apply.
• Benet frequency limitations may
apply to certain services.
• Cigna does not provide ID cards to
DPPO members. Members should use
their Medical ID card.
Cigna DPPO Plan At-A-Glance
Network Total Cigna DPPO
Calendar Year Deductible (CYD) In-Network Out-of-Network*
Per Member $50 $50
Per Family $150 $150
Waived for Class I Services? Yes
Calendar Year Benet Maximum
Per Member (Includes Class I Services) $2,000
Class I Services: Diagnostic & Preventive Care
Routine Oral Exam (2 Per Calendar Year)
Plan Pays: 100%
Deductible Waived
Plan Pays: 100%
Deductible Waived
(Subject to Balance Billing)
Routine Cleanings (2 Per Calendar Year)
Bitewing X-rays (2 Per Calendar Year)
Complete X-rays (1 Set Every 3 Calendar Years)
Emergency Care to Relieve Pain
Class II Services: Basic Restorative Care
Fillings
Plan Pays: 85%
After CYD
Plan Pays: 85%
After CYD
(Subject to Balance Billing)
Simple Extractions
Endodontics (Root Canal Therapy)
Oral Surgery
Periodontal Services
Anesthetics
Class III Services: Major Restorative Care
Crowns
Plan Pays: 60%
After CYD
Plan Pays: 60%
After CYD
(Subject to Balance Billing)
Bridges
Dentures
Class IV Services: Orthodontia
Lifetime Maximum $3,500
Benefit
Plan Pays: 50%
After CYD
Plan Pays: 50%
After CYD
(Subject to Balance Billing)

15
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Vision Insurance
Cigna Vision Plans
The District oers vision insurance through Cigna Healthcare to benet-eligible
employees. The costs for coverage are listed in the premium tables below and a
brief summary of benets is provided on the following page. For more detailed
information about the vision plan, please refer to the carrier’s summary plan
document or contact Cigna’s customer service.
Vision Insurance – Cigna Core Vision Plan
Payroll Deductions - Regular Premiums
Tier of Coverage
Employee
Bi-Weekly
Premium
Employee
Monthly
Premium
District
Monthly
Contribution
Total
Monthly
Premium
Employee Only $2.50 $5.00 $1.60 $6.60
Employee + 1 Child $4.00 $8.00 $4.50 $12.50
Employee + Spouse $5.00 $10.00 $2.50 $12.50
Employee + Family $6.00 $12.00 $6.40 $18.40
Employee + Family
(Employee + Children)
$6.00 $12.00 $6.40 $18.40
Vision Insurance – Cigna Core Vision Plan
Payroll Deductions - Managers and SES Premiums
Tier of Coverage
Employee
Bi-Weekly
Premium
Employee
Monthly
Premium
District
Monthly
Contribution
Total
Monthly
Premium
Employee Only $0.00 $0.00 $6.60 $6.60
Employee + 1 Child $0.00 $0.00 $12.50 $12.50
Employee + Spouse $0.00 $0.00 $12.50 $12.50
Employee + Family $0.00 $0.00 $18.40 $18.40
Employee + Family
(Employee + Children)
$0.00 $0.00 $18.40 $18.40
Vision Insurance – Cigna Buy-Up Vision Plan
Payroll Deductions - All Employee Premiums
Tier of Coverage
Employee
Bi-Weekly
Premium
Employee
Monthly
Premium
District
Monthly
Contribution
Total
Monthly
Premium
Employee Only $5.00 $10.00 $7.80 $17.80
Employee + 1 Child $10.00 $20.00 $13.70 $33.70
Employee + Spouse $14.00 $28.00 $5.70 $33.70
Employee + Family $21.50 $43.00 $6.70 $49.70
Employee + Family
(Employee + Children)
$21.50 $43.00 $6.70 $49.70
In-Network Benets
The vision plan oers employee and covered dependent(s) coverage for routine
eye care, including eye exams, eyeglasses (lenses and frames) or contact lenses.
To schedule an appointment, covered employee and covered dependent(s)
may select any network provider who participates in the Cigna Vision network.
At the time of service, routine vision examinations and basic optical needs will
be covered as shown on the plan’s schedule of benets. Cosmetic services and
upgrades will be additional if chosen at the time of the appointment.
Out-of-Network Benets
Employee and covered dependent(s) may also choose to receive services
from vision providers who do not participate in the Cigna Vision network.
When going out of network, the provider will require payment at the time of
appointment. Cigna will then reimburse based on the plan’s out-of-network
reimbursement schedule upon receipt of proof of services rendered.
Calendar Year Deductible
There is no calendar year deductible.
Calendar Year Out-of-Pocket Maximum
There is no out-of-pocket maximum. However, there are benet reimbursement
maximums for certain services.
Claims Mailing Address
Cigna Vision Claims Department
PO Box 385018 | Birmingham, AL 35238-5018
Cigna Healthcare
Customer Service: (800) 244-6224 | www.mycigna.com

16
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Cigna Vision Plans At-A-Glance
Plan Core Vision Plan Buy-Up Vision Plan
Network Cigna Vision Cigna Vision
Services In-Network Out-of-Network
Eye Exam No Charge Up to $40 Reimbursement Up to $50 Allowance
Frequency of Services
Examination 24 Months 12 Months
Lenses 24 Months 12 Months
Frames 24 Months 12 Months
Contact Lenses 24 Months 12 Months
Lenses
Single
Covered at 100%
Up to $45 Reimbursement Up to $101 Allowance
Bifocal Up to $90 Reimbursement Up to $203 Allowance
Trifocal Up to $126 Reimbursement Up to $284 Allowance
Frames
Allowance Up to $150 Allowance Up to $45 Reimbursement Up to $150 Allowance
Contact Lenses*
Non-Elective; Medically Necessary Covered at 100% Up to $90 Reimbursement Up to $203 Allowance
Elective (Fitting, Evaluation & Follow-up) Up to $100 Allowance Up to $90 Reimbursement Up to $203 Allowance
Locate a Provider
To search for a participating provider,
contact Cigna’s customer service or visit
www.mycigna.com. When completing
the necessary search criteria, select the
Cigna Vision network.
Plan References
*Contact lenses are in lieu of spectacle
lenses.
Important Notes
• Member options, such as LASIK, UV
coating, progressive lenses, etc. are not
covered in full, but may be available at
a discount.
• Vision Buy Up benets are provided on
a yearly basis.
• Vision Core benets are provided every
other year.
• Benet waiting period is based on
date of service and not on plan change
eective date.
• Eligibility for eye examinations and
materials are based on the calendar
year the services were last received and
are tracked across vision plans.

17
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Flexible Spending Accounts
The District oers Flexible Spending Accounts (FSA) administered through HealthEquity/WageWorks. The FSA plan year is from January 1 to December 31.
Participating employee must re-elect the dollar amount to be deducted each plan year.
There is no automatic enrollment for an FSA. Employees who do not re-elect this benet during Open Enrollment will not have an FSA for the upcoming plan year.
If employee or family member(s) has predictable health care or work-related day care expenses, then employee may benet from participating in an FSA. An FSA allows
employee to set aside money from employee's paycheck for reimbursement of health care and day care expenses they regularly pay. The amount set aside is not taxed
and is automatically deducted from employee’s paycheck and deposited into the FSA. During the year, employee has access to this account for reimbursement of some
expenses not covered by insurance. Participation in an FSA allows for substantial tax savings and an increase in spending power. Participating employee must re-elect
the dollar amount to be deducted each plan year. There are two (2) types of FSAs:
Health Care FSA Dependent Care FSA
This account allows participant to set aside up to an annual
maximum of $3,050. This money will not be taxable income
to the participant and can be used to oset the cost of a
wide variety of eligible medical expenses that generate
out-of-pocket costs. Participating employee can also receive
reimbursement for expenses related to dental and vision
care (that are not classied as cosmetic).
Examples of common expenses that qualify for
reimbursement are listed below.
This account allows participant to set aside up to an annual maximum of $5,000 if the
participating employee is single or married and les a joint tax return ($2,500 if married
and le a separate tax return) for work-related day care expenses. Qualied expenses
include day care centers, preschool, and before/after school care for eligible children and
adults.
Please note, if a family's income is over $20,000, this reimbursement option will likely
save participants more money than the dependent day care tax credit taken on a tax
return. To qualify, dependents must be:
• The participants dependent, and
• A child under the age of 13, or
• A child, spouse or other dependent who is physically or mentally incapable of
self-care and spends at least eight (8) hours a day in the participant's household.
Please Note: The entire Health Care FSA election is available for use on
the first day coverage is effective.
Please Note: Unlike the Health Care FSA, reimbursement is only up to the amount that has been deducted
from the participant’s paycheck for the Dependent Care FSA.
A sample list of qualied health care expenses eligible for reimbursement include, but not limited to, the following:
9
Prescription/Over-the-Counter Medications
9
Physician Fees and Oce Visits
9
LASIK Surgery
9
Menstrual Products
9
Drug Addiction/Alcoholism Treatment
9
Mental Health Care
9
Ambulance Service
9
Experimental Medical Treatment
9
Nursing Services
9
Chiropractic Care
9
Corrective Eyeglasses and Contact Lenses
9
Optometrist Fees
9
Dental and Orthodontic Fees
9
Hearing Aids and Exams
9
Sunscreen SPF 15 or Greater
9
Diagnostic Tests/Health Screenings
9
Injections and Vaccinations
9
Wheelchairs
Log on to http://www.irs.gov/publications/p502/index.html for additional details regarding qualied and non-qualied expenses.

18
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Flexible Spending Accounts (Continued)
FSA Guidelines
• The Health Care FSA has a 90 day run out period at the end of the calendar
year in which to submit reimbursement on eligible expenses incurred during
the period of coverage within the plan year January 1 – December 31,
2024. For 2024, the run out period ends March 31, 2025.
• Only Health Care FSA allows a grace period at the end of the plan year. The
grace period allows additional time to incur claims and use any unused
funds on eligible expenses after the plan year ends. Once the grace period
ends, any unused funds still remaining in the account will be forfeited. The
2024 grace period ends on March 15, 2025.
• When a plan year and grace period ends, and all claims have been led,
unused funds will be forfeited and will not be allowed to be returned.
• Employee can enroll in either or both FSAs only during the Open
Enrollment Period or New Hire Orientation.
• Money cannot be transferred between FSAs.
• Reimbursed expenses cannot be deducted for income tax purposes.
• Employee and dependent(s) cannot be reimbursed for services not
received.
• Employee and dependent(s) cannot receive insurance benets or any
other compensation for expenses reimbursed through an FSA.
• Domestic Partners are not eligible in the employee FSA as federal law
does not recognize them as a qualied dependent.
Filing a Claim
Claim Form
A completed claim form along with a copy of the receipt as proof of the
expense can be submitted by mail, fax, online or through the HealthEquity/
WageWorks mobile app. The IRS requires FSA participants to maintain complete
documentation, including copies of receipts for reimbursed expenses, for a
minimum of one (1) year.
Debit Card
FSA participants can request a debit card for payment of eligible expenses.
With the card, most qualied services and products can be paid at the point
of sale versus paying out-of-pocket and requesting reimbursement. The debit
card is accepted at a number of medical providers and facilities, and most
pharmacy retail outlets. HealthEquity/WageWorks may request supporting
documentation for expenses paid with a debit card. Failure to provide
supporting documentation when requested, may result in suspension of
the card and account until funds are substantiated or refunded back to
the District. This card will not expire at the end of the benet year. Please keep
the issued card for use next year. The debit card is only for medical expenses,
not dependent care.
HealthEquity/WageWorks
4609 Regent, Suite 100, Irving, TX 75063
Claims: help@wageworks.com
HERE’S HOW IT WORKS!
An employee earning $30,000 elects to place $1,000 into a Health
Care FSA. The payroll deduction is $38.46 based on a 26 pay period
schedule. As a result, health care expenses are paid with tax-free
dollars, giving the employee a tax savings of $197.
With a Health
Care FSA
Without a Health
Care FSA
Salary $30,000 $30,000
FSA Contribution - $1,000 - $0
Taxable Pay $29,000 $30,000
Estimated Tax
19.65% = 12% + 7.65% FICA
- $5,698 - $5,895
After Tax Expenses - $0 - $1,000
Spendable Income $23,302 $23,105
Tax Savings
$197
Please Note: Be conservative when estimating health care and/or dependent
care expenses. IRS regulations state that any unused funds remaining in an
FSA, after a plan year ends and after all claims have been led, cannot be
returned or carried forward to the next plan year. This rule is known as “use-
it or lose-it.”
Using a Smartphone or Mobile Device
With EZ Receipts mobile app from HealthEquity/WageWorks, employees
can file and manage reimbursement claims and receipts with a click of a
smartphone or mobile device camera, from anywhere.
Use EZ Receipts:
• Download the app from www.WageWorks.com, Apple App Store or
Google Play Store.
• Log into account.
• Choose the type of receipt from the simple menu.
• Enter required information regarding the transaction.
• Use a smartphone camera or device to capture the documentation.
• Submit the image and details to HealthEquity/WageWorks.
HealthEquity/WageWorks
Customer Service: (877) 924-3967 | www.WageWorks.com

19
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Employee Assistance Program
The District cares about their employees well being on and o the job and
provides all benet-eligible employees and each family member an Employee
Assistance Program (EAP) through Cigna at no cost.
What is an Employee Assistance Program?
An Employee Assistance Program oers covered employees and family
members free and convenient access to a range of condential and professional
services to help address a variety of problems that negatively aect well-being
such as:
9
Stress Management
9
Parenting Problems
9
Marital Problems
9
Relationship Issues
9
Substance Abuse
9
Critical Incident Debrieng
9
Child Care
9
Elder Care
9
Financial Services
How Do Employees Access EAP Benets?
The EAP provides up to six (6) counseling sessions per occurrence for short-
term problem resolution. Conditions that require long-term treatment may be
referred to employee's medical plan. The EAP also provides unlimited phone
consultation with an EAP professional available 24 hours a day, seven (7) days
a week at the customer service number given below.
Are Services Condential?
Yes. Receipt of EAP services are completely condential. If, however,
participation in the EAP is the direct result of a Management Referral (a
referral initiated by a supervisor or manager), we will ask permission to
communicate certain aspects of the employee’s care (attendance at sessions,
adherence to treatment plans, etc.) to the referring supervisor/manager. The
referring supervisor/manager will not receive specic information regarding
the referred employee’s case. The supervisor/manager will only receive reports
on whether the referred employee is complying with the prescribed treatment
plan.
To Access Services
Employee and family member(s) must register and create a user ID on
www.mycigna.com to access EAP services.
Cigna
Customer Service: (877) 622-4327 | www.mycigna.com
Employee ID: southoridawater
Basic Life and AD&D Insurance
Basic Term Life Insurance
The District provides benet-eligible employees, working a minimum of 25
hours per week, a Basic Term Life insurance benet through New York Life at
no cost to the employee as follows:
Regular Full-Time Employees
The Life insurance benet amount is equal to one (1) times the employee’s
annual salary rounded up to the nearest $1,000, to a maximum of
$200,000. Employees will be required to pay imputed income tax for
coverage over $50,000.
Managers/Select Exempt Service Employees
The Life Insurance benet amount is equal to two (2) times employee’s
annual salary rounded up to the nearest $1,000, to a maximum of
$400,000. Employees will be required to pay imputed income tax for
coverage over $50,000.
The Life insurance benet carries an Accelerated Living Benet. This allows an
employee to apply for a living benet if diagnosed with a terminal condition.
The amount of the term life insurance under the policy will be reduced by the
amount of living benet paid to you and by any administrative fees.
Accidental Death & Dismemberment Insurance
Also, at no cost to employee, The District provides Accidental Death &
Dismemberment (AD&D) insurance to eligible employees working a minimum
of 25 hours per week. The AD&D pays in addition to the Basic Term Life
insurance when a death occurs as a result of an accident. The AD&D benet
amount is equal to one (1) times the employee’s annual salary rounded up to
the nearest $1,000, to a maximum of $50,000.
Age Reduction Schedule
Benet amounts are subject to the following age reduction schedule:
› Reduces to 65% of the benet amount at age 65
› Reduces to 45% of the benet amount at age 70
› Reduces to 30% of the benet amount at age 75
› Reduces to 20% of the benet amount at age 80
Always remember to keep beneciary information
updated. Beneciary information may be updated
at anytime through Bentek.
New York Life Group Benet Solutions
Customer Service (800) 362-4462 | www.mynylgbs.com

20
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Voluntary Life Insurance
Voluntary Employee Life Insurance
Employees regularly working a minimum of 25 hours per week may elect to
purchase Voluntary Life insurance via payroll deduction through New York Life.
This Voluntary Life insurance may be purchased at dierent benet amounts
depending on eligibility classications. All employee classications also have
the option to purchase spouse and/or children at dierent levels.
New Hires may purchase Voluntary Employee Life insurance without being
subject to Medical Underwriting, also known as Evidence of Insurability
(EOI), up to the Guaranteed Issue amount of $350,000.
• Units can be purchased in increments of $10,000 to the lesser of ve (5)
times salary or $500,000.
• Benet amounts are subject to the following age reduction schedule:
› Reduces to 65% of the benet amount at age 65
› Reduces to 45% of the benet amount at age 70
› Reduces to 30% of the benet amount at age 75
› Reduces to 20% of the benet amount at age 80
• Calculate Bi-Weekly Premium Deduction:
Benet Amount ÷ $1,000 x Rate (See Table) x 12 ÷ 24 = Deduction
• 2024 Open Enrollment: Enrolled employees may increase coverage up
to but not exceeding the Guaranteed Issue amount of $350,000 without
being subject to Medical Underwriting, also known as Evidence of
Insurability (EOI). All others will need to complete an EOI. Please contact
Human Resources for additional information
Voluntary Spouse Life Insurance
New Hires may purchase Voluntary Spouse Life insurance without being
subject to Medical Underwriting, also known as Evidence of Insurability
(EOI), up to the Guaranteed Issue amount of $50,000.
• Employees must rst elect Voluntary Employee Life insurance in order to
purchase Voluntary Spouse Life coverage.
• Units can be purchased in increments of $5,000 not to exceed a maximum
of $250,000 or 100% of employee's Voluntary Life insurance amount.
• Rate is based on employee age.
• Benet amounts are subject to the voluntary employee life age reduction
schedule based on the employee's age.
• Calculate Bi-Weekly Premium Deduction:
Benet Amount ÷ $1,000 x Rate (See Table) x 12 ÷ 24 = Deduction
• 2024 Open Enrollment: Enrolled employees may increase coverage for
spouses up to but not exceeding the Guaranteed Issue amount of $50,000
without being subject to Medical Underwriting, also known as Evidence
of Insurability (EOI). All others will need to complete an EOI. Please
contact Human Resources for additional information.
Voluntary Employee and Spouse Life Rate Table
Age
Employee and Spouse
(Rate Per $1,000)
<20-34 $0.11
35-39 $0.12
40-44 $0.16
45-49 $0.26
50-54 $0.43
55-59 $0.72
60-64 $1.01
65-69 $1.73
70-99 $6.75
Voluntary Dependent Child(ren) Life Insurance
• Employee must rst elect Voluntary Employee Life insurance in order to
purchase Voluntary Dependent Child(ren) Life coverage.
• Coverage may be purchased for dependent child(ren) birth to six (6)
months in the amount of $500.
• Coverage may be purchased for dependent child(ren) age six (6) months
to 30 years in at benet amounts of $5,000, $10,000 or $25,000.
Voluntary Dependent Child(ren) Life Rate Table
Benet Amount
Bi-Weekly Premium
($0.15 Rate Per $1,000)
Monthly Premium
($0.30 Rate Per $1,000)
$5,000 $0.38 $0.75
$10,000 $0.75 $1.50
$25,000 $1.88 $3.75
Always remember to keep beneciary information
updated. Beneciary information may be updated
at anytime through Bentek.
New York Life Group Benet Solutions
Customer Service (800) 362-4462 | www.mynylgbs.com

21
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Voluntary Short Term Disability
The District oers Short Term Disability (STD) insurance through New York
Life to all benet-eligible employees working a minimum of 25 hours per
week. The STD benet pays employee a percentage of weekly base earnings if
employee becomes disabled due to an illness or non-work related injury.
Voluntary Short Term Disability (STD) Benets
• STD oers a benet of 60% of employee’s weekly pre-disability
earnings subject to a benet maximum of $1,500 per week.
• Employee must be disabled for 14 consecutive days due to illness
or a non-work related injury prior to becoming eligible for benets,
(known as the elimination period).
• Benet payments will commence on the 15th day of disability.
• Maximum benet period is 26 weeks (includes elimination period).
• Employee deemed unable to return to work after the STD 26-week
maximum period is exhausted, may be eligible to transition to Long
Term Disability (LTD) insurance.
• Benet may be reduced by other income.
• Disability benets may be taxable.
New York Life Group Benet Solutions
Customer Service (800) 362-4462 | www.mynylgbs.com
Long Term Disability
The District oers Core and Buy-up Long Term Disability (LTD) insurance
through New York Life to all benet-eligible employees working a minimum
of 25 hours per week. The LTD benet pays employee a percentage of monthly
earnings if employee becomes disabled due to an illness or injury.
Core Long Term Disability (LTD) Benets
• Eligible employee is automatically enrolled in this coverage at no cost to
the employee.
• LTD provides a benet of 60% of employee’s monthly pre-disability
earnings up to a benet maximum of $2,300 per month.
• Employee must be disabled for 180 days prior to becoming eligible for
the LTD benet (known as elimination period).
• Benet payments will commence on the 181st day of disability.
• Employee may continue to be eligible for partial benets if returning to
work on part-time basis.
• Benet may be reduced by other income.
• Maximum benet period depends on employee age at the time of
disability as shown below.
• Disability benets may be taxable.
Vountary Buy-Up Long Term Disability (LTD) Benets
• Buy-Up LTD is only oered to employee with a salary that exceeds $46,000.
• Provides a benet of 60% of employee’s monthly pre-disability earnings
up to a benet maximum of $7,500 per month.
• Employee must be disabled for 180 days prior to becoming eligible for
the LTD benet (known as elimination period).
• Benet payments will commence on the 181st day of disability.
• Employee may continue to be eligible for partial benets if returning to
work on part-time basis.
• Benet may be reduced by other income.
• Maximum benet period depends on employee age at the time of
disability as shown below.
• Disability benets may be taxable.
Please Note: The Buy-up option will require Evidence of Insurability (EOI) unless employee
enrolls within 31 days of eligibility or an annual salary increase in excess of $46,000.
Benet Duration Period
If disability occurs at age 62 or younger, the benet will continue to age 65 or
the date the 42nd monthly benet is payable, if later. Please see table below if
age of disability is above 63:
Age of Disability
63 64 65 66
67 68 69+
Number of Months Benets Paid
36 30 24 21 18 15 12
New York Life Group Benet Solutions
Customer Service (800) 362-4462 | www.mynylgbs.com

22
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Supplemental Insurance and Discounts
Trustmark
Trustmark oers a variety of voluntary supplemental insurance plans to full-time
benet-eligible employees. These may be purchased separately on a voluntary
basis and premiums paid by payroll deduction. Available plans include:
Accident Insurance Benet
Trustmark Accident Insurance is an aordable voluntary solution that helps
pay for unexpected health care expenses due to non-occupational accidents.
Accident insurance pays benets directly to the employee in addition to any
other coverage they have. Benets include initial care, injuries and follow-up
care of a covered accident. The plan is portable after employee’s rst payroll
deduction.
Accident Insurance also oers a Wellness Benet. A $100 benet is given to
oset the cost of going to the doctor for routine physicals, immunizations and
health screening tests, regardless of other coverage. The benet provides a
maximum of two (2) visits per person and a 60-day waiting period applies. To
inquire about eligible tests, please contact customer service.
Critical Illness Insurance
Critical Illness Insurance oered to employees through Trustmark provides a
benet ranging from $5,000 - $100,000. Funds are provided directly to the
covered person and can be used at their own discretion such as travel, room
and board, child care or treatment options not covered by traditional insurance.
The plan is portable after the rst payroll deduction.
Critical Illness Insurance also includes an Optional Health Screening Benet.
The cost of one (1) screening test per calendar year ($50 or $100 benet). To
inquire about a specic screening, please contact customer service.
Universal Life Insurance
Trustmark oers a variety of additional exible benets though Universal
Life Insurance for eligible employees and covered family members. This plan
complements any group term life insurance plan. The exible benets include,
death benet, LTC Living Benets and Interest-Earning Cash Value. This plan
comes with an EZ Value Plan option allowing for automatic increases in your
coverage annually on each of the rst ve (5) policy anniversaries. The increase
is equal to the amount of protection an additional $1.00 per week of deduction
would purchase.
Trustmark
New Enrollments
Customer Service: (888) 501-1280
Current Policy Holders
Customer Service: (800) 918-8877
Claims Phone: (877) 201-9373
www.TrustmarkVB.com
Legal Club
The District oers employees the opportunity to participate in a voluntary
pre-paid Family Protection Plan provided by Legal Club. By enrolling in this
plan, a participant will have direct access to attorneys who will provide legal
assistance, for a variety of situations including:
9
Free & Discounted Legal Care
9
Tax Preparation & Advice
9
Financial Education & Credit Counseling
9
Identity Theft Solutions
9
Life Events™ Counseling
This plan also oers identity theft protection to participants with consultations,
privacy and security monitoring, identity monitoring and restoration benets.
The cost to the employee to participate in this legal plan is $14 per month.
This includes coverage for the entire household including spouse, domestic
partners, dependent children and any dependent individual living in the
member’s home, such as a parent or grandparent, regardless of the number of
eligible dependents enrolled in the plan.
Free Membership
After six (6) continuous years of participation in Legal Club, members from
qualied groups will no longer be required to pay for access to free and
discounted LEGAL benets. Payroll deductions will continue at a signicantly
reduced rate so that member can access the other NON-LEGAL related services.
Legal - Family Protection Plan
Premium Payroll Deductions
Coverage
Employee
Bi-Weekly Premium
Employee
Monthly Premium
Family Protection Plan $7.00 $14.00
Legal Club
Customer Service: (800) 305-6816 | www.legalclub.com

23
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Supplemental Insurance and
Discounts (Continued)
Pet Benet Solutions
The District provides employees the opportunity to purchase Pet Benet
Solutions, a Veterinary Discount Plan, on a voluntary basis. Participating Pet
Benet Solutions providers oer a 25% savings on all in-house veterinary
medical care. This includes oce visit, exam, shots, surgery, x-rays and
more. Visit petassure.com/search for a complete list of local providers. Pet
Benet Solutions is not insurance, therefore there are no exclusions. An
employee can enroll any pet, any breed, any age and in any health condition;
including pets with pre-existing and hereditary conditions. Also, included at
no additional cost is ThePetTag, Pet Assure’s 24/7 Lost Pet Recovery Service.
ThePetTag that helps thousands of lost pets reunite with their families. The
Pet Assure Veterinary Discount Plan can be purchased for $9 per month,
regardless of how many covered pets.
Pet Discount Program
Premium Payroll Deductions
Coverage
Employee
Bi-Weekly Premium
Employee
Monthly Premium
Pet Benefit Solutions $4.50 $9.00
Pet Benet Solutions
Customer Service: (800) 891-2565 | www.petbenets.com/land/sfwmd
Florida Retirement System
Florida Retirement System (FRS)
The District participates in the Florida Retirement System (FRS) Plan for all full-
time employees working in regularly established positions. Positions that are
scheduled and budgeted as temporary or seasonal are not eligible.
Members are eligible for the Pension Plan benet with six (6) years of service
vesting if enrolled before July 1, 2011 or with 8 (eight) years of service vesting
if enrolled on or after July 1, 2011. Investment Plan members are vested after
one (1) year of service. One of the special features of membership in the FRS
is portability — the ability to keep the retirement credit when an employee
changes FRS employers. This means if an employee separates employment
with one (1) FRS employer, and later goes to work with any other FRS employer,
their service credit will be retained from their previous job and combined with
the new service credit. If you are employed in a regularly established position
(one (1) covered for retirement) on or after July 1, 2011, you must pay the three
(3) percent employee contribution unless you are participating in DROP or you
are re-employed retiree who is not eligible for renewed membership.
The monthly benet payment an employee receives when they retire depends
on their years of creditable service, retirement age, average nal compensation,
and the retirement plan options you select. The formula for calculating the
monthly benet will be provided upon enrollment by FRS.
Category
Enrollment* Date
Prior to July 1, 2011
Enrollment* Date
After July 1, 2011
Normal Retirement Criteria
30 years of FRS service
regardless of age
33 years of FRS service
regardless of age
Service Credit Age
Age 62 and 6 years of FRS
service
Age 65 and 8 years of
FRS service
Average Final Compensation
Average of the 5 highest
years of compensation
Average of the 8 highest
years of compensation
DROP Participation
Eligible upon meeting
normal retirement
criteria above
Eligible upon meeting
normal retirement
criteria above
DROP Interest Rate
6.5% interest paid on
DROP accounts annually
4% interest paid on
DROP accounts annually
*Enrollment is considered creditable service from any FRS employer.
FRS | Customer Service: (844) 377-1888 | www.myfrs.com

24
South Florida Water Management District
|
Employee Benet Highlights
|
2024
© 2016, Gehring Group, Inc., All Rights Reserved
Voluntary Retirement Plan
Fidelity Investments
The District oers a 457(b) Deferred Compensation savings plan through
Fidelity Investments.
457(b) Plan
Employees may set aside pre-tax dollars toward retirement savings
through automatic payroll deductions, which reduces taxes that
are paid out today. The money contributed to this type of account,
including earnings, accumulates on a tax-deferred basis. Withdrawals of
contributions and earnings are subject to Federal and State (if applicable)
income taxes in eect at the time of withdrawal.
Additional Benets:
1. Rollover eligible savings from a previous employer into this plan as
well as 401(k), 401(a), 403(b), 457(b) or IRAs.
2. Take a loan from the account with a minimum vested account balance
of $2,000, a loan can be requested for any reason for up to 50 percent
of the vested account balance.
3. A Roth post-tax payroll deduction investment option is also available,
please contact customer service for additional information.
2023 Limitations
457(b)
Annual Deferral Limit for 457 Plans $22,500
“Age 50” Catch-Up Limit
$7,500
($30,000 Total)
Please Note: These limits are set by the IRS and participants may adjust their contribution
amounts accordingly.
There is no employer matching for this program, and is subject to minimum
and maximum participation amounts. Employees can choose to contribute
to the 457(b) Deferred Compensation plan by contacting Fidelity customer
service or logging into Fidelity online.
Fidelity Investments
Customer Service: (800) 343-0860 | www.mydelitysite.com/SFWMD
Please Note: Be sure to maintain your list of beneciaries for each benet
that you choose. A separate list of beneciaries is required for every plan. For
example, each retirement plan and life insurance policy is separate.
Notes
Use this section to make notes regarding personal benet plans or to keep track
of important information such as doctors' names and addresses or prescription
medications.

FINAL
Last Modied: September 13, 2023 4:32 PM
3500 Kyoto Gardens Drive, Palm Beach Gardens, Florida 33410
Toll Free: (800) 244-3696
|
Fax: (561) 626-6970
|
www.gehringgroup.com
© 2016, Gehring Group, Inc., All Rights Reserved
