
Medicare Benefit Policy Manual
Chapter 16 - General Exclusions From Coverage
Table of Contents
(Rev. 198, 11-06-14)
Transmittals for Chapter 16
10 - General Exclusions from Coverage
20 - Services Not Reasonable and Necessary
30 - Foot Care
40 - No Legal Obligation to Pay for or Provide Services
40.1 - Indigence
40.2 – Provider, Physician, or Supplier Bills Only Insured Patients
40.3 - Medicare Patient Has Other Health Coverage
40.4 - Items Covered Under Warranty
40.5 - Members of Religious Orders
40.6 - Ambulance Services
50 - Items and Services Furnished, Paid for or Authorized by Governmental Entities -
Federal, State, or Local Governments
50.1 - Items and Services Which a Non-Federal Provider Furnishes Pursuant to an
Authorization Issued by a Federal Agency
50.1.1 - Veterans’ Administration (VA) Authorized Services
50.1.2 - Medicare Secondary Payment Where VA Authorizes Fewer Days
Than Total Number of Covered Days in the Stay
50.1.3 - Effect of VA Payments on Medicare Deductible and Utilization
50.1.4 - VA “Fee Basis Card"
50.1.5 - Services Authorized by Indian Health Service
50.2 - Items and Services Furnished by Federal Provider of Services or Federal
Agency
50.3 - Items or Services Paid for by Governmental Entity
50.3.1 - Application of Exclusion to State and Local Government Providers
50.3.2 - Application of Exclusion to Nongovernmental Providers,
Physicians and Suppliers
50.3.3 - Examples of Application of Government Entity Exclusion

50.4 - TRICARE and CHAMPVA (Civilian Health and Medical Program of
Veterans Administration)
50.5 - Active Duty Members of Uniformed Services
60 - Services Not Provided Within United States
70 - Services Resulting from War
80 - Personal Comfort Items
90 - Routine Services and Appliances
100 - Hearing Aids and Auditory Implants
110 - Custodial Care
110.1 - Custodial Care Under a Hospice Program
120 - Cosmetic Surgery
130 - Charges Imposed by Immediate Relatives of the Patient or Members of the
Patient’s Household
140 - Dental Services Exclusion
150 - Services Reimbursable Under Automobile, No Fault, Any Liability Insurance or
Workers’ Compensation
170 - Inpatient Hospital or SNF Services Not Delivered Directly or Under Arrangement
by the Provider
180 - Services Related to and Required as a Result of Services Which Are Not Covered
Under Medicare

10 - General Exclusions from Coverage
(Rev. 198, Issued: 11-06-14, Effective: 01-01-15, Implementation: 01-05-15)
No payment can be made under either the hospital insurance or supplementary medical
insurance program for certain items and services, when the following conditions exist:
• Not reasonable and necessary (§20);
• No legal obligation to pay for or provide (§40);
• Paid for by a governmental entity (§50);
• Not provided within United States (§60);
• Resulting from war (§70);
• Personal comfort (§80);
• Routine services and appliances (§90);
• Custodial care (§110);
• Cosmetic surgery (§120);
• Charges by immediate relatives or members of household (§130);
• Dental services (§140);
• Paid or expected to be paid under workers’ compensation (§150);
• Non-physician services provided to a hospital inpatient that were not provided
directly or arranged for by the hospital (§170);
• Services Related to and Required as a Result of Services Which are not Covered
Under Medicare (§180);
• Excluded foot care services and supportive devices for feet (§30); or,
• Excluded investigational devices (See Chapter 14).
20 - Services Not Reasonable and Necessary
(Rev. 1, 10-01-03)
A3-3151, HO-260.1, B3-2303, AB-00-52 - 6/00
Items and services which are not reasonable and necessary for the diagnosis or treatment
of illness or injury or to improve the functioning of a malformed body member are not
covered, e.g., payment cannot be made for the rental of a special hospital bed to be used

by the patient in their home unless it was a reasonable and necessary part of the patient’s
treatment. See also §80.
A health care item or service for the purpose of causing, or assisting to cause, the death of
any individual (assisted suicide) is not covered. This prohibition does not apply to the
provision of an item or service for the purpose of alleviating pain or discomfort, even if
such use may increase the risk of death, so long as the item or service is not furnished for
the specific purpose of causing death.
30 - Foot Care
(Rev. 1, 10-01-03)
Some foot care is excluded and some is covered. A description of both is in Chapter 15,
§290.
40 - No Legal Obligation to Pay for or Provide Services
(Rev. 1, 10-01-03)
A3-3152, HO-260.2, B3-2306
Program payment may not be made for items or services which neither the beneficiary
nor any other person or organization has a legal obligation to pay for or provide. This
exclusion applies where items and services are furnished gratuitously without regard to
the beneficiary’s ability to pay and without expectation of payment from any source, such
as free x-rays or immunizations provided by health organizations. However, Medicare
reimbursement is not precluded merely because a provider, physician, or supplier waives
the charge in the case of a particular patient or group or class of patients, as the waiver of
charges for some patients does not impair the right to charge others, including Medicare
patients. The determinative factor in applying this exclusion is the reason the particular
individual is not charged.
The following sections illustrate the applicability of this exclusion to various situations
involving services other than those paid for directly or indirectly by a governmental
entity. (For a discussion of the latter, see §50.)
40.1 - Indigence
(Rev. 1, 10-01-03)
A3-3152.A, HO-260.2.A
This exclusion does not apply where items and services are furnished to an indigent
individual without charge because of their inability to pay, if the provider, physician, or
supplier bills other patients to the extent that they are able to pay.
40.2 - Provider, Physician, or Supplier Bills Only Insured Patients
(Rev. 1, 10-01-03)
A3-3152.B, HO-260.2.B

Some providers, physicians, and suppliers waive their charges for individuals of limited
means, but they also expect to be paid where the patient has insurance which covers the
items or services they furnish. In such a situation, because it is clear that a patient would
be charged if insured, a legal obligation to pay exists and benefits are payable for services
rendered to patients with medical insurance if the provider, physician, or supplier
customarily bills all insured patients - not just Medicare patients - even though non-
insured patients are not charged.
Individuals with conditions which are the subject of a research project may receive
treatment financed by a private research foundation. The foundation may establish its
own clinic to study certain diseases or it may make grants to various other organizations.
In most cases, the patient is not expected to pay for treatment out-of-pocket, but if the
patient has insurance, the parties expect that the insurer will pay for the services. In this
situation, a legal obligation is considered to exist in the case of a Medicare patient even
though other patients may not have insurance and are not charged.
40.3 - Medicare Patient Has Other Health Coverage
(Rev. 1, 10-01-03)
A3-3152.C, HO-260.2.C
Payment is not precluded under Medicare if the patient is covered by another health
insurance plan or program, which is obligated to provide or pay for the same services.
However, Medicare does not pay until after the other payer has paid in the following
situations:
• Services covered by automobile medical or no-fault insurance;
• Services rendered during a specified period of up to 30 months to individuals
eligible or entitled solely on the basis of end stage renal disease (ESRD) who are
insured under an employer group health plan;
• Services rendered to individuals age 65 or over and spouses age 65 or over who
are insured under an employer group health plan by virtue of current employment
status;
• Services rendered to individuals under age 65 entitled to Medicare based on
disability and have large group health plan coverage based on the individual’s
current employment status or the current employment status of a family member;
and
• Services covered by workers’ compensation.
In these cases, the other plan pays primary benefits and if the other plan does not pay the
entire bill, secondary Medicare benefits may be payable. Medicare is also secondary to
the extent that a liability insurer has paid for services.

See the Medicare Secondary Payment (MSP) Manual, Pub. 100-05.
40.4 - Items Covered Under Warranty
(Rev. 1, 10-01-03)
A3-3152.D, HO-260.2.D
When defective equipment or a defective medical device is replaced under a warranty,
hospital or other provider services rendered by parties other than the warrantor are
covered despite the warrantor’s liability. However, see the Medicare MSP Manual (CMS
Pub. 100-05) for requirements for recovery under the liability insurance provisions.
With respect to payment for the device itself under cost reimbursement, the following
rules apply:
• If equipment or a device is replaced free of charge by the warrantor, no program
payment may be made, since there was no charge involved.
• If replacement equipment or device from another manufacturer had to be
substituted because the replacement offered under the warranty was not
acceptable to the beneficiary or the beneficiary’s physician, payment may be
made for the replaced device.
• If the warrantor supplied the replaced equipment or device, but some charge or a
pro rata payment was imposed, program payment may be made for the partial
payment imposed for the device furnished by the warrantor.
• If an acceptable replacement could have been obtained free of charge under a
warranty but the provider chose to purchase one instead, payment cannot be made
for the purchased device under the prudent buyer rules. (See Provider
Reimbursement Manual, Part 1, §2103.)
• If an acceptable replacement could have been purchased at a reduced price under
a warranty but the full price was paid to the original manufacturer or a new
replacement was purchased from a different manufacturer or other source,
coverage is limited to the amount that would have been paid under the warranty.
While payments to a hospital for inpatient services under the prospective payment system
(PPS) are not reduced to reflect collections under warranty provisions for medical
devices, cost-based reimbursed hospitals and exempt units are subject to the prudent
buyer rules.
40.5 - Members of Religious Orders
(Rev. 1, 10-01-03)
A3-3152.E, HO-260.2.E

A legal obligation to pay exists where a religious order either pays for or furnishes
services to members of the order. Although medical services furnished in such a setting
would not ordinarily be expressed in terms of a legal obligation, the order has an
obligation to care for its members who have rendered life-long services, similar to that
existing under an employer’s prepayment plan. Thus, payment may be made for such
services whether they are furnished by the order itself or by independent sources that
customarily charge for their services.
40.6 - Ambulance Services
(Rev. 1, 10-01-03)
B3-2306
There are numerous methods of financing ambulance companies. For example, some
volunteer organizations do not charge the patient or any other person but ask the recipient
of services for a donation to help offset the cost of the service. Although the recipients
may be under considerable moral and social pressure to donate, they are not required to
do so, and there is no enforceable legal obligation on the part of the individual or anyone
else to pay for the services. Thus, Medicare benefits would not be payable. However,
services of volunteer ambulance corps are not categorically excluded. Many such
companies regularly charge for their services and Medicare covers these services.
Some ambulance companies provide services without charge to residents of specific
geographical areas but charge non-residents to the extent they are able to pay (e.g.,
through private health insurance). Under those circumstances, the free services provided
the residents would be excluded from coverage, while the services furnished non-
residents would be covered.
Ambulance companies which charge membership fees generally do not charge additional
fees for services covered under the membership plan, although they may charge for
certain other services (e.g., additional trips or mileage). Services furnished by such
ambulance companies including services for which prepayment is made under the
membership plan, are considered to be services for which there is a legal obligation to
pay. Therefore, such services are reimbursable provided the ambulance company bills all
third party payers. Membership fees and insurance premiums are not incurred expenses
under Medicare (see the Medicare Benefit Policy Manual, Chapter 15, “Covered Medical
and Other Health Services,” §10) and are not reimbursable.
50 - Items and Services Furnished, Paid for or Authorized by
Governmental Entities - Federal, State, or Local Governments
(Rev. 1, 10-01-03)
A3-3153, HO-260.3, B3-2309
The law contains three separate exclusions applicable to items and services furnished,
paid for or authorized by governmental entities. In general, payment may not be made
for items and services:

• Furnished by a provider (Governmental or non governmental) or other person at
public expense pursuant to an authorization issued by a Federal agency (§50.1);
• Furnished by a provider of services or agency of the Federal government (§50.2);
and
• Paid for directly or indirectly by a Federal, State, or local governmental entity
(§50.3).
The A/B MAC (A) or (B) applies each of these exclusions separately, i.e., benefits are
excluded where any one of the exclusions applies.
50.1 - Items and Services Which a Non-Federal Provider Furnishes
Pursuant to an Authorization Issued by a Federal Agency
(Rev. 1, 10-01-03)
A3-3153.1, HO-260.3.B, B3-2309.2
50.1.1 - Veterans’ Administration (VA) Authorized Services
(Rev. 1, 10-01-03)
A3-3153.1.A, B3-2309.2, A3-3153.1.E, HO-260.3.B
Generally, an authorization issued by the Veterans’ Administration (VA) binds the VA to
pay in full for the items and services provided. No payment is made under Medicare for
such authorized services.
NOTE: Medicare can reimburse veterans for (or credit toward Medicare deductible or
coinsurance amounts) VA copayment amounts charged for VA authorized services
furnished by non-VA sources.
Medicare does not pay for any item or service rendered by a non-Federal provider
pursuant to an authorization issued by a Federal agency, under the terms of which the
Federal government agrees to pay for the services.
The VA may authorize non-Federal providers or private physicians or other suppliers to
render services at Federal expense. For example, the VA may pay for treatment of
veterans in non-VA hospitals for service connected disabilities and, in certain
circumstances, for nonservice-connected disabilities, provided the VA has given prior
authorization for the services. The VA may also agree to pay for emergency services
furnished a veteran who appears at a hospital without prior authorization, provided a
notification of the veteran’s admission and a request for authorization to provide care at
VA expense is submitted to the VA within 72 hours after the admission.
As a general rule, the VA does not authorize inpatient services at non-VA facilities for
treatment of nonservice-connected conditions. Accordingly, the A/B MAC (A) should
receive few, if any, requests for reimbursement for a VA copayment for treatment in a
non-VA provider. If a beneficiary requests reimbursement for the amount of the VA

copayment, the beneficiary must submit to the A/B MAC (A), along with their request,
VA Form 10-9014, Statement of Charges for Medical Care. These requests will be
handled on an ad hoc basis. For further guidance contact:
Centers for Medicare & Medicaid Services
Center for Medicare Management
Provider Billing Group
7500 Security Boulevard
Baltimore, Maryland 21244-1850
The VA may authorize up to six months of care in non-VA SNFs for veterans requiring
such care after transfer from a VA hospital. Services furnished pursuant to a VA
authorization do not count against the 100 days of extended care benefits available in a
benefit period. Where a veteran remains in a SNF until VA benefits are exhausted,
extended care benefits could begin under Medicare. Such benefits begin with the first
day after the VA benefits are exhausted, provided a physician certifies that the individual
still requires skilled nursing care on a continuing basis for a condition for which the
patient received inpatient hospital services or which arose while the patient was still
being treated in the facility for such a condition. The 3-day qualifying hospital stay and
30-day transfer requirements of the law must be met as of the time of entrance to the
facility.
Where an authorization from the VA was not given to the party rendering the services,
Medicare payment is not precluded even though the individual might have been entitled
to have payment made by the VA had they requested the authorization. Also, Medicare
secondary benefits may be payable where the VA authorizes fewer days than the total
number of covered days in the stay.
Generally it is advantageous for Medicare beneficiaries who are veterans to have items
and services paid for by the VA where possible, since in most cases the VA has no
deductible or coinsurance requirements. Also, services paid for in full by the VA do not
count against the individual’s maximum number of benefit days or visits available in a
Medicare benefit period.
However, the VA may charge veterans copayments for treatment of nonservice-
connected conditions (during periods of 90 days duration within a period of 365 days) if a
veteran’s income exceeds a specified amount (38 CFR Part 17). The VA may charge the
beneficiary a copayment for physician/supplier and outpatient services. The amount of
the copayment is equal to 20 percent of the estimated average cost (during the calendar
year in which the services are furnished) of an outpatient visit in a VA facility. The VA
determines the estimated average cost. The beneficiary pays the copayment amount
directly to the VA, i.e., the VA does not reduce its payments to physicians/suppliers or
for outpatient services. The total amount of a veteran’s copayment obligation for all
services received (inpatient and outpatient, authorized or furnished directly by the VA)
during any 90-day period within the 365-day period cannot exceed the amount of the
inpatient Medicare deductible in effect on the first day of the 365-day period. Medicare

pays secondary benefits to the beneficiary for VA copayment amounts in accordance with
§§50.1.4.
The charges for the following services are credited to the Medicare deductibles, on the
basis of Medicare fee schedule or allowable amounts, even though the Federal Agency
(VA) has not yet paid for them.
• Charges for services that exceed the VA copayment;
• Services rendered in a non-VA facility that are not authorized by the VA; or
• Services rendered after VA benefits are exhausted in a non-VA facility.
Crediting of VA payments to Medicare deductibles is handled in the same manner as the
crediting of employer group health plan payments. See Pub 100-05, the Medicare
Secondary Payer (MSP) Manual, Chapter 3, for billing and Chapter 5 for payment
instructions. Medicare can pay for such services where neither the physician/supplier nor
beneficiary has claimed benefits from the VA.
Medicare may also pay for (covered) services for which the VA does not make any
payment. For example, if a veteran is authorized “fee basis” care at VA expense for a
service connected back injury, and receives treatment for a different condition for which
the VA does not pay, Medicare can pay for the (covered) services that are not
reimbursable by the VA.
50.1.2 - Medicare Secondary Payment Where VA Authorizes Fewer
Days Than Total Number of Covered Days in the Stay
(Rev. 1, 10-01-03)
A3-3153.1.C, HO-260.3.B
The Medicare secondary payment is the lower of:
• The gross amount payable by Medicare for all covered days in the stay (without
regard to deductible or coinsurance) minus the amount paid by the VA for
Medicare covered services, or
• The gross amount payable by Medicare (without regard to deductible or
coinsurance) minus any applicable Medicare deductible or coinsurance.
EXAMPLE: The VA authorizes payment for 4 days of a 7-day stay. Charges for the 4
days total $2,350. The VA reimburses the hospital that amount. The gross amount
payable by Medicare (unreduced by deductible and coinsurance) for the 7-day stay is
$3,350. The beneficiary’s Part A deductible has not been met. The Medicare secondary
payment is determined by subtracting the VA payment from the gross amount payable by
Medicare: $3,350 - $2,350 = $1,000.

Medicare pays $1,000, which is less than the gross amount payable by Medicare minus
the Medicare deductible ($3,350 - $812 = $2,538). The beneficiary’s Part A deductible is
met by the VA payment.
50.1.3 - Effect of VA Payments on Medicare Deductible and Utilization
(Rev. 1, 10-01-03)
A3-3153.1.D, HO-260.3.B
Where an authorization issued by the VA binds the VA to pay in full for the items and
services, no payment may be made under Medicare. When the VA pays in full, the
services do not count against benefit maximums, e.g., the 90 days of inpatient hospital
services or the 60-day lifetime reserve. Charges which would be reimbursable by
Medicare except for the fact that the VA paid in full for authorized services may be
credited to the Medicare deductibles.
When the VA authorizes fewer days than the total number of covered days in the stay,
Medicare utilization is determined as follows:
• Divide the actual Medicare payment by the amount Medicare would have paid for
covered charges as primary payer (i.e., the gross amount payable by Medicare for
all covered days in the stay reduced by applicable Medicare deductible and
coinsurance).
• Multiply this percentage by the number of covered days in the stay.
A partial day resulting from this calculation is not charged as a full day if it is less than .5
of a day, but is charged as a full day if it is .5 or more of a day.
EXAMPLE: The following is the same facts as presented in example in §50.1.2. The
amount Medicare would pay, as a primary payer, is $2,538 ($3,350 - $812 deductible).
Utilization is determined as follows: $1,000 ÷ $2,538 =. 39 X 7 days = 2.75, rounded to
3 days.
When the VA pays an amount for Medicare covered services that is equal to, or less than,
the deductible and coinsurance that would apply if Medicare were the primary payer,
utilization is not reduced.
50.1.4 - VA “Fee Basis Card”
(Rev. 1, 10-01-03)
B3-2309.2
1. General
One method the VA uses to authorize physician services is to issue the veteran a “fee
basis ID card” (formally designated the VA Outpatient Medical Treatment Information
Card). This card is issued to certain veterans with a service connected disability, as well

as certain other veterans who require medical services for an extended period when VA
and other Federal health care facilities are not capable of furnishing economical care, or,
because of geographical inaccessibility, are not capable of furnishing the care or services
required. The card constitutes an agreement by the VA to pay up to a specified monthly
dollar amount for treatment of specific disabilities or for any condition specified on the
face of the card. The veteran is not restricted in choice of physician nor does the
physician selected by the veteran have to inform the VA in advance that they will be
treating the veteran. (The physicians are not participating physicians in the VA program
nor does the VA have an express “assignment” procedure.)
When the charges for the services exceed the specified monthly amount routinely allowed
by the VA, the VA may allow an additional amount if the physician justifies the need for
the additional cost. If justified, the VA will authorize an increase in the monthly dollar
limitation for a specific period of time. The VA may approve charges for services
exceeding the specified monthly amount retroactively if they were of the type that would
have been approved had they been submitted in advance.
2. VA Fee Basis Payment Is Payment in Full
When a physician accepts veterans as patients and bills the VA, the physician must
accept the VA’s “usual and customary” charge determination as payment in full. Neither
the patient nor any other party can be charged an additional amount. Except for the VA
copayment (see subsection 4(b)), Medicare cannot make payment on an assigned or
unassigned basis when the physician’s bill exceeds the amount the VA paid a physician
who has accepted the “Fee Basis” card. However, as indicated in subsection 4(a),
Medicare can pay for services that are not reimbursable by the VA. Therefore, the mere
existence of a “Y” trailer code indicating that the beneficiary has a VA fee card (as
discussed in subsection 5) is not sufficient to deny Medicare benefits. See subsection
4(a) for secondary Medicare benefits where the veteran bills the VA, and the VA
reimburses the beneficiary or physician less than the Medicare allowable amount.
3. Crediting Part B Deductible
Payments made by the VA for otherwise covered services are credited to the
beneficiary’s Part B deductible. (See subsection 5(c).)
4. Secondary Benefits
(a) Veteran Bills the VA
Where the physician does not accept the fee basis card (i.e., bills the veteran directly)
the veteran may file a claim with the VA. The VA may either reimburse the
beneficiary for out-of-pocket costs or pay the physician based on a claim filed by the
beneficiary. If the VA payment to the beneficiary or physician based on a claim filed
by the beneficiary is less than the Medicare fee schedule or allowable amount for the
services, Medicare can pay secondary benefits to supplement the VA payment,

provided the beneficiary submits a copy of the VA’s explanation of benefits which
accompanies the VA payment.
The VA explanation of benefits generally consists of a computer-generated notice,
which looks much like a punch card. It contains the beneficiary’s name and social
security number, the physician’s or supplier’s name, the month of service, and the
amount paid. (The VA plans to add the day of service to the notice.) The VA sends
this notice to the party that receives the payment (i.e., the beneficiary or the
physician/supplier). In some cases, the VA may also send a letter containing more
detailed information. If the A/B MAC (B) cannot determine from the VA notice the
amount the VA paid for particular services, it asks the physician or supplier to help it
match up the VA payment with specific services for which Medicare has been billed.
If the A/B MAC (B) is unable to obtain the help it needs from the physician or
supplier, it make reasonable assumptions about the relationship between the VA
payment and the services which have been billed to Medicare based on the
information available to it.
The Medicare secondary benefit amount, where the VA payment to the beneficiary or
physician is less than the allowable amount, is the lower of the following:
• The Medicare allowable amount minus applicable Medicare deductible
and coinsurance amounts; or
• The Medicare allowable amount minus the VA payment.
EXAMPLE: An individual who is authorized by the VA to receive physician services
for treatment of a nonservice-connected condition is issued a fee basis card. The
individual receives treatment from a physician who charges $135. The physician does
not accept the fee basis card. The individual bills the VA directly. The VA pays the
individual $82 ($96 fee basis rate minus $14 outpatient copayment). The Medicare
allowable amount for the service is $115. The individual’s unmet Part B deductible is
$75. The Medicare secondary benefit is the lower of:
• The Medicare allowable amount minus applicable deductible and
coinsurance amounts:
$115 - $75 = $40 X .80 = $32, or
• The Medicare allowable amount minus the VA payment:
$115 - $82 = $33.
The A/B MAC (B) pays $32, the lower of $32 or $33.
The beneficiary’s Part B deductible is considered met by the VA payment.

(b) Physician Bills the VA; VA Bills Beneficiary for Copayment
If a physician accepts the fee basis card and bills the VA, the VA payment is
considered payment in full. If the VA bills the beneficiary a copayment amount for
authorized physician/supplier services that are covered by Medicare in the absence of
the VA authorization, the A/B MAC (B) pays a secondary benefit to the beneficiary
consisting of the lower of the VA copayment amount or the amount Medicare would
pay in the absence of VA coverage (Medicare allowable amount minus applicable
deductible and coinsurance amounts).
EXAMPLE: A physician accepts fee basis reimbursement for services rendered.
The charges for the services are $96. The VA fee basis rate is $78. The VA pays the
physician $78 and charges the beneficiary a $14 copayment. The beneficiary claims
Medicare reimbursement for the VA copayment amount. The Medicare allowable
amount for the services is $83. The individual’s unmet Part B deductible is $75. The
Medicare secondary benefit is the lower of:
• Amount payable by Medicare in the absence of VA coverage:
$83 - $75 = $8 X .8 = $6.40, or
• Individual’s VA copayment obligation: $14.
The A/B MAC (B) pays $6.40.
The beneficiary’s deductible is credited with $75. If the beneficiary’s Part B
deductible had been met previously, the Medicare secondary payment would be $14,
the lower of:
• $66.40 ($83 X .8), or
• $14.
NOTE: Medicare may pay for covered outpatient emergency services furnished by a
VA hospital if there is a charge for the services. Medicare’s payment is subject to
applicable Part B Medicare deductible and coinsurance provisions. Accordingly,
there is no Medicare payment until the Part B deductible is met. However, any
charges to the beneficiary for covered VA hospital outpatient emergency services are
credited to the Medicare Part B deductible. The CMS, OMB, Division of
Accounting, which is responsible for processing claims for emergency services by
Federal providers, will ensure, in these cases, that pertinent data is entered into the
beneficiary’s Health Insurance Master Beneficiary Record.
5. Procedure
(a) Claim Is for Primary Medicare Benefits

When the A/B MAC (B) receives a Y trailer code (code 3) or a code 36, (type code
3), automatic notice from the Health Insurance Master File (which is sent in instances
where a Medicare beneficiary also has a VA fee basis card), it follows the instructions
in the Medicare Secondary Payer (MSP) Manual, Chapter 5, “Contractor Prepayment
Processing Requirements,” §20.3.1. It contacts the physician or supplier to ascertain
whether a claim has been, or will be submitted to the VA based on an authorization of
the VA or based on the fee basis card. If the physician responds that no claim has
been or will be submitted to the VA, the A/B MAC (B) pays the Medicare claim in
the usual manner. If the physician or supplier indicates that a claim has been or will
be submitted to the VA, the A/B MAC (B) denies the Medicare claim. If the
physician fails to respond to the A/B MAC (B)’s inquiry within 30 days, the A/B
MAC (B) denies the claim if the physician has accepted assignment on the grounds
that the physician refuses to furnish information necessary to determine the proper
Medicare payment. (The assignment agreement prohibits the physician from
charging the beneficiary in these cases because the basis for denial is failure to
furnish information, not noncoverage of services.) In unassigned cases, if the
physician fails to respond to the A/B MAC (B)’s inquiry within 30 days, the A/B
MAC (B) pays the Medicare claim in the usual manner. In accordance with a CMS-
VA agreement, no contacts are to be made with the beneficiary, unless the beneficiary
has submitted a claim for secondary Medicare benefits. Ordinarily, the A/B MAC
(B) does not contact the VA for information concerning actual or potential VA
payments; but if a VA facility offers to share such information with it, e.g.,
information about payments to beneficiaries or physicians or about VA authorized
services to beneficiaries, the A/B MAC (B) may work out arrangements with the
facility to receive such information on a periodic basis or on request.
(b) Claim Is for Secondary Medicare Benefits
If the information on the claim indicates that the VA has already paid benefits for the
services, but has not paid all of the charges, the Medicare A/B MAC (B) pays
Medicare secondary benefits in accordance with subsection 4(a) provided the VA
claim was filed by the beneficiary. If the beneficiary submits the VA’s computer
generated notice, the A/B MAC (B) assumes that the beneficiary filed the VA claim
and pays secondary benefits. If it is unclear whether the physician or beneficiary
submitted the VA notification, the A/B MAC (B) assumes that, in unassigned cases,
the beneficiary filed the VA claim and the A/B MAC (B) pays secondary benefits. In
assigned cases, the A/B MAC (B) asks the physician whether the physician or the
beneficiary filed the VA claim. Also, when it is clear that the physician submitted the
computer-generated notice, the A/B MAC (B) asks the physician (on both assigned
and unassigned claims) whether the physician or the beneficiary filed the claim with
the VA (since in either case the VA sends the notice to the physician who receives the
VA payment).
If the physician does not respond within 30 days, the A/B MAC (B) denies benefits,
in assigned cases, because of the physician’s refusal to furnish information necessary

to determine the proper Medicare payment. (The assignment agreement prohibits the
physician from charging the beneficiary in these cases because the basis for denial is
failure to furnish information, not noncoverage of services.) In unassigned cases, if
the physician does not respond within 30 days, the A/B MAC (B) assumes that the
beneficiary filed the VA claim and pays secondary benefits to the beneficiary.
(c) Claim Is for Reimbursement of VA Copayment Amounts or Crediting of
Medicare Deductible
Beneficiaries must attach to the Medicare claim form a copy of VA form 10-9014
(Statement of Charges for Medical Care) showing the VA copayment amount for
authorized services, when requesting Medicare payment toward that amount or in
order to have their Part B deductible credited.
50.1.5 - Services Authorized by Indian Health Service
(Rev. 1, 10-01-03)
A3-3153.1.B, HO-260.3A.2 B.3-2309.3
The Division of Indian Health of the United States Public Health Service authorizes
private physicians and privately owned hospitals and nursing homes to provide treatment
to Indians and their dependents under contractual arrangements with the Division of
Indian Health. In the case of such contract health services to Indians and their
dependents entitled under the Indian Health Service (IHS) program and Medicare,
Medicare is the primary payer and the IHS the secondary payer.
50.2 - Items and Services Furnished by Federal Provider of Services or
Federal Agency
(Rev. 1, 10-01-03)
A3-3153.2, HO-260.3.A, B3-2309.1
Generally, Federal providers are excluded from participation in the Medicare program.
However, Federal hospitals, like other nonparticipating hospitals, may be paid for
emergency inpatient and outpatient hospital services. Additionally, payment is precluded
for items and services rendered by a federally operated nonprovider, e.g., Veterans
Administration clinics. A provider or other facility acquired by the Department of
Housing and Urban Development (DHUD) in the administration of an FHA mortgage
insurance program is not considered to be a Federal provider or agency and this exclusion
is not applicable to services furnished by such facilities. The law provides exceptions to
this exclusion which permits the following categories of Federal providers to participate
in Medicare:
• Hospitals and SNFs of Indian Health Service; and
• A Federal provider which is determined to be providing services to the public
generally as a community institution or agency. VA hospitals which have sharing
agreements with non-VA participating hospitals under which the VA hospitals

furnish end-stage renal disease (ESRD) services to nonveterans may be
considered community hospitals with respect to any otherwise covered service
rendered to ESRD beneficiaries. This exception does not apply to Federal clinics
or other Federal health facilities which are not “providers of services” as defined
in the Medicare law, i.e., which are not hospitals, SNFs, HHAs or CORFs. The
CMS is responsible for processing claims for services furnished directly by
Federal providers. If the A/B MAC (A) were to receive a request for Medicare
reimbursement of such services it would forward the request to:
Centers for Medicare & Medicaid Services
Office of Financial Management
P.O. Box 17255
Baltimore, Maryland 21203-7255
NOTE: The VA copayment provisions mentioned in §50.1.1 also applies to inpatient
services furnished in a VA hospital. Should the A/B MAC (A) receive a request for
Medicare reimbursement of VA copayment amounts for emergency services furnished by
VA hospitals, it would refer the request to CMS.
50.3 - Items or Services Paid for by Governmental Entity
(Rev. 1, 10-01-03)
A3-3153.3, HO-260.3.C, B3-2309.4
Medicare payment may not be made for items or services paid for directly or indirectly
by a Federal, State or local governmental entity. However, the law specifies that this
exclusion does not prohibit payment for:
• Items or services furnished under a health benefits or insurance plan established
for employees of the governmental entity;
• Items or services furnished under one of the titles of the Social Security Act (such
as medical assistance under title XIX); or
• Rural health clinic services.
50.3.1 - Application of Exclusion to State and Local Government
Providers
(Rev. 1, 10-01-03)
A3-3153.3.A, HO-260.3.C
Except for the two categories of facilities referred to below, payment may not be made
for items and services which a State or local government facility furnishes free of charge,
i.e., without expectation of payment from any source and without regard to the
individuals’ ability to pay. A facility which reduces or waives its charges for patients
unable to pay, or charges patients only to the extent of their Medicare and other health

insurance coverage, is not viewed as furnishing free services and may therefore receive
program payment.
Medicare regulations permit payment to the following two categories of governmental
providers even though they furnish services free of charge:
• Payment may be made for items and services furnished in or by a participating
State or local Government hospital, including a psychiatric or tuberculosis
hospital, which serves the general community. A psychiatric hospital to which
patients convicted of crimes are committed involuntarily is considered to be
serving the general community if State law provides for voluntary commitment to
the institution. However, payment may not be made for services furnished in or
by State or local hospitals, which serve only a special category of the population,
but do not serve the general community, e.g., prison hospitals.
• Payment may be made for items and services paid for by a State or local
governmental entity and furnished an individual as a means of controlling
infectious diseases or because the individual is medically indigent.
50.3.2 - Application of Exclusion to Nongovernmental Providers,
Physicians and Suppliers
(Rev. 1, 10-01-03)
A3-3153.3.B, HO-260.3.D, B3-2309.4
Payment may not be made for items or services furnished by a nongovernmental
provider, physician or supplier if the charges have been paid for by a government
program other than Medicare, or if the provider, physician, or supplier intends to look to
another government program for payment, unless the payment by the other program is
limited to the Medicare deductible and coinsurance amounts, as it is for certain
individuals covered under TRICARE/CHAMPVA. (See §50.4).
The mere fact that a nongovernmental provider receives government financing does not
mean that the items and services it furnishes are considered paid for by a governmental
entity. However, if a clinic receives government financing earmarked for particular
services to patients (e.g., in the form of a research grant), Medicare may not pay for the
same services.
If an individual has the option of receiving care free of charge at a government provider
or care which is not free at a nongovernment provider, and the individual, chooses the
latter, Medicare payment may be made for the care at the nongovernment provider.
However, items and services authorized by a Federal agency (for example, by the VA at a
nongovernmental hospital) are excluded. (See §50.3.3, below.)
50.3.3 - Examples of Application of Government Entity Exclusion
(Rev. 122, Issued: 04-09-10, Effective/Implementation Date: 07-09-10)

The following paragraphs explain the application of the governmental entity exclusion to
various situations involving services rendered by governmental and non governmental
facilities:
1. State Veterans Homes
Many State governments operate veterans homes and hospitals. These institutions are
generally open only to veterans and certain dependents of veterans, and include
domiciliary, hospital, infirmary, and/or nursing home type facilities. These institutions
are financed primarily from State funds; in addition, most receive nominal per diem
payments from the VA for domiciliary care, hospital care, or nursing home type care for
each veteran who would also qualify for admission to a VA hospital or domiciliary.
When such a participating institution charges its residents and patients to the extent of
their ability to pay, or seeks payment from available sources other than Medicare,
benefits are payable for covered items and services furnished to Medicare beneficiaries.
However, if it is the policy of the institution to admit and treat a veteran without charge
simply because the individual is a veteran, or because the condition is service-connected,
payment would be precluded under title XVIII.
Per diem amounts paid by the VA to State veterans homes on behalf of those patients
who are otherwise eligible for care in a VA facility may be credited towards any
deductible, coinsurance, or noncovered amounts required to be paid by the patient.
However, if a State veterans home collects amounts from the VA in excess of the
applicable deductible and coinsurance, the A/B MAC (A) reduces the Medicare payment
to the extent of such payments.
2. State and Local Psychiatric Hospitals
In general, payment may be made under Medicare for covered services furnished without
charge by State or local psychiatric hospitals which serve the general community. (See
§50.3.1.) However, payment may not be made for services furnished without charge to
individuals who have been committed under a penal statute (e.g., defective delinquents,
persons found not guilty by reason of insanity, and persons incompetent to stand trial).
For Medicare purposes such individuals are “prisoners,” as defined in subsection 3, and
may have services paid by Medicare only under the exceptional circumstances described
there.
A psychiatric hospital to which patients convicted of crimes are committed is considered
to be serving the general community if State law also provides for voluntary admissions
to the institution.
3. Prisoners
The regulation at 42 CFR §411.4(b) states:

“Individuals who are in custody include, but are not limited to, individuals who are
under arrest, incarcerated, imprisoned, escaped from confinement, under supervised
release, on medical furlough, required to reside in mental health facilities, required to
reside in halfway houses, required to live under home detention, or confined completely
or partially in any way under a penal statute or rule.”
Moreover, 72 FR 47405 states further that the—
“…definition of “custody” is in accordance with how custody is defined by Federal
courts for purposes of the habeas corpus protections of the Constitution. For example,
the term “custody” is not limited solely to physical confinement. (Sanders v. Freeman,
221F.3d 846, 850-851 (6
th
Cir. 2000).) Individuals on parole, probation, bail, or
supervised release may be “in custody.”
42 CFR §411.4(b) goes on to describe the special conditions that must be met in order for
Medicare to make payment for individuals who are in custody, 42 CFR §411.4(b) states:
“Payment may be made for services furnished to individuals or groups of
individuals who are in the custody of the police or other penal authorities or in the
custody of a government agency under a penal statute only if the following
conditions are met:
1. State or local law requires those individuals or groups of individuals to repay the
cost of medical services they receive while in custody, and
2. The State or local government entity enforces the requirement to pay by billing all
such individuals, whether or not covered by Medicare or any other health
insurance, and by pursuing the collection of the amounts they owe in the same
way and with the same vigor that it pursues the collection of other debts."
The CMS presumes that a state or local government that has custody of a Medicare
beneficiary under a penal statute has a financial obligation to pay for the cost of
healthcare items and services unless the State can demonstrate to the A/B MAC (A)’s,
(B)’s, or (HHH)’s, or DME MAC’s satisfaction, in consultation with the RO, that:
• State or local law requires that individuals in custody repay the cost of the
services.
• The State or local government entity enforces the requirement to pay by billing
and seeking collection from all individuals in custody with the same legal status
(e.g., not guilty by reason of insanity), whether insured or uninsured, and by
pursuing collection of the amounts they owe in the same way and with the same
vigor that it pursues the collection of other debts. This includes collection of any
Medicare deductible and coinsurance amounts and the cost of items and services
not covered by Medicare.

NOTE: The A/B MAC (A), (B), or (HHH), or DME MAC will require evidence that
routine collection efforts include the filing of lawsuits to obtain liens against
individuals’ assets outside the prison and income derived from non-prison sources.
• The State or local entity documents its case with copies of regulations, manual
instructions, directives, etc., spelling out the rules and procedures for billing and
collecting amounts paid for prisoners’ medical expenses. As a rule, the A/B
MAC (A), (B), or (HHH), or DME MAC will inspect a representative sample of
cases in which prisoners have been billed and payment pursued, randomly
selected from both Medicare and non-Medicare eligible. The existence of cases
in which the State or local entity did not actually pursue collection, even though
there is no indication that the effort would have been unproductive, indicates that
the requirement to pay is not enforced.
The CMS maintains a file of incarcerated beneficiaries, obtained from SSA, that is used
to edit claims.
Providers and suppliers that render services or items to a prisoner or patient in a
jurisdiction that meets the conditions described above indicate this fact with the use of a
modifier (for A/B MAC (B) processed claims) or condition code (for A/B MAC (A)
processed claims). Otherwise the claims are denied.
4. Health Department Outpatient Clinics
Services rendered free of charge by State and local health department outpatient clinics
are not covered unless the services are rendered because of the individual’s indigence or
as a means of controlling infectious diseases. Thus, services rendered by city-operated
clinics for the poor and clinics for the detection and treatment of such illnesses as
venereal disease and tuberculosis are not excluded from Medicare coverage.
5. Vocational Rehabilitation (VR) Agencies
Under the vocational rehabilitation (VR) programs of the various States, vocational
training and services, including hospital and medical care, are provided to handicapped
persons who qualify under State law. These programs are financed in part by a Federal
matching fund program set up under the Vocational Rehabilitation Act.
When items or services are furnished by a State VR agency, title XVIII benefits are
payable if the agency charges all clients for its services or makes services available
without cost only to medically indigent individuals. If a rehabilitation agency has paid for
items and services furnished by nonproviders (e.g., physicians’ services and prosthetic
appliances), it may claim the Part B payment due the beneficiary if the latter has
authorized it to do so. The procedure is similar to that provided for State welfare
agencies; the State vocational rehabilitation agency function is comparable to that of a
State welfare agency in relation to a welfare recipient.

50.4 - TRICARE and CHAMPVA (Civilian Health and Medical
Program of Veterans Administration)
(Rev. 1, 10-01-03)
A3-3153.3.D, HO-260.3.F
1. General
TRICARE and CHAMPVA are similar programs administered by the Department of
Defense, except that the Veterans Administration determines the eligibility of persons
seeking to establish entitlement to CHAMPVA coverage. TRICARE provides benefits
for health care services furnished by civilian providers, physicians, and suppliers to
retired members of the Uniformed Services and to spouses and children of active duty,
retired, and deceased members. The term “Uniformed Services” includes the Army,
Navy, Air Force, Marine Corps, Coast Guard, and the Commissioned Corps of the U.S.
Public Health Service and of the National Oceanic and Atmospheric Administration.
CHAMPVA provides similar benefits for spouses and children of veterans who are
entitled to VA permanent and total disability benefits and to widows and children of
veterans who died of service-connected disabilities.
The governmental entity exclusion does not preclude Medicare payment for items or
services furnished to a beneficiary who is also eligible for TRICARE/CHAMPVA benefit
payments for the same services. Medicare is the primary payer for such items and
services, and TRICARE/CHAMPVA is a supplementary payer. (See subsection 3,
below.)
2. Effect of Medicare Eligibility on TRICARE/CHAMPVA Entitlement
TRICARE/CHAMPVA beneficiaries, other than dependents of active duty members, lose
their entitlement to TRICARE/CHAMPVA if they qualify for Medicare Part A on any
basis and do not enroll in Medicare Part B (effective October 1, 2001).
NOTE: TRICARE beneficiaries that turned age 65 prior to April 1, 2001 are not
required to purchase Medicare Part B in order to retain their TRICARE Pharmacy
benefits. However, all TRICARE individuals entitled to Medicare Part A must be
enrolled in Medicare Part B to receive the rest of their TRICARE benefit.
Individuals who are eligible for Medicare Part B benefits only, do not lose their
entitlement to TRICARE/CHAMPVA benefits. If a Medicare beneficiary, who has lost
entitlement to CHAMPVA upon becoming entitled to Part A of Medicare, thereafter
exhausts any Part A benefits, the individual can again be entitled to CHAMPVA. Once
the individual re-attains CHAMPVA benefits, the individual will not lose them by virtue
of later again becoming eligible for Medicare Part A benefits. There is no similar
provision for TRICARE which enables an individual to re-attain TRICARE eligibility
after exhausting Medicare Part A benefits. A/B MACs (A) and (B) will direct questions
concerning this provision to the CHAMPVA Center.

3. Medicare-TRICARE/CHAMPVA Relationship
If a TRICARE/CHAMPVA beneficiary also has Medicare coverage, TRICARE/
CHAMPVA reduces its liability in all cases by the amount payable by Medicare, i.e.,
Medicare is the primary payer and TRICARE/CHAMPVA supplements Medicare by
paying the Medicare deductible and coinsurance amounts and portions of the bill not
covered by Medicare. Thus, dually entitled individuals may be reimbursed up to 100
percent of expenses for items and services covered by both programs.
TRICARE/CHAMPVA has established policies and procedures which provide for (a) the
identification of claimants who have coverage under both TRICARE/CHAMPVA and
Medicare and (b) the detection of duplicate payments under both programs. If
TRICARE/CHAMPVA inadvertently pays amounts which duplicate Medicare payments
for the same items or services, TRICARE/CHAMPVA will take steps to recover the
incorrect TRICARE/CHAMPVA payments.
50.5 - Active Duty Members of Uniformed Services
(Rev. 1, 10-01-03)
A3-3153.3.E, HO-260.3.G
In limited circumstances, active duty members of the Uniformed Services may have care
in civilian facilities paid for by the Army, Navy, Air Force, Marine Corps, or other
appropriate uniformed service. Except for emergency services, prior approval is
generally required before such payment can be made. Services furnished pursuant to
such approval and services paid for or expected to be paid for by the Uniformed Services
are not reimbursable under Medicare.
60 - Services Not Provided Within United States
(Rev. 102; Issued: 02-13-09; Effective/Implementation Date: 03-13-09)
Items and services furnished outside the United States are excluded from coverage except
for the following services, and certain services rendered on board a ship:
• Emergency inpatient hospital services where the emergency occurred:
o While the beneficiary was physically present in the United States; or
o In Canada while the beneficiary was traveling without reasonable delay and
by the most direct route between Alaska and another State. See Pub. 100-04,
Medicare Claims Processing Manual Chapter 3, Inpatient Hospital Billing,
Section 110 for a description of claims processing procedures.
• Emergency or nonemergency inpatient hospital services furnished by a hospital
located outside the United States, if the hospital was closer to, or substantially
more accessible from, the beneficiary’s United States residence than the nearest
participating United States hospital which was adequately equipped to deal with

and available to provide treatment of the illness or injury (see Pub. 100-04,
Medicare Claims Processing Manual Chapter 3, Inpatient Hospital Billing,
Section 110 for a description of claims processing procedures);
• Physician and ambulance services furnished in connection with a covered foreign
hospitalization. Program payment may not be made for any other Part B medical
and other health services, including outpatient services furnished outside the
United States (see Pub. 100-04, Medicare Claims Processing Manual Chapter 1,
General Billing Requirements, Section 10.1.4.1 for a description of claims
processing procedures);
• Services rendered on board a ship in a United States port, or within 6 hours of
when the ship arrived at, or departed from, a United States port, are considered to
have been furnished in United States territorial waters. Services not furnished in a
United States port, or within 6 hours of when the ship arrived at, or departed from,
a United States port, are considered to have been furnished outside United States
territorial waters, even if the ship is of United States registry (see Pub. 100-04,
Medicare Claims Processing Manual Chapter 1, General Billing Requirements,
Section 10.1.4.7 for a description of claims processing procedures); and
The term “United States” means the 50 States, the District of Columbia, the
Commonwealth of Puerto Rico, the Virgin Islands, Guam, the Northern Mariana Islands,
American Samoa and, for purposes of services rendered on a ship, includes the territorial
waters adjoining the land areas of the United States.
A hospital that is not physically situated in one of the above jurisdictions is considered to
be outside the United States, even if it is owned or operated by the United States
Government.
Payment may not be made for any item provided or delivered to the beneficiary outside
the United States, even though the beneficiary may have contracted to purchase the item
while they were within the United States or purchased the item from an American firm.
Payment may not be made for a medical service (or a portion of it) that was
subcontracted to another provider or supplier located outside the United States. For
example, if a radiologist who practices in India analyzes imaging tests that were
performed on a beneficiary in the United States, Medicare would not pay the radiologist
or the U.S. facility that performed the imaging test for any of the services that were
performed by the radiologist in India.
Under the Railroad Retirement Act, payment is made to Qualified Railroad Retirement
beneficiaries (QRRBs) by the RRB for covered hospital services furnished in Canadian
hospitals as well as in the U.S. Physician and ambulance services are not covered by the
Railroad Retirement Act; however, under an agreement between CMS and RRB, if the
QRRB claims payment for Part B services in connection with Canadian hospitalization,
RRB processes the Part B claim. In such cases the RRB determines:

• Whether the requirements are met for the inpatient services; and
• Whether the physician and/or ambulance services were furnished in connection
with the services.
Services for an individual who has elected religious nonmedical health care status may be
covered if the above requirements are met but this revokes the religious nonmedical
health care institution election.
70 - Services Resulting from War
(Rev. 1, 10-01-03)
A3-3155, HO-260.5, B3-2315
Items and services which are required as a result of war, or of an act of war, occurring
after the effective date of the patient’s current entitlement date are not covered.
80 - Personal Comfort Items
(Rev. 1, 10-01-03)
A3-3156, HO-260.6, B3-2318
Items that do not contribute meaningfully to the treatment of an illness or injury or the
functioning of a malformed body member are not covered.
Charges for special items requested by the patient such as radio, television, telephone,
and air conditioner, and beauty and barber services are excluded from coverage. The
patient may be charged for such a service if they requested it with knowledge that they
will be charged. To avoid misunderstanding and disputes, the provider informs the
individual upon request for such an item or service that there is a specified charge (not
exceeding the customary charge). Thereafter, the provider may not charge the patient
more for the item or service than the charge specified. A provider may not require a
beneficiary to request noncovered items or services as a condition of admission or of
continued stay.
Basic personal services such as simple barber and beautician services (e.g., shaves,
haircuts, shampoos, and simple hair sets) which patients need and cannot perform for
themselves may be viewed as ordinary patient care when furnished by a long-stay
institution. Such services are covered costs reimbursable under Part A when included in
the flat rate charge and provided routinely without charge to the patient by an SNF or by
a general psychiatric or tuberculosis hospital. The services are maintenance of at least a
minimum level of personal hygiene, decency, and presentability items essential to the
well-being of the patient and of other patients who must associate with the patient.
However, under the personal comfort exclusion, more elaborate services, such as
professional manicures, hair styling, etc., are excluded even when furnished routinely and
without special charge.

90 - Routine Services and Appliances
(Rev. 186, Issued: 04-16-14, Effective: 01-01 01, Implementation: 05-12-14)
Routine physical checkups; eyeglasses, contact lenses, and eye examinations for the
purpose of prescribing, fitting, or changing eyeglasses; eye refractions by whatever
practitioner and for whatever purpose performed; hearing aids and examinations for
hearing aids; and immunizations are not covered.
The routine physical checkup exclusion applies to (a) examinations performed without
relationship to treatment or diagnosis for a specific illness, symptom, complaint, or
injury; and (b) examinations required by third parties such as insurance companies,
business establishments, or Government agencies.
The routine physical checkup exclusion does not apply to the following services (as noted
in section 42 CFR 411.15(a)(1)):
• Screening mammography,
• Colorectal cancer screening tests,
• Screening pelvic exams,
• Prostate cancer screening tests,
• Glaucoma screening exams,
• Ultrasound screening for abdominal aortic aneurysms (AAA),
• cardiovascular disease screening tests,
• diabetes screening tests,
• screening electrocardiogram,
• Initial preventive physical examinations,
• Annual wellness visits providing personalized prevention plan services, and
• Additional preventive services that meet the criteria specified in 42 CFR 410.64.
If the claim is for a diagnostic test or examination performed solely for the purpose of
establishing a claim under title IV of Public Law 91-173, “Black Lung Benefits,” the
service is not covered under Medicare and the claimant should be advised to contact their
Social Security office regarding the filing of a claim for reimbursement under the “Black
Lung” program.
The exclusions apply to eyeglasses or contact lenses, and eye examinations for the
purpose of prescribing, fitting, or changing eyeglasses or contact lenses for refractive
errors. The exclusions do not apply to physicians’ services (and services incident to a
physicians’ service) performed in conjunction with an eye disease, as for example,
glaucoma or cataracts, or to post-surgical prosthetic lenses which are customarily used
during convalescence from eye surgery in which the lens of the eye was removed, or to
permanent prosthetic lenses required by an individual lacking the organic lens of the eye,
whether by surgical removal or congenital disease. Such prosthetic lens is a replacement
for an internal body organ - the lens of the eye. (See the Medicare Benefit Policy
Manual, Chapter 15, “Covered Medical and Other Health Services,” §120).

Expenses for all refractive procedures, whether performed by an ophthalmologist (or any
other physician) or an optometrist and without regard to the reason for performance of the
refraction, are excluded from coverage.
A. Immunizations
Vaccinations or inoculations are excluded as immunizations unless they are either:
• Directly related to the treatment of an injury or direct exposure to a disease or
condition, such as antirabies treatment, tetanus antitoxin or booster vaccine,
botulin antitoxin, antivenin sera, or immune globulin. (In the absence of injury or
direct exposure, preventive immunization (vaccination or inoculation) against
such diseases as smallpox, polio, diphtheria, etc., is not covered.); or
• Specifically covered by statute, as described in the Medicare Benefit Policy
Manual, Chapter 15, “Covered Medical and Other Health Services,” §50.4.4.2.
B. Antigens
Prior to the Omnibus Reconciliation Act of 1980, a physician who prepared an antigen
for a patient could not be reimbursed for that service unless the physician also
administered the antigen to the patient. Effective January 1, 1981, payment may be made
for a reasonable supply of antigens that have been prepared for a particular patient even
though they have not been administered to the patient by the same physician who
prepared them if:
• The antigens are prepared by a physician who is a doctor of medicine or
osteopathy, and
• The physician who prepared the antigens has examined the patient and has
determined a plan of treatment and a dosage regimen.
A reasonable supply of antigens is considered to be not more than a 12-month supply of
antigens that has been prepared for a particular patient at any one time. The purpose of
the reasonable supply limitation is to assure that the antigens retain their potency and
effectiveness over the period in which they are to be administered to the patient. (See the
Medicare Benefit Policy Manual, Chapter 15, “Covered Medical and Other Health
Services,” §50.4.4.1)
100 - Hearing Aids and Auditory Implants
(Rev. 39; Issued: 11-10-05; Effective: 11-10-05; Implementation: 12-12-05)
Section 1862(a)(7) of the Social Security Act states that no payment may be made under
part A or part B for any expenses incurred for items or services “where such expenses are
for . . . hearing aids or examinations therefore. . . .” This policy is further reiterated at

42 CFR 411.15(d) which specifically states that “hearing aids or examination for the
purpose of prescribing, fitting, or changing hearing aids” are excluded from coverage.
Hearing aids are amplifying devices that compensate for impaired hearing. Hearing aids
include air conduction devices that provide acoustic energy to the cochlea via stimulation
of the tympanic membrane with amplified sound. They also include bone conduction
devices that provide mechanical energy to the cochlea via stimulation of the scalp with
amplified mechanical vibration or by direct contact with the tympanic membrane or
middle ear ossicles.
Certain devices that produce perception of sound by replacing the function of the middle
ear, cochlea or auditory nerve are payable by Medicare as prosthetic devices. These
devices are indicated only when hearing aids are medically inappropriate or cannot be
utilized due to congenital malformations, chronic disease, severe sensorineural hearing
loss or surgery.
The following are prosthetic devices:
• Cochlear implants and auditory brainstem implants, i.e., devices that replace the
function of cochlear structures or auditory nerve and provide electrical energy to
auditory nerve fibers and other neural tissue via implanted electrode arrays.
• Osseointegrated implants, i.e., devices implanted in the skull that replace the
function of the middle ear and provide mechanical energy to the cochlea via a
mechanical transducer.
Medicare contractors deny payment for an item or service that is associated with any
hearing aid as defined above. See §180 for policy for the medically necessary treatment
of complications of implantable hearing aids, such as medically necessary removals of
implantable hearing aids due to infection.
110 - Custodial Care
(Rev. 1, 10-01-03)
A3-3159, HO-260.10, HO-261, B3-2326
Custodial care is excluded from coverage. Custodial care serves to assist an individual in
the activities of daily living, such as assistance in walking, getting in and out of bed,
bathing, dressing, feeding, and using the toilet, preparation of special diets, and
supervision of medication that usually can be self-administered. Custodial care
essentially is personal care that does not require the continuing attention of trained
medical or paramedical personnel. In determining whether a person is receiving
custodial care, the A/B MAC (A) or (B) considers the level of care and medical
supervision required and furnished. It does not base the decision on diagnosis, type of
condition, degree of functional limitation, or rehabilitation potential.

Institutional care that is below the level of care covered in a SNF is custodial care. (See
the Medicare Benefit Policy Manual, Chapter 8, “Coverage of Extended Care (SNF)
Services Under Hospital Insurance,” §30.) Some examples of custodial care in hospitals
and SNFs are:
• A stroke patient who is ambulatory, has no bladder or bowel involvement, no
serious associated or secondary illnesses and does not require medical or
paramedical care but requires only the assistance of an aide in feeding, dressing,
and bathing;
• A cardiac patient who is stable and compensated and has reasonable cardiac
reserve and no associated illnesses, but who because of advanced age has
difficulty in managing alone in the home, and requires assistance in meeting the
activities of daily living; and
• A senile patient who has diabetes which remains stabilized as long as someone
sees to it that the patient takes oral medication and sticks to a prescribed diet.
Even if a patient’s stay in a hospital or SNF is determined to be custodial, some
individual services may still be covered under Part B if they are reasonable and
necessary. For example, periodic visits by a physician to their patient are covered under
Part B if such services are reasonable and necessary to the treatment of the patient’s
illness or injury even though a finding has been made that the care being furnished the
patient in the hospital or SNF is custodial care and, therefore, not covered. Similarly,
such a finding of custodial care does not preclude payment for a Part B claim for
ancillary services, which are medically necessary (see the Medicare Benefit Policy
Manual, Chapter 15, “Covered Medical and Other Health Services,” §250). (See the
Medicare Benefit Policy Manual, Chapter 6, “Hospital Services Covered Under Part B,”
§10, and Chapter 8, §80.)
110.1 - Custodial Care Under a Hospice Program
(Rev. 1, 10-01-03)
A3-3159.1
Care furnished to an individual who has elected the hospice care option is custodial only
if it is not reasonable and necessary for the palliation or management of the terminal
illness or related conditions. (See the Medicare Benefit Policy Manual, Chapter 9,
“Coverage of Hospice Services Under Hospital Insurance,” §40.)
120 - Cosmetic Surgery
(Rev. 1, 10-01-03)
A3-3160, HO-260.11, B3-2329
Cosmetic surgery or expenses incurred in connection with such surgery is not covered.
Cosmetic surgery includes any surgical procedure directed at improving appearance,
except when required for the prompt (i.e., as soon as medically feasible) repair of

accidental injury or for the improvement of the functioning of a malformed body
member. For example, this exclusion does not apply to surgery in connection with
treatment of severe burns or repair of the face following a serious automobile accident, or
to surgery for therapeutic purposes which coincidentally also serves some cosmetic
purpose.
130 - Charges Imposed by Immediate Relatives of the Patient or
Members of the Patient’s Household
(Rev. 1, 10-01-03)
A3-3161, HO-260.12, B3-2332
A. General
These are expenses that constitute charges by immediate relatives of the beneficiary or by
members of their household. The intent of this exclusion is to bar Medicare payment for
items and services that would ordinarily be furnished gratuitously because of the
relationship of the beneficiary to the person imposing the charge. This exclusion applies
to items and services rendered by providers to immediate relatives of the owner(s) of the
provider. It also applies to services rendered by physicians to their immediate relatives
and items furnished by suppliers to immediate relatives of the owner(s) of the supplier.
B. Immediate Relative
The following degrees of relationship are included within the definition of immediate
relative.
• Husband and wife;
• Natural or adoptive parent, child, and sibling;
• Stepparent, stepchild, stepbrother, and stepsister;
• Father-in-law, mother-in-law, son-in-law, daughter-in-law, brother-in-law, and
sister-in-law;
• Grandparent and grandchild; and
• Spouse of grandparent and grandchild.
NOTE 1: A brother-in-law or sister-in-law relationship does not exist between the
physician, supplier or owner of a provider (or supplier) and the spouse of his wife’s or
her husband’s brother or sister.
NOTE 2: A father-in-law or mother-in-law relationship does not exist between a
physician or the owner of a provider and his or her spouse’s stepfather or stepmother.

A step-relationship and an in-law relationship continues to exist even if the marriage
upon which the relationship is based is terminated through divorce or through the death
of one of the parties. For example, if a provider treats the stepfather of the owner after
the death of the owner’s natural mother or after the owner’s stepfather and natural mother
are divorced, or if the provider treats the owner’s father-in-law or mother-in-law after the
death of their spouse, the services are considered to have been furnished to an immediate
relative, and therefore, are excluded from coverage.
C. Members of Patient’s Household
These are persons sharing a common abode with the patient as a part of a single family
unit, including those related by blood, marriage or adoption, domestic employees and
others who live together as part of a single family unit. A mere roomer or boarder is not
included.
D. Charges for Provider Services
Payment is not made under Part A or Part B for items and services furnished by providers
to immediate relatives of the owner(s) of the providers. This exclusion applies whether
the provider is a sole proprietor who has an excluded relationship to the patient, or a
partnership in which even one of the partners is related to the patient.
E. Charges for Physician and Physician-Related Services
This exclusion applies to physician services, including services of a physician who
belongs to a professional corporation, and services furnished incident to those services
(for example, by the physician’s nurse or technician) if the physician who furnished the
services or who ordered or supervised services incident to their services has an excluded
relationship to the beneficiary.
Professional corporation means a corporation that is completely owed by one or more
physicians, and is operated for the purpose of conducting the practice of medicine,
osteopathy, dentistry, podiatry, optometry, or chiropractic, or is owned by other health
care professionals as authorized by State law. Any physician or group of physicians
which is incorporated constitutes a professional corporation. (Generally, physicians who
are incorporated identify themselves by adding letters such as P.C. or P.A. after their
title.)
F. Charges for Items Furnished by Nonphysician Suppliers
This exclusion applies to charges imposed by a nonphysician supplier that is not
incorporated, whether the supplier is owned by a sole proprietor who has an excluded
relationship to the patient, or by a partnership in which even one of the partners is related.
It does not apply to charges imposed by a corporation (other than a professional
corporation), regardless of the patient’s relationship to any of the stockholders, officers,
or directors of the corporation or to the person who furnished the service.

140 - Dental Services Exclusion
(Rev. 1, 10-01-03)
A3-3162, HO-260.13, B3-2336
Items and services in connection with the care, treatment, filling, removal, or replacement
of teeth, or structures directly supporting the teeth are not covered. Structures directly
supporting the teeth mean the periodontium, which includes the gingivae, dentogingival
junction, periodontal membrane, cementum, and alveolar process. However, payment
may be made for certain other services of a dentist. (See the Medicare Benefit Policy
Manual, Chapter 15, “Covered Medical and Other Health Services,” §150.)
The hospitalization or nonhospitalization of a patient has no direct bearing on the
coverage or exclusion of a given dental procedure.
When an excluded service is the primary procedure involved, it is not covered regardless
of its complexity or difficulty. For example, the extraction of an impacted tooth is not
covered. Similarly, an alveoplasty (the surgical improvement of the shape and condition
of the alveolar process) and a frenectomy are excluded from coverage when either of
these procedures is performed in connection with an excluded service, e.g., the
preparation of the mouth for dentures. In like manner, the removal of the torus palatinus
(a bony protuberance of the hard palate) could be a covered service. However, with rare
exception, this surgery is performed in connection with an excluded service, i.e., the
preparation of the mouth for dentures. Under such circumstances, reimbursement is not
made for this purpose.
The extraction of teeth to prepare the jaw for radiation treatments of neoplastic disease is
also covered. This is an exception to the requirement that to be covered, a noncovered
procedure or service performed by a dentist must be an incident to and an integral part of
a covered procedure or service performed by the dentist. Ordinarily, the dentist extracts
the patient’s teeth, but another physician, e.g., a radiologist, administers the radiation
treatments.
Whether such services as the administration of anesthesia, diagnostic x-rays, and other
related procedures are covered depends upon whether the primary procedure being
performed by the dentist is covered. Thus, an x-ray taken in connection with the
reduction of a fracture of the jaw or facial bone is covered. However, a single x-ray or x-
ray survey taken in connection with the care or treatment of teeth or the periodontium is
not covered.
See also the Medicare Benefit Policy Manual, Chapter 1, “Inpatient Hospital Services,”
§70, and Chapter 15, “Covered Medical and Other Health Services,” §150 for additional
information on dental services.
150 - Services Reimbursable Under Automobile, No Fault, Any Liability
Insurance or Workers’ Compensation
(Rev. 1, 10-01-03)

A3-313, HO-260.14, B3-2370
The program may not pay for items and services for which payment has been made or
can reasonably be expected to be made promptly under a liability, automobile, no-fault or
workers’ compensation law or plan of the United States or a State. Also, payments for
items and services under the health insurance program are subject to repayment to the
appropriate trust fund if notice or information is received that payment is available for the
items and services under a liability, automobile, no-fault or workers’ compensation plan.
See the MSP manual for specific instructions.
170 - Inpatient Hospital or SNF Services Not Delivered Directly or
Under Arrangement by the Provider
(Rev. 1, 10-01-03)
A3-3164, HO-260.15, B3-2390, PM A 00-88
Nonphysician services provided to a Part A inpatient or Part B inpatient of a hospital or
to a Part A inpatient of a SNF which are not provided directly by the hospital/SNF or
under arrangement generally are excluded from coverage under Medicare.
This coverage exclusion does not apply to the following types of services:
• Physicians’ services for hospital inpatients or physician’s services other than
therapy for SNF inpatients (i.e., therapy provided by physicians is not covered for
any SNF Part A and Part B inpatient unless provided by the SNF, but other
physician services may be covered. Any normally-covered service may be
provided by a physician to a hospital inpatient);
• Physician assistant services;
• Nurse practitioners and clinical nurse specialists;
• Certified nurse-midwife services;
• Qualified clinical psychologist services;
• Certified registered nurse anesthetist; and
• Services of an anesthetist employed by a physician that were furnished during
cost reporting periods beginning on or after October 1, 1984, through any part of a
cost reporting period occurring before January 1, 1989.
The A/B MAC (B) may make direct payment on Part B bills for these services, if they are
medically necessary, even though they are not furnished directly or arranged for by the
hospital/SNF.

For SNF Part A inpatients, the following services are additional exceptions to this non
coverage rule and may be covered if provided by another authorized provider or supplier:
• Home dialysis supplies and equipment, self-care home dialysis support services,
and institutional dialysis services and supplies, including any related necessary
ambulance services;
• EPO;
• Hospice care related to a beneficiary’s terminal condition;
• Radioisotope services;
• Some customized prosthetic devices;
• Some chemotherapy and chemotherapy administration services;
• The following services which are considered beyond the scope of a SNF when
furnished in a Medicare participating Hospital or Critical Access Hospital. Note that this
exception does not apply if the service is furnished in an ASC. Specific coding is
described in the Medicare Claims Processing Manual.
º Cardiac catheterization;
º CT scans;
º MRIs;
º Ambulatory surgery involving the use of an operating room;
º Radiation therapy;
º Emergency services;
º Ambulance services related to the six services listed immediately above;
and ambulance transportation related to dialysis services.
180 - Services Related to and Required as a Result of Services Which
Are Not Covered Under Medicare
(Rev. 189, Issued: 06-27-14, Effective: 05-30-14, Implementation: 06-29-14)
Medical and hospital services are sometimes required to treat a condition that arises as a
result of services that are not covered because they are determined to be not reasonable
and necessary or because they are excluded from coverage for other reasons. Services
"related to" non-covered services (e.g., cosmetic surgery, non-covered organ transplants,
non-covered artificial organ implants, etc.), including services related to follow-up care

and complications of non-covered services which require treatment during a hospital stay
in which the non-covered service was performed, are not covered services under
Medicare. Services "not related to" non-covered services are covered under Medicare.
Following are examples of services "related to" and "not related to" non-covered services
while the beneficiary is an inpatient:
• A beneficiary was hospitalized for a non-covered service and broke a leg while in
the hospital. Services related to care of the broken leg during this stay is a clear
example of "not related to" services and are covered under Medicare.
• A beneficiary was admitted to the hospital for covered services, but during the
course of hospitalization became a candidate for a non-covered transplant or
implant and actually received the transplant or implant during that hospital stay.
When the original admission was entirely unrelated to the diagnosis that led to a
recommendation for a non-covered transplant or implant, the services related to
the admitting condition would be covered.
• A beneficiary was admitted to the hospital for covered services related to a
condition which ultimately led to identification of a need for transplant and
receipt of a transplant during the same hospital stay. If, on the basis of the nature
of the services and a comparison of the date they are received with the date on
which the beneficiary is identified as a transplant candidate, the services could
reasonably be attributed to preparation for the non-covered transplant, the services
would be "related to" non-covered services and would also be non-covered.
Following is an example of services received subsequent to a non-covered inpatient stay:
After a beneficiary has been discharged from the hospital stay in which the beneficiary
received non-covered services, medical and hospital services required to treat a condition
or complication that arises as a result of the prior non-covered services may be covered
when they are reasonable and necessary in all other respects. Thus, coverage could be
provided for subsequent inpatient stays or outpatient treatment ordinarily covered by
Medicare, even if the need for treatment arose because of a previous non-covered
procedure. Some examples of services that may be found to be covered under this policy
are the reversal of intestinal bypass surgery for obesity, complications from cosmetic
surgery, removal of a non-covered bladder stimulator, or treatment of any infection at the
surgical site of a non-covered transplant that occurred following discharge from the
hospital.
However, any subsequent services that could be expected to have been incorporated into
a global fee are not covered. Thus, where a patient undergoes cosmetic surgery and the
treatment regimen calls for a series of postoperative visits to the surgeon for evaluating
the patient's progress, these visits are not covered.

Transmittals Issued for this Chapter
Rev # Issue Date Subject Impl Date CR#
R198BP 11/06/2014 Medicare Coverage of Items and Services in
Category A and B Investigational Device
Exemption (IDE) Studies
01/05/2015
8921
R189BP 06/27/2014 Invalidation of National Coverage
Determination 140.3 - Transsexual Surgery
06/29/2014
8825
R186BP 04/16/2014 Clarification to Pub. 100-02, Medicare Ben
efit
Policy Manual Regarding Antigens and
Deletion of Section 13.14 from Chapter 13 of
Pub. 100-08, Medicare Program Integrity
Manual
05/12/2014
8665
R184BP 04/11/2014 Clarification to Pub. 100-
02, Medicare Benefit
Policy Manual Regarding Antigens and
Deletion of Section 13.14 from Chapter 13 of
Pub. 100-08, Medicare Program Integrity
Manual – Rescinded and replaced by
Transmittal 186
05/12/2014
8665
R170BP 05/10/2013 Updates to Medicare Coverage of Hepatitis B
Vaccine and its Administration and Medicare
Coverage of the Annual Wellness Visit
(AWV) Providing Personalized Prevention
Plan Services (PPPS)
06/10/2013
8275
R122BP 04/09/2010 Claims Submitted for Items or Services
Furnished to Medicare Beneficiaries in State
or Local Custody
Under a Penal Authority and
Examples of Application of Government
Entity Exclusion. This CR rescinds and fully
replaces CR 6544.
07/09/2010
6880
R110BP 09/04/2009 Claims Submitted for Items or Services
Furnished to Medicare Beneficiaries in State
or Local Custody Under a Penal Authority and
Examples of Application of Government
Entity Exclusion – Rescinded and replaced by
CR 6880, Transmittal 122
12/07/2009
6544
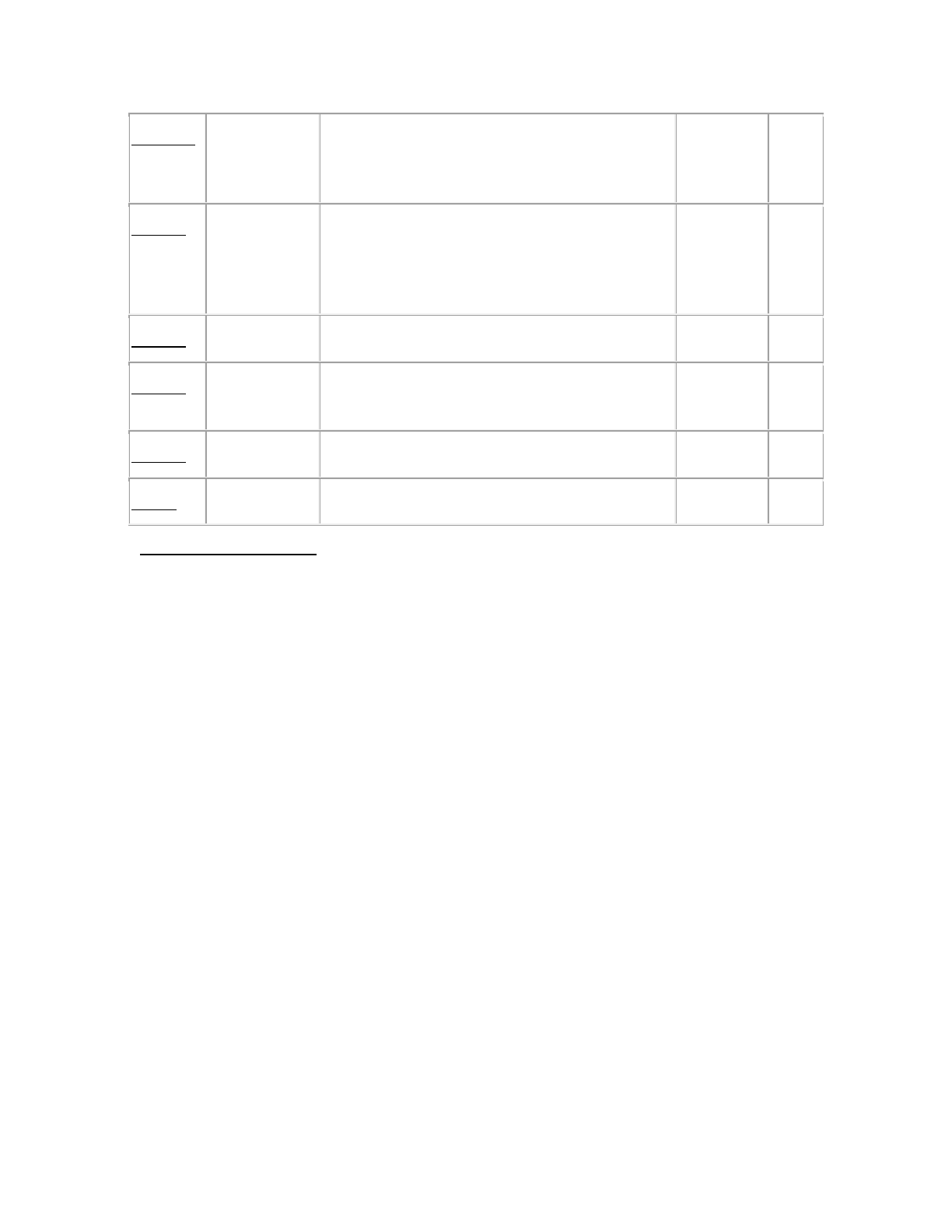
R102BP 02/12/2009 Shipboard Services Billed to the Carrier and
Services Not Provided Within the United
States
03/13/2009
6327
R95BP 10/03/2008 Shipboard Services Billed to the Carrier and
Services Not Provided Within the United
States – Rescinded and replaced by CR 6327,
Transmittal 102
01/05/2009
6217
R66BP 02/23/2007 Services Not Provided Within United States 04/02/2007
5427
R39BP 11/10/2005 Auditory Osseointegrated and Auditory
Brainstem Devices
12/12/2005
4038
R38BP 08/19/2005 Services Not Provided Within United States 11/17/2005
3781
R1BP 10/01/2003 Introduction to the Benefit Policy Manual N/A N/A
Back to Top of Chapter
