
A
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
National Family Planning
Costed Implementation Plan
2015-2020
Ministry of Health and Population
Department of Health Services
Family Health Division
2015 (2072)
Government of Nepal
FP CIP
2015-2020

National Family Planning
Costed Implementation Plan
2015-2020
November 2015
Ministry of Health and Population
Department of Health Services
Family Health Division
2015 (2072)
Government of Nepal





NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
VI

VII
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
AIDS Acquired Immune Deficiency Syndrome
ASFR Age-Specific Fertility Rate
BCR Benefit-Cost Ratio
CBA Cost-Benefit Analysis
CDB Curriculum Development Board
CHD Child Health Division
CIP Costed Implementation Plan
CAC Comprehensive Abortion Care
CPR Contraceptive Prevalence Rate
CSE Comprehensive Sexuality Education
CTS Clinical Training Skill
CYP Couple Years of Protection
DDA Department of Drug Administration
DFID Department for International Development
DHS Demographic and Health Survey
DHO District Health Office
DoHS Department of Health Services
DPHO District Public Health Office
EDCD Epidemiology and Disease Control Division
EDP External Development Partners
EPI Expanded Program on Immunization
FARHCS Facility-based Assessment on Reproductive Health Commodities & Services
FCHV Female Community Health Volunteers
FHD Family Health Division
FHI360 Family Health International
FP Family Planning
FPAN Family Planning Association of Nepal
FPMCH Family Planning, Maternal and Child Health
FSW Female Sex Workers
FTE Full-Time Equivalent
GDP Gross Domestic Product
GBV Gender Based Violence
GoN Government of Nepal
HA Health Assistants
HP Health Post
HIV Human Immunodeficiency Virus
HMIS Health Management Information System
HMG Health Mother Groups
HRH Human Resources for Health
ICPD International Conference on Population Development
IFPSC Integrated Family Planning Service Center
IMR Infant Mortality Rate
INGO International Non- Governmental Organisation
Ipas International Post-abortal Care Services
IUCD Intrauterine Contraceptive Device
LARC Long-Acting Reversible Contraceptive
LAM Lactational Amenorrhea Method
LMD Logistics Management Division
LMIS Logistics Management and Information System
mCPR Modern Contraceptive Prevalence Rate
MD Management Division
Abbreviations

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
VIII
MDG Millennium Development Goal
MICS Multiple Indictor Cluster Survey
M&E Monitoring and Evaluation
MNCH Maternal, Newborn, and Child Health
MNH Maternal and Neonatal Health
MoE Ministry of Education
MoF Ministry of Finance
MoHP Ministry of Health and Population
MSI Marie Stopes International
NCASC National Centre for AIDS and STD Control
NDHS Nepal Demographic and Health Survey
NFHS Nepal Family Health Survey
NGO Non- Governmental Organisation
NGOCC Non-Governmental Organization Coordination Committee
NHEICC National Health Education, Information and Communication Centre
NHSP Nepal Health Sector Program
NHSP IP Nepal Health Sector Program Implementation Plan
NHTC National Health Training Centre
NPC National Planning Commission
NPHL National Public Health Laboratory
NPR Nepalese Rupees
NSV Non Scalpel Vasectomy
NTC National Tuberculosis Centre
OPM Oxford Policy Management
PHCC Primary HealthCare Centre
PHC/ORC Primary Health Care Outreach Clinics
PHCRD Primary Health Care Revitalization
PMTCT Prevention of Mother-To-Child Transmission of HIV
PPICD Policy, Planning and International Cooperation Division
PPIUCD Post-Partum Intrauterine Contraceptive Device
PPP Private Public Partnership
PSI Population Services International
RH Reproductive Health
RHCC Reproductive Health Coordination Committee
RHCS Reproductive Health Commodity Security
RHD Regional Health Directorate
RHSC Reproductive Health Steering Committee
RHTC Regional Health Training Center
SBCC Social and Behavioural Change Communication
SCM Supply Chain Management
SDP Service Delivery Points
SHP Sub-Health Post
SMNSC Safe-motherhood and neonatal Sub-committee
SRH Sexual and Reproductive Health
STI Sexually Transmitted Infection
STS Service Tracking Survey
TFR Total Fertility Rate
TSG Target Setting Group
TWG Technical Working Group
U5MR Under-5 Mortality Rate
UNFPA United Nations Population Fund
UNICEF UnitedNationsChildren’sFund
USAID United States Agency for International Development
USD United States Dollar
VSC Voluntary Surgical Contraception
WASH Water, Sanitation and Hygiene
WHO World Health Organization

IX
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Table of Contents
Introduction 1
Current Situation on Population and Family Planning 2
Population 2
Impressive but unequal progress in Family Planning 2
Unmet Need 3
Demand Satised for modern contraception 3
Contraceptive Method Mix 4
Exposure to family planning message 4
Availability of contraceptive services 4
Adolescents’ use of contraception 5
Issues and Challenges of the current Family Planning Program 6
Enhance quality FP Service Delivery 6
Capacity of service providers 8
Contraceptive commodities and logistics 9
Strengthening FP service seeking behavior 9
Advocacy for family planning 10
Management, monitoring and evaluation 10
Projecting Population Growth and Method Mix to Scale up Family Planning 11
National Costed Implementation Plan for Family Planning 12
Purpose, Vision & Goal 12
Strategic action areas and objectives 12
Strategic Action Area: Enabling Environment 14
Strategic Action Area: Demand Generation 14
Strategic Action Area: Enhancing Service Delivery 16
Strategic Action Area: Capacity Building 17
Strategic Action Area: Research and Innovation 18
Costs and Benefits of Scaling up Family Planning 19
Demographic impact 19
Health Benets 20
Social and economic benets 21
Investment requirements 22
Return on investment 23

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
X
The way forward 24
Institutional Arrangements for Implementation 24
District-level Planning 25
Resource Mobilization 25
Monitoring and Evaluation Framework 26
References 33
List of Annexes
Annex A Estimated Total Resources Required and Disaggregated by Area 35
Annex B Estimated resource requirements of General Programme Management, by key
interventions, related programmatic activities and year, (natural units) 37
Annex C Estimated resource requirements of Enabling Environment, by key
interventions, related programmatic activities and year, (natural units) 38
Annex D Estimated resource requirements of Demand Generation, by key
interventions, related programmatic activities and year, (in natural units) 39
Annex E Estimated resource requirements of Enhancing Service Delivery, by
key interventions, related programmatic activities and year, (natural units) 42
Annex F Estimated resource requirements of Capacity Building, by key
interventions, related programmatic activities and year, (natural units) 45
Annex G Estimated resource requirements of Research & Innovation, by key
interventions, related programmatic activities and year, (natural units) 47
A n n e x H S c e n a r i o M o d e l l e d 4 9
List of Figures
Figure 1: Trends in Fertility 1
Figure 2: Trends in Contraceptive Prevalence Rate for Modern Methods 3
Figure 3: Method Mix (NMICS, 2015) 4
Figure 4: Trends in Use of Family Planning 5
Figure 5: Organogram of MoHP Health Care Delivery 7
Figure 6: Total population projections for Nepal (2011-2030) 19
Figure 7: Increase in income per capita 20
Figure 8: Maternal Mortality Rate 20
Figure 9: Cumulative cost savings 22
Figure 10: Projected expenditure under the FP Scale-up and Counter factual scenarios capita 22
Figure 11: CIP Coordination and Management Structure 25
List of Tables
Table 1: Changes in Method Mix 11
Table 2: Estimate of total resource requirements (millions) 13
Table 3: Dependency ratios 19
Table 4: Cost savings in ve sectors (millions) 21
Table 5: Cost per CYP and cost per user 22
Table 6: Investment metrics 23

XI
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Nepal is aspiring to graduate from a ‘Least
Developed Country’ to a ‘Developing Country’
by 2022 and is commied to improving the health
status of its people through reduction in maternal,
neonatal, infant and under-ve mortality. In the
area of Family Planning (FP), the Government
of Nepal aims to enable women and couples to
aain the desired family size and have healthy
spacing of childbirths by improving access to
rights-based FP services and reducing unmet need
for contraceptives. The Family Health Division
(FHD)/ Ministry of Health and Population
(MoHP) revised the national FP program to
devise strategies and interventions that will
enable the country to increase access to and use
of quality FP services by all—and in particular by
poor, vulnerable and marginalized populations.
Under the leadership of the MoHP a national
Costed Implementation Plan (CIP) on family
planning was developed in close consultation
with all stakeholders. The purpose of the CIP is
to articulate national priorities for family planning
and to provide guidance at national and district
levels on evidence-based programming for family
planning so as to achieve the expected results,
as well as to identify the resources needed for
CIP implementation. In addition, the CIP is
intended to serve as a reference document for
external development partners including donors
and implementing agencies to understand and
contribute to the national priorities on family
planning outlined in the Plan to ensure coherence
and harmonization of eorts in advancing family
planning in Nepal. To address the existing
challenges and opportunities for scaling up rights-
based FP in the country, the CIP focuses on ve
strategic areas. They are Enabling Environment,
Demand Generation, Service Delivery, Capacity
Building and Research & Innovation. Through
investment in these areas the country aims
to increase demand satised for modern
contraceptives from 56% (NDHS, 2011) to 62.9%
and Contraceptive Prevalence Rate (CPR) for
modern methods from 47% in 2014 (MICS) to 50%
by 2020. Likewise it aims to reduce unmet need
for FP from 25.2% in 2014 (MICS) to 22% which
would allow the country to achieve a replacement
level fertility of 2.1 births per women by 2021.
These targets may appear relatively modest but
were chosen to reect the context of a country
that has witnessed impressive gains in FP but
has CPR that has been stagnant for some time in
recent years. There are also signicant variations
in FP service use by age, geographic region,
wealth quintile and spousal separation. The target
therefore reects a FP strategy that aims to give
individual and couples a choice of contraceptive
methods with a special emphasis on reaching the
poor, vulnerable and marginalized groups. The
strategy also includes changes in the method mix
over time, with a balance between permanent,
long-acting reversible methods and short-acting
methods.
The total resources required for scaling up FP in
Nepal for the period 2015-2020 is NPR 13,765.2
million (corresponding to approximately USD
154.2 million) for six years The majority (57%)
of this total is due to the costs that are directly
incurred in delivering FP interventions. One third
(35%) is due to programme costs, or expenditures
on activities at the wider population level that
are required for FP interventions to be eectively
implemented. The remainder (8%) is indirect
costs, which predominately relate to health facility
overhead costs such as administrative sta and
utility bills. Among the programme costs the
largest planned expenditure category over the
period is Enhancing Service Delivery (1,836.9
million NPR), followed by Demand Generation
(738.4 million NPR), Capacity Building (793.8
million NPR) and Enabling Environment (679.2
million NPR). General Programme Management
Executive Summary

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
XII
(303.1 million) and Research & Innovation (446.3
million NPR) constitute the remainder of the total
projected expenditure of 4,797.7 million NPR.
The scale up of family planning in Nepal will
contribute to further reduction in maternal
mortality rate as well as reduction in infant and
child mortality rates. It is estimated that there
will be 230 fewer maternal deaths a year and
approximately 3,000 fewer infant deaths each year
by 2030 in the FP scale-up scenario compared to
the counterfactual scenario. Likewise the number
of couple years of protection (CYPs), which is a
function of both population growth and increased
contraceptive use, is estimated at 2.9 million
by 2030 under the FP scale-up. The projected
demographic impacts of FP scale up include
a smaller increase in total population (32m by
2030 compared 33.5m under the counterfactual
scenario) and a lower (total) dependency ratio
that lead to achievement of 4.6% higher income
per capita by 2030 catalyzed by the demographic
dividend.
Slower rates of population growth translate into
cost savings to the government as there are fewer
people who need social services. A cumulative
cost savings of 46,569.9 million NPR is estimated
to be achieved over the time period (2015-2030)
under the FP scale-up scenario compared to the
counterfactual scenario in primary education, child
immunization, treatment of child pneumonia,
maternal health services and improved water
sources. Over the time period 2015-2030, for every
rupee spent on FP, Nepal is projected to save
3.1 rupees in the ve sectors mentioned above
if the FP scale-up scenario is achieved. There
are likely to be cost savings to other sectors not
included here – those related to health sector
(like improved pregnancy outcomes, reduced
unsafe abortion from unwanted pregnancies
and improved protection from HIV and other
STIs) and those outside the health sector (like
cost saving in providing social services, climate
change benets and improvements in women’s
right, empowerment and gender equality).

1
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
The historic people’s movement in 2006
entrenched health as a fundamental human
right in Nepal (National Development Plan,
2007/2008–2010/2011), but the country has long
since recognized the benets of scaling up Family
Planning (FP). This can be seen in the prominence
given to FP services throughout the country’s
development plans and strategies, including:
the three-year Interim Development Plan,
2010/2011–2012/2013; the Eleventh Development
Plan, 2008-2013; the Second Long-Term Health
Plan, 2006-2017; the Population Perspective Plan,
2010-2031; and the Nepal Health Sector Program
Implementation Plan II, 2010-2015 (NHSP-IP II)
and NHSP III, currently being developed.
The intention behind these eorts is to develop
a well-educated, skilled and healthy nation and
graduate from a ‘Least Develo ped Country’ to
a ‘Developing Country’ by 2022. To do so it will
require not only that the economy grows by 8%
per annum, but that the growth is inclusive.
Given the level of inequality portrayed in the
recently released Nepal Human Development
Report 2014, substantial eorts are required to
reduce inequality and increase levels of human
development to sustain the peace that has only
recently been achieved. Improving health is one of
the goals with ambitious targets aimed at reducing
maternal, neonatal, and infant and under-ve
mortality as well as number of underweight
children. In the area of FP, the Government of
Nepal aims to enable women and couples to aain
the desired family size and have healthy spacing
of childbirths by improving access to rights-based
FP services and reducing unmet need for modern
contraceptives.
To expand access to quality care FP services
have been integrated into Reproductive health
package (as a basic health service package) and
provided free-of-charge to entire population in
governmental clinics. For the past thirteen years
Nepal has made remarkable progress in increasing
utilization of modern methods among currently
married women from 35% (NDHS, 2001) to
47.1 (MICS, 2014). Demand satised by modern
methods has also increased up to 63% (MICS,
2014) and unmet need for FP declined from 31%
in 1996 (NFHS) to 25.2 in 2014 (MICS).
Regardless of the overall progress in FP disparities
in FP utilization rates are still visible among
dierent sub-regions, and specic population
groups such as adolescents, poor and marginalized
women. If Nepal is to meet its domestic targets
and its international obligations—notably the
Millennium Development Goals (MDGs) and
the targets of the 1994 International Conference
on Population Development (ICPD)—then the
country will need to broaden the reach and the
scope of FP services.
The Family Health Division (FHD) of the Ministry
of Health and Population (MoHP) has begun a
process of reviewing and revising the country’s
FP program to devise strategies and interventions
that will enable accelerated progress towards
ensuring increased and equitable access to and
utilization of quality FP information and services
by all—and in particular by poor, vulnerable and
marginalized populations.
Introduction
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
2
Current situation on Population
and Family Planning
Population
The 2011 Population Census recorded the
population of Nepal at 26.5 million, with 17% of
the population living in urban areas. Population
density (average number of population per square
kilometre) has increased to 180 per km2, from 157
in 2001.
The country’s population has grown by 3.3 million
over the last decade—an annual average growth
rate of 1.35%. Over the last 40 years; however,
Nepal’s population has more than doubled,
growing rapidly between 1970 and 1980 but
slowing down in recent years. An indication
of that, is evident by the decrease of an average
household size from 5.4 (2001) to 4.9 (2011). For
the past eighteen years, the Total Fertility Rate
(TFR) gradually reduced from 4.6 (NFHS1996) to
2.3 (MICS, 2014) as it is shown in Figure 1.
The decline in fertility can be explained by several
factors such as increased age at marriage, beer
access to education among girls including in rural
areas; shi in ideal number of children among
women from 2.9 in 1996 to 2.1 in 2011 (NDHS) and
beer access to modern contraception in order to
space or limit childbearing to aain the desired
number of children.
A large proportion (37%) of the Nepalese
population is under the age of 15, although this
proportion has declined from 41% in 2006. 11% of
the population is under ve years, a decrease since
2006. Both of these are indications of a declining
trend in fertility. As is the fact, that people 65-and-
older account for 6% of the total population (up
from 4% in 2006). Examining the proportion of
children-under-ve in urban against rural areas
suggests that recent declines in fertility are more
evident in urban than rural areas and that the
transition to lower fertility began with the urban
population.
Contributing to the decline in household size is
that almost 2 million Nepalese of working age
(15-59 years) live abroad (up from 760,000 in
2001). 25% of households reported that at least one
member of their household is absent or is living
out of the country
1
, while 57% of households
reported that at least one person had migrated
away from the household at some time in the past
10 years
2
. Among the households that reported
migration of former residents, on average, about
two people migrated. It is unsurprising, therefore,
that the number of female-headed households has
increased from 15% (2001) to 23% (2006) to 26%
(2011).
Impressive but unequal progress in
Family Planning
FP has been a longstanding strategy of the
Government of Nepal in order to promote
the development of an educated and healthy
population (National Planning Commission,
2002). To achieve this, the country has set itself
ambitious goals aimed at increasing access to
voluntary FP services with a focus on poor,
vulnerable and marginalized populations.
1
Central Bureau of Statistics: Nepal Population Census 2011
2
MoHP: Nepal Demographic Health Survey, 2011
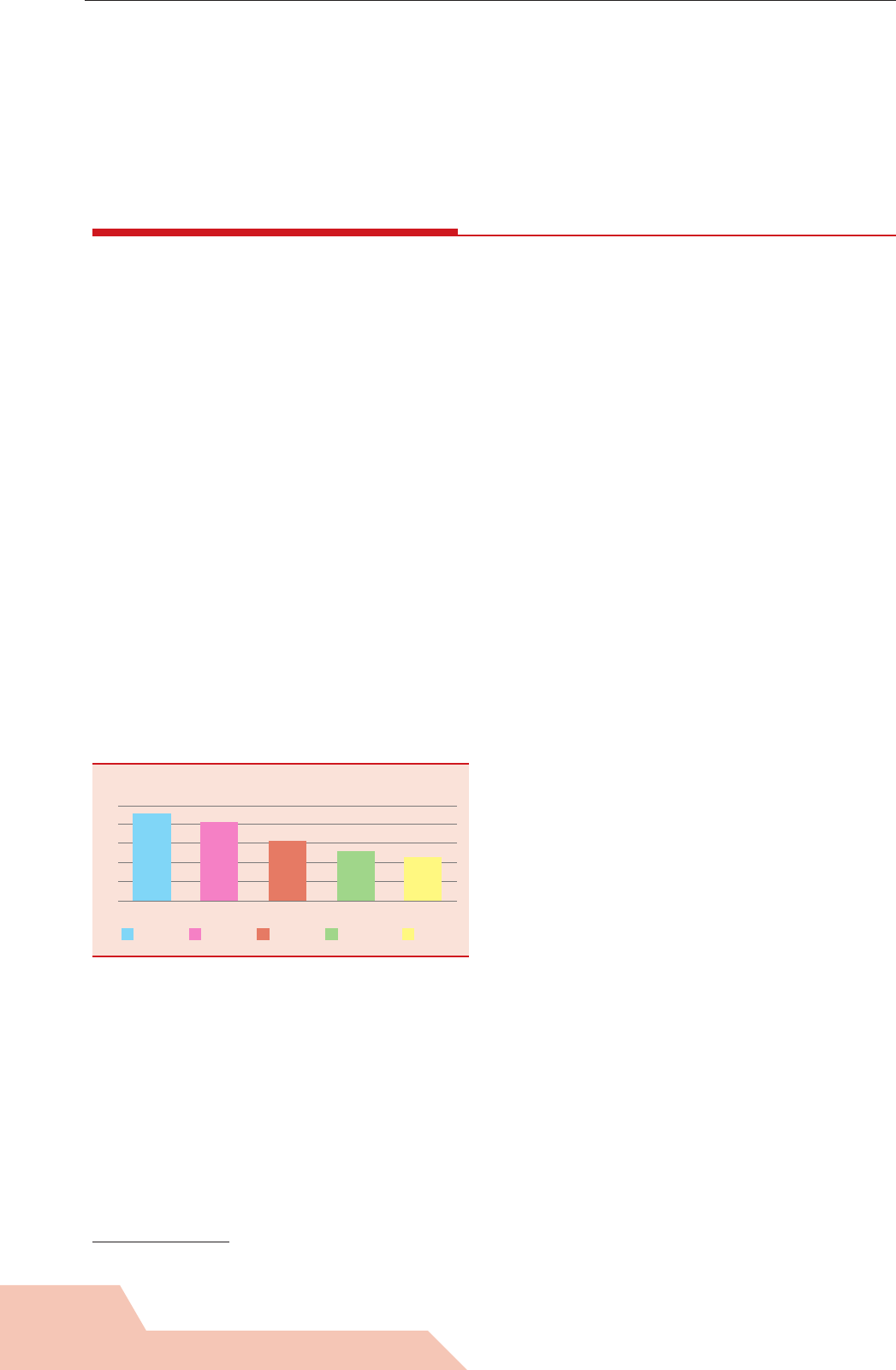
FIGURE 1:
Trends in Fertility
5
4
3
2
1
0
TFR
1996 2001 2006 2011 2014
1996 2001 2006 2011 2014
4.6
4.1
3.1
2.6
2.3

3
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Nepal made a signicant progress in increasing
contraceptive prevalence rate for modern
contraception among currently married women
from 35% in 2001 to 43% in 2011 (NDHS) and 47.1
in 2014 (MICS). The trends are shown in Figure 2.
Regardless of the increased use of modern
contraception, access to services is not yet universal
across the country, and mCPR varies among the sub-
regions with the highest rate at 55.1% in Far Western
Terai to 32% in Eastern Hill. Factors aecting access
to FP services are numerous including availability
and capacity of service providers; availability of
supplies; social and cultural beliefs; accessibility
of health facilities. To address low utilization of FP
services in sub-regions, a district level analysis of
service delivery and needs of communities should
be done.
Signicant inequalities in using modern
contraception still exist among poorest quintile and
highest quintile of population (35.6% vs. 48.9%).
Rural population has lower total contraceptive
rate than urban residents, however, it has higher
utilization of female and male sterilization, while
more women living in urban areas use pills,
condoms and traditional methods.
Migration complicates the interpretation of
standard FP indictors for Nepal. For example, it
is interesting to note that among married women
who live with their husbands the CPR is 55.5%.
This most likely indicates that overall CPR is
inuenced by the large number of women whose
husbands live away from home and who are
therefore not as likely to be using contraceptives.
These women may eventually need contraceptives
when their husbands return, therefore, should not
be excluded from the data on family planning,
neither from FP programmes.
Unmet Need
Unmet need measures women who do not want
any more births or those who want to postpone
the next birth at least two more years—birth
limiting and birth spacing respectively, yet are not
using a method of contraception. 25.2% of women
in Nepal (just over one-in-four) have an unmet
need for FP (MICS, 2014). While this has declined
noticeably from 31% in 1996 (NFHS) the present
level of unmet need (25.2%) is still at the same
level as it was in 2006 (25%) and provides scope
for the expansion of FP services.
Unmet need declines with age from 42% among
adolescent girls to 13% among the oldest age
group. For poorest quintile unmet need is 31%
(9% for spacing and 22% for limiting) compared
to 22% for the richest quintile (8% for spacing and
14% for limiting). Unmet need is also higher in
rural areas and is highest in the hill zone.
Migration remains a signicant factor in increasing
unmet need in Nepal, as it is for the decline in TFR.
The standard denition of unmet need counts
a woman whose husband is away from home
and who is therefore not using contraception as
having an unmet need for FP if she says that she
wants to delay or stop childbearing. In the context
of the countries such as Nepal, where spousal
separation is due to migration, it is common that
unmet need statistics are more enlightening when
disaggregated. The 2011 NDHS shows that unmet
need for women living with their husbands is
16%, while it is 58% for women whose husband
has lived elsewhere for more than a year. Clearly,
FP programs need to be tailored, recognising the
dierent contraceptive needs of these groups.
Unmet need also contributes to need for abortion.
According to NDHS (2011), 20% of the interviewed
women mentioned that the main reason for their
most recent abortion was that they did not want
any more children, while 12% said that their
husband/partner did not want the child.
contraception
Another good indicator is demand satised for
modern contraception. International evidence
suggests that for FP to achieve an impact on
population development, this indicator should be
FIGURE 2: Trends in Contraceptive Prevalence Rate
for Modern Methods
50
45
40
35
30
25
20
15
10
5
0
26
35
44 43
47
1996 2001 2006 2011 2014
mCPR
mCPR

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
4
increased to at least 75%, including in rural areas
(USAID 2013).
Overall, demand satised for modern methods in
Nepal is relatively high, although there is still some
way to go in achieving the 75% target, particularly
when the indicator is disaggregated by socio-
economic characteristics and sub-regions. For
example, the lowest level of demand satised by
modern contraceptives was recorded in Western
Hill, Eastern Hill and Eastern Mountain.
The 2011 NDHS shows that demand satised for
modern methods is 56%, but with adolescent girls
(24.3%), those living in the Eastern Hills (42.7%)
and Western Hill (44.2%) and those in the lowest
wealth quintile (49.3%), have the lowest demand
satised.
Contraceptive Method Mix
The period from 1996 to 2006 saw a remarkable
increase in the use of female sterilisation, pill,
injectables and male condoms, although the use has
declined slightly in 2011 for female sterilisation and
injectables, yet has increased for male sterilisation
(Figure 4). While among the most eective methods,
Intrauterine Contraceptive Device (IUCD) and
implants continue to have a relatively low uptake
rate, although this did double between 2006 and
2011. As shown in Figure 4, the use of traditional
FP methods, although not promoted by the FP
program, also doubled over the same period (from
3.7% to 6.5%) although the NMICS in 2015 showed
a decline to 2.5% (Figure 3).
Exposure to family planning
message
According to NDHS 2011, 55% of women and 70%
of men (age 15-49) saw a FP message recently on
a poster or hoarding board, while 52% of women
and 59% of men heard FP messages broadcast
through radio. NDHS results demonstrate that:
exposure to FP messages is lower in rural areas
than in urban and older age categories of women
are exposed less to FP messages. This is an
important nding since mothers and mothers-in-
law can be a vital source of information on FP for
young girls.
Availability of contraceptive services
The Family Health Division of the MoHP has
noted the rapid expansion of the private sector
and has commied to encourage the private sector
and non-governmental organisations to play an
expanded role in the national FP programme
(NHSP-IP II).
Currently, short-acting FP methods (male
condoms, pill, and injectables) are provided on
a regular basis through all governmental health
posts, sub health posts, Primary health Care
Outreach Clinics (PHC-ORC), periphery level
health workers and volunteers (Condoms and
resupply of pills). Services such as IUCD and
Implants are available only at limited number of
Primary Health Care Centres (PHCC) and health
posts where trained personnel are available.
Depending on the district, sterilization services
are provided at static sites or through scheduled
“seasonal” or mobile outreach services. Almost
all district Family Planning, Maternal and Child
Health (FPMCH) clinics are providing all types
of temporary FP methods regularly. FP services
are also providing by INGOs (International
Non- Governmental Organisations), NGOs (Non-
Governmental Organisation), private service
providers and social marketing system.
Sixty-nine percent (69%) of the population accesses
their modern contraceptive method from the
government sector, however this is a signicant
decline from the 77% recorded in the 2006 NDHS
and does vary by method choice. Because method
choice depends on the level of health facility, it
denes where women go to obtain a preferred
FIGURE 3: Method Mix (NMICS, 2015)
Traditional
5%
Female
Sterilization
36%
Male
Sterilization
10%
IUCD
3%
Implant
3%
Injectables
26%
Pills
26%
Condoms
26%

5
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
method. A risk is a limitation of choices if a woman
hasn’t received full information about all methods
at the point of entry.
9% of users obtain their methods from the NGO
sector, mostly from Marie Stopes International
(6%) and the Family Planning Association of Nepal
(2%). It is the commercial private sector that has
seen the most marked increase, however—rising
from just 14% in 2006 to 22% in 2011. Of particular
note is the use of pharmacies for the short-term
methods, with 32% of pill users, 12% of injectable
users and 52% of condom users obtaining
their methods from this source. Private sector
pharmacies are widespread in Nepal and provide
diagnosis and treatment including prescription of
drugs. They are a major recipient of out-of-pocket
spending by all income groups, although they are
predominantly based in urban areas.
If FP is to reach those who are currently
underserved or population groups that are not
being adequately reached by current approaches,
then the FP programme will need to make the best
use of all resources available. This will require that
considerable eort be devoted to strengthening
partnerships with the private and NGO sectors
3
.
Adolescents’ use of contraception
Adolescents and youth account for one-third of
Nepal’s population. Early marriage and early
childbearing continue to be the norm in Nepal,
although the median age at rst marriage has
increased over the years. Adolescent childbearing
is still common, although decreasing – adolescent
birth rate is 81 per 1000 women (MICS 2014 – 71).
Among adolescents and youth, contraceptive
use can prevent unintended pregnancy and
early childbearing and their consequences. In
Nepal knowledge about FP is almost universal
(99.9 percent) including among adolescents
and youth. However, only 14percent of married
adolescent girls age 15-19 and 24 percent of
married women age 20-24 are currently using a
modern contraceptive method. Unmet need for
FP has been estimated to be highest (42 percent)
for married girls age 15-19, followed by 37 percent
among married women age 20-24 (MoHP et al.,
2012). The data on contraceptive use and unmet
need among young people is unavailable in
Nepal. According to Demographic and Health
Surveys (DHS) comparative report on adolescent
sexual and reproductive health around the world,
unmarried young women are more likely to use
modern contraceptive methods and also to have
higher levels of unmet need for FP than currently
married young women (Khan and Mishra, 2008).
FIGURE 4: Trends in Use of Family Planning
50
45
40
35
30
25
20
15
10
5
0
Any modern method Female Sterilisation
Method type
Percent of married women
currently using a method of FP
Male Sterilisation Any traditional method
1996 NHFS 2001 NDHS 2006 NDHS 2011 NDHS
3
NHSP-IP II – Mid-Term Review Report (2013)

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
6
Issues and Challenges of
the current Family Planning
Program
For eective scale-up of the FP program in
Nepal, a number of challenges and issues must
be addressed by 2021. Five program areas or
components are essential for implementing
a successful FP program: strong advocacy to
increase visibility and support for the program,
behavior change communication interventions to
address the knowledge-use gap among FP clients;
strong management to ensure ecient and
eective program implementation; availability of
broader range of contraceptive commodities at
all levels of service delivery; sucient numbers
of skilled health providers to provide FP services
eectively and appropriately equipped facilities
to provide quality FP services.
Enhance Quality Family Planning
Service Delivery
Access to high-quality FP services is a human right
and should be provided without discrimination
and coercion.
Family planning information and services are
provided through government, social marketing,
non-governmental organizations and private
sectors. In government health system, currently,
short-acting FP methods (male condoms, pill, and
injectables) are provided on a regular basis through
all levels of health facilities including health posts,
sub health posts, PHC- Outreach clinics. Female
Community Health Volunteers (FCHVs) provide
information to community people, and distribute
Condom and resupply pills. Services such as
IUCD and Implants are available only at limited
number of PHCCs and Health Posts (HPs) where
trained personnel are available. Depending on the
district, sterilization services are provided at static
sites or through scheduled “seasonal” or mobile
outreach services. Almost all district hospitals are
providing all types of temporary and permanent
FP methods regularly. Therefore, at central,
regional and district level women can access
all the 7 methods of FP while at primary health
care accessibility to a full range of FP services is
limited. Family Planning services are integrated at
all levels of MoHP health care delivery, as shown
in Figure 5.
Due to integrated nature of FP services, women
should be able to access the services at any
service delivery point and in any geographical
district. However, “supply” and “demand”
related challenges aecting the access still exist
in the country. For example, shortage of human
resources for health overall and in particular lack
of skilled service providers, lack of supplies and
contraceptives especially at primary health care
level aect accessibility and quality of contraceptive
services. Women experience challenges to access
the services due to travel 2014 arrangements such
as nding a means of transportation, time spent on
travel, costs of travel; and sometimes due to costs
of services (STS, 2013). In some cases, gender and
culture related norms aect the access, for example
in some cases women needed to get a permission
from husband/other members of family to go to a
health facility for healthcare services, including FP .
(STS, 2013)
To reduce access barriers the Government of Nepal
(GoN) provides free counseling and services
including contraceptives of choice, in addition
to a nominal wage compensation for clients
undergoing Voluntary Surgical Contraception
(VSC) and covers costs of services included in
the essential health package. However, due to a
lack of awareness about these entitlements, some
groups of population have not used the incentives

7
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
FIGURE 5: Organogram of MoHP Health Care Delivery
4
and continue paying out of pocket. Interventions
on increasing awareness of clients and service
providers about entitlements for free care at all
levels of public-sector health care institutions
should be delivered at communities.
By 2015 MoHP aimed to provide all 5 types of
temporary FP methods at 60% of health post
(NHSP IP – II). Likewise the government also
planned to have regular VSC services available at
all district hospitals and selected PHCCs. However
only 18% of Health Posts were able to oer all
ve methods of FP in 2013 (STS) and this gure
increased to only 20% in 2014 (UNFPA, 2014). The
urban-rural disparity in access to services is also
huge, compared to 82.5% of health facilities in the
urban areas only 22.8% of health facilities in the
rural areas are currently oering all ve methods
of temporary contraceptive methods (UNFPA,
2014).
4
Annual Report, DoHS
MINISTRY OF HEALTH AND POPULATION
DEPARTMENT OF HEALTH SERVICES
MD
CHD
FHD
LMD
EDCD
PHCRD
NTC
NHTC
NPHL
NCSAC
NHEICC
DIVISION CENTER
CENTRAL HOSPITALS-8
REGIONAL HEALTH DIRECTORATE-5
SUB-REGIONAL
HOSPITAL-2
REGIONAL
TRAINING CENTER-5
REGIONAL
MEDICAL STORE-5
REGIONAL
TB CENTER-1
ZONAL HOSPITAL-10
DISTRICT PUBLIC HEALTH
OFFICE-16
DISTRICT/OTHER
HOSPITALS-72
DISTRICT HEALTH
OFFICE-59
PRIMARY HEALTH CARE CENTER/
HEALTH CENTER-207
HEALTH POST-1,689
SUB-HEALTH POST-22127
FCHV
50,007
PHC/ORC CLINIC
12,608
EPR OUTREACH CLINIC
16,746
REGIONAL
HOSPITAL-3

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
8
To facilitate access to FP services, the GoN
supported integration of FP in post-partum,
post-abortion services, immunization program
and promoted expansion of service sites oering
long acting methods. At least ve methods of
contraception were available in 91.4% of health
facilities providing safe abortion services (STS,
2013) while only 30% of women accepted any one
method of contraception aer an abortion (HMIS,
2013). Lack of proper counseling on FP during post-
partum and post abortion visits contributed to
low uptake of modern contraceptives. According
to NDHS, 91% of post-partum women and 56 %
of women who had abortion were not provided
counseling on family planning. Although causes
of low contraceptive use among women in post-
abortion and post-partum period need to be
analyzed further, one obvious reason is poor
quality of counseling on family planning. Poor
quality of counseling is an issue for private and
NGO sectors as well as demonstrated by NDHS
(2011).
Quality of service plays key role in accepting,
rejecting and discontinuation of FP services.
Overall, 51 percent of contraceptive users
discontinued using a method within 12 months
of starting its use (NDHS, 2011). Twenty-six
percent of episodes of discontinuation occurred
because the women’s husbands were away,
12 percent was due to the fear of side eects or
health concerns, and 5 percent because the woman
wanted to become pregnant. The most common
discontinued modern method was oral pills. Fear
of side-eects and health concerns can be reduced
through quality counseling that would also enable
a couple or a woman to make informed choice
of contraception. However, only 63% of women
using contraception received full information
on possible side-eects and 59% of them were
informed on what to do if they experience side
eects. Percentage of those who were informed
about side eects was the lowest among women
who chose oral pills and female sterilization.
MoHP/FHD has invested in improving quality
of care through various interventions such as
establishing competency based training, and
training on infection prevention, conducting
comprehensive FP training for all level of service
providers and establishing/strengthening FP
service center. However, these eorts require
a long-term support including investments to
have sustainable results. A systematic approach
for improvement of quality of care including
systematic review and update of clinical protocols
and guidelines at national and clinic level,
developing indicators on quality assurance,
monitoring compliance with standards and
clinical audit for solving problems through a team
approach are needed to be in place. Education of
communities about clients’ rights and solicitation
of clients’ feedback on a regular basis need to be
embedded in quality improvement process.
Capacity of service providers
Trained, competent and condent human
resource is vital for providing integrated quality
FP services. The GoN has started implementation
of the Human Resource for Health -Strategic
Plan (2011-2015) to address challenges and
constraints related to distribution of skilled
human resources for health. However, health
facilitates at districts and primary health levels
still experience signicant shortage of health
providers, particularly obstetrician/gynecologists
and nurses (STS, 2013). The lack of skilled health
providers, especially female health professionals,
inhibits access and use of family planning. (PEER
study, 2012). Existing challenges with lack of
long-acting reversible methods or interruptions
in supply in most sites are mainly due to lack
of trained health providers (STS 2013). In some
cases, misconceptions and negative perceptions
harbored by healthcare providers themselves
limits individuals’ access to FP services of their
choices. In order to increase understanding of
health managers and services providers about the
role of FP for improving women’s health especially
within the integrated service delivery modality
and strengthen skills of service providers, support
for continuous capacity building is vital.
Family Planning training is institutionalized in
the country and delivered through a nationwide
network of training health sites under the
National Health Training Center (NHTC). The
national training plan, developed in co-ordination
with the Family Health Division, needs to be
timely implemented. A challenge is insucient
pool of trainers and coverage of service providers
including those from private sector. There is also

9
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
a need to institutionalize certain training like
postpartum FP counseling and postpartum IUCD
and to establish an integrated mechanism for post-
training follow-up and supportive supervision.
Another key area is to update training curricula
and make it available as e-learning modular
course to reduce o-site training duration and
thus absenteeism from work, in addition to
covering more service providers.
Contraceptive commodities and
logistics
In Nepal Government procures most of the FP
commodities required for public sector and
oen for NGOs. In 1993 MoHP established
Logistics Management Division (LMD) to manage
procurement and logistics management of all
health commodities including contraceptives.
Under the leadership of LMD national capacity
on forecast, purchase and distribution of
commodities has been signicantly improved in
the country. According to the FARHCS (UNFPA,
2014), “no stock out” of male condoms, oral pills
and injectable was reported in 100% PHCCs
and SHP; and 99% of hospitals and 99% HPs. In
addition 80% of PHCCs and 72% of HP had no
stock out of IUCD and implants.
Recognizing an increased demand for long-acting
methods, MoHP/FHD has aimed to increase
access to these methods in all health posts and
primary health care centers by end of NHSP II
(2015). However, the services are available only
in limited sites due to lack of supplies and skilled
personnel.
Factors contributing to stock outs of contraceptives
at all levels of service delivery include long
bureaucratic policies and procedures to purchase
commodities. Likewise supply of commodities
from regional stores to district and from district
stores to health facility level is oen interrupted.
In cases when facilities have stock outs of IUCD
and implants, it is mainly due to lack of trained
health sta to provide services and as a result no
request for the commodities
Strengthening FP service seeking
behavior
Knowledge of contraceptive methods is an
important factor for increasing uptake of FP
services. Radio, television and posters are three
main channels for FP messages that the majority
of the population has been exposed to. Modern
methods are more widely known than traditional
method. Although most people have heard about
at least one modern method of contraception
(NDHS, 2011), this does not represent existence,
among the entire population, of knowledge that
is comprehensive enough to allow individuals
and couples to choose and use FP services.
This is demonstrated by However, uptake of
modern contraceptives is hindered by existing
misconceptions, myths and fear of side eects.
Culture and religious ties such as a strong son
preference, religious beliefs and concerns about
side-eects (PEER Study 2012) also serve as
substantial barriers to increasing the Modern
Contraceptive Prevalence Rate (mCPR).
Regardless of almost universal knowledge about
contraception, married adolescents (15-19 years
old) has the lowest demand satised by modern
methods among all age groups (24.3), while their
unmet need for spacing is the highest (37.5).
Married women whose husbands are away
discontinue using contraception but in many cases
fail to use FP when reunite with spouses.
Men play a signicant role in decision making
on family planning. Engagement and education
of men about FP is crucial for reducing unmet
need for family planning, especially for modern
methods. Myths about contraception still exist
among men. For example, about 20 percent of men
think that women who use contraception may
become promiscuous. Men living in rural areas,
the Terai, and the Western region, particularly the
Western hill sub-region, are more likely to have
these perceptions than other men. Men with SLC
and higher level of education and those in the
highest wealth quintile are less likely to have these
misconceptions regarding contraceptive use than
other men.
Targeted communication and behavior change
approaches are needed to address the existing
challenges especially among adolescents
and migrants’ population. Increasing men
involvement in FP will benet elimination of
myths and encouragement of service seeking
behavior among women. Likewise demand and

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
10
utilization of FP services among special groups like
postpartum mothers, Muslims and disadvantaged
groups also need to be improved through targeted
interventions.
Advocacy for family planning
While the overall policy environment for FP is
positive, including the incorporation of FP/RH
into the GoN’s development and national health
programmes, the government’s strong policy and
strategy commitments have not been accompanied
by an equally commensurate dedication of
national nancial resources to meet the full
need for FP program and contraceptives. Some
decision makers, managers and service providers
are of view that FP is a mature program in Nepal
and hence does not need as much aention as
new programs require. Such perception has to
some extent negatively inuenced nancial and
programmatic commitments to FP. In addition,
advancing FP requires a multi-sectoral approach
which means that engagement of other sectors
such as education, youth, nance, women
and social welfare, transportation needs to be
strengthened.
Another aspect of creating enabling environment
for FP is to ensure that policies and legislations
are in place to facilitate access to services for most
vulnerable populations such as adolescents and
young people, women from poor selements
(urban or rural) and ethnic minorities. Although
the GoN has in place policies and regulations
related to safe motherhood, SRH and FP services,
a regular update and communication of such
policies to all relevant stakeholders, duty bearers
and right-holders alike is needed to scale up FP.
Gender equality and cultural factors play a
signicant role in making decisions on uptake
of contraceptives among women and especially
girls. Advocacy interventions need to be in place
to address men engagement in family planning,
role of religious leaders and other community-
gatekeepers.
Management, monitoring and
evaluation
Clear leadership responsibility and authority are
essential for scaling up FP in the multi-sectoral
environment. Current bolenecks in supervision,
monitoring, and evaluation include limited
dedicated stang resources at the national and
district levels as well as insucient capacity
to utilize available data and implement current
guidelines and other tools. A need for strengthened
co-ordination at central, regional and districts
levels both within the government system as well
as with external development partners cannot be
over-emphasized.

11
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Projecting Population Growth
and Method Mix to Scale up
Family Planning
To scale up FP in Nepal, demand satised for
modern contraceptives is modelled to reach 62.9%,
which reects on Contraceptive Prevalence Rate
(CPR) and unmet need. CPR for modern methods
will reach 50% and unmet need will be reduced
to 22 % by 2021. At this rate of contraceptive
use, TFR will be at 2.1 births per women, which
represent replacement level.
This target may appear relatively modest but was
chosen to reect the context of Nepal: a country
that has made impressive gains in FP, but which has
experienced a stalling CPR more recently, as well
as signicant variations in use by age, geographic
region, wealth quintile and spousal separation.
The target therefore reects a FP strategy that aims
to give women a choice in contraceptive method
and to reach poor, vulnerable and marginalised
groups. The strategy is also to make changes in
the method mix over time, with a balance between
permanent, long-acting reversible methods and
short-acting methods. Previous analysis by the
Nepal expert working group served as the basis
for these changes, which reect historical trends,
shown in Table 1.
Table 1: Changes in Method Mix
2015 2020 2025 2030
Pill 8.3% 8.3% 8.3%
8.3%
Condom 8.9% 9.1% 9.3%
9.5%
Injectable 18.7% 18.9% 19.1%
19.3%
IUD 3.1% 3.7% 4.4%
5.0%
Implant 3.2% 4.2% 5.2%
6.2%
Male sterilisation 15.7% 15.7% 15.7%
15.7%
Female sterilisation 29.1% 27.0% 25.0%
22.9%
Traditional 13.1% 13.1% 13.1%
13.1%
Total 100.0% 100.0% 100.0%
100.0%
Source: OPM calculations based on Nepal working group projections and NDHS 2011.

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
12
National Costed
Implementation Plan
for Family Planning
Purpose
Recognizing the need to revive and scale up FP
in Nepal, the Government has developed the
Costed Implementation Plan (CIP) on FP. The
development of the plan has been guided by the
strategic directions developed through extensive
consultations with relevant stakeholders at
national, regional and district levels and is in line
with the National Health Sector Program (NHSP
III 2015-2020) which is currently being nalized. As
did the previous health sector plans (NHSP I and
II) the upcoming NHSP III has also recognized FP
as a priority, and it is considered as a component
of reproductive health package and essential health
care services.
The purpose of the CIP is to strengthen the
foundation for FP programming and service
delivery at national and districts levels as well as
to identify the activities to be implemented and
resources needed for achieving the results.
The CIP clearly denes priorities for strategic
actions, delineates the activities and inputs needed
to achieve them, and estimates the costs associated
with each as a basis for budgeting and mobilizing
resources required for implementation at dierent
levels by organizations and institutions over the
2015-2020 period. In addition, CIP is intended to
serve as a guide for development partners and
implementing agencies on areas of need to ensure
the success of the national FP program.
More specically, it will be used to:
l Inform policy dialogue, planning and
budgeting to strengthen FP as a priority area
l Prioritize strategies on FP to be adopted over
the next 6 years.
l Enable FHD, NHTC, LMD and NHEICC
to develop their respective implementation
plans with eective, ecient and actionable
interventions/activities and timelines
identied.
l Support Government and national partners
to understand nancial and technical support
needs for scaling up FP in the country.
l Support advocacy eorts for FP with clear
messages on impact of FP on health & non-
health sectors including cost-savings to justify
investments.
l Set benchmarks that can be used by the MoHP
and external development partners to monitor
and support the national FP programme.
Vision
Healthy, happy and prosperous individuals and
families through fulllment of their reproductive
and sexual rights and needs
Goal:
Women and girls - in particular those that are
poor, vulnerable and marginalised – exercise
informed choice to access and use voluntary FP
(through increased and equitable access to quality
FP information and services).
Strategic action areas and objectives
The strategic objectives reect the issues and
challenges in FP that have to be addressed in
order to scale up FP interventions in the country
to reach the goal. The strategic objectives of the
CIP ensure that limited available resources are
directed to areas that have the highest need to
reduce the unmet need for FP in Nepal. In the case
of a funding gap between resources required and

13
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
those available, most eective activities should
be prioritize to ensure the greatest impact and
progress towards the objectives laid out.
Strategic Action Area and Objectives:
The Costed Implementation Plan on FP has ve
strategic areas for action to achieve its objectives
in order to scale up FP in the country with a focus
on rights of women and girls.
l Enabling Environment: Strengthen enabling
environment for family planning
l Demand Generation: Increase health care
seeking behavior among population with
high unmet need for modern contraception
l Service Delivery: Enhance FP service delivery
including commodities to respond to the needs
of marginalized, rural residents, migrants,
adolescents and other special groups.
l Capacity Building: Strengthen capacity of
service providers to expand FP service
delivery network
l Research and Innovation: Strengthen evidence
base for eective programme implementation
through research and innovations
General Programme Management:
Programme Management is an essential component
of managing and overseeing the implementation
of activities that the accelerated scale-up plan
envisages. In short, programme management is
critical for ‘pulling everything together’ and to make
sure that each component of the programmatic
interventions is working as it should and is aligned
and coordinated with the full range of interventions.
General Programme Management covers the
full costs of the government personnel required
to implement programmatic activities, at the
Central Level (FHD) and District/ Regional
Level. The resource requirements / costs that are
involved estimate the number of stas by cadre
for whom FP activities constitute a signicant
share of their daily work and then combine
this with information on the share of their time
allocated to FP and information on salaries /
allowances. Estimated resources required for
general programme management to implement
the Costed Implementation Plan are shown in
Annex B.
Each Strategic Action Area and General
Programme Management has a set of costed
activities. The activities were generated, under
the leadership of FHD, through Key Informant
Interviews and several rounds of consultations
at central, regional and district levels involving
a wide range of stakeholders in the government,
donor communities, civil societies, professional
organizations, social marketing and private
sector. Cost estimation of the activities including
commodities was done by an expert group
including the Technical Working Group (TWG)
member. The estimated costs that emerged were
then reviewed by Oxford Policy Management
(OPM) and technical experts at UNFPA
Headquarter. This review involved ensuring that
the strategic interventions planned are in line with
global recommendations and best practices. OPM
also checked for and corrected calculation errors;
Scaling down observed over-estimates for certain
Table 2: Estimate of total resource requirements (millions)
2015 2016 2017 2018 2019 2020 Total
NPR
Total
USD
Direct intervention
costs
1,229.6 1,258.9 1,289.3 1,336.1 1,365.8 1,363.6 7,843.3 87.9
57%
Programme costs 1,099.3 1,094.5 860.6 780.4 456.2 506.8 4,797.7 53.8
35%
Indirect costs 172.7 178.6 184.4 190.3 196.3 201.9 1,124.1 12.6
8%
Total 2,501.6 2,531.9 2,334.3 2,306.8 2,018.4 2,072.2 13,765.2 154.2
Year as % of total cost 18% 18% 17% 17% 15% 15% 100%
Source: Multi-Year Costed Implementation Plan, OneHealth modeling and OPM calculations

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
14
activities; and Removing medical equipment and
facility rehabilitation costs in order to eliminate
double-counting.
As shown in Table 2 the total resources required
for scaling up FP in Nepal are $ 154.2 million for
six years that include:
1. Direct intervention costs - commodities and
supplies and medical personnel (constituting
57% of the total cost).
2. Programme resources – activities at the wider
population level that are required for an
intervention to be implemented eectively
(constituting 35% of the total cost).
3. Indirect costs – costs related to health facility
overhead costs such as administrative sta
and utilities bills (constituting 8% of the total
cost).
Estimates for all required resources are presented
in the Annexes.
Strategic Action Area: Enabling
Environment
A policy environment that enables the above
four Action Areas to be implemented eectively
is key for a successful FP programme. Strategic
interventions in this area include increasing
advocacy at all levels for FP; addressing legal
and socio-cultural barriers to young people
accessing FP; strengthening the integration of
services; and developing /updating national
polices and strategies to facilitate task shiing.
Estimated resources required to implement the
key interventions are presented in Annex C.
KEY INTERVENTIONS:
l Increase Advocacy for Family Planning.
Identify national champions for FP from
multiple elds and support them to advocate
for FP by providing advocacy materials/tools
and conducting follow up meetings. Develop
and distribute advocacy packages using global
evidences and tools, including modeling
exercises, (in English and Nepali) for key
stakeholders. Support high level advocacy
events at central level and districts engaging
parliamentarians, governmental ocials and
donors as well as civil society organizations
and media. Support advocacy events at
community level including celebration of FP
day at community level
l Address legal and socio-cultural barriers to
access to FP services for young people and
other special groups. Update the National
ASRH strategy & review implementation
of the strategy in 2019. Advocate with
Ministry of Education (MoE), Curriculum
Development Board (CDB) and key
stakeholders to incorporate Comprehensive
Sexuality Education (CSE) components in
curriculum for Grade 9-10. Develop a national
strategy on increasing access to voluntary FP
services among disabled people and support
its implementation ensuring multi-sectoral
co-ordination and collaboration.
l Advocate for integration of FP services.
Support development of national FP service
integration strategy as part of the CIP for FP
and NHSP III. Based on the strategy, develop
operational guidelines and disseminate them
at all levels of service delivery.
l Promoting task shiing and sharing. Develop
a national strategy on task shiing/sharing.
Strategic Action Area: Demand
Generation
The variation in the unmet need for FP in Nepal
is an indication of signicant scope for increasing
access to FP, although it is also an indication that
demand for FP services is not uniform and that
promoting such access will require specic and
targeted eorts. Demand generation strategy will
focus on strengthening health service seeking
behavior especially among adolescents and young
people and marginalized populations.
Demand generation eorts will focus on targeted
approaches to reach adolescents in and out of
schools especially in urban areas; reduce fear
of side eects of modern contraception as well
as myths and misconceptions among women
and men; strengthen community based work to
provide full information on FP to marginalized
population and use innovative nancing to reduce
nancial barriers to the services. Estimated cost
of key interventions for Demand Generation is
presented in Annex D.

15
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
KEY INTERVENTIONS:
l Support integration and implementation
of Comprehensive Sexuality Education
(CSE) in schools secondary and higher level.
Support will be provided to fully implement
CSE curriculum in grades 6-10 and interactive
sessions with students in grades 11-12 will be
conducted. It will include advocacy with the
Ministry of Education, training of educators/
teachers and updating teaching materials and
other communication tools.
l Reach adolescents with FP messages using
innovative approaches. Support promotion
of FP among adolescents and young people
using SMS and mobile technology. Mobile
application on FP and health related issues
will be developed and introduced in
collaboration with phone companies with
a focus on adolescents and young people
needs. In addition a telephone hotline will be
set up to provide information on emergency
contraception and other SRH/FP related
issues to young people. A program on access
and use of contraceptives for adolescents
living in urban areas will be supported for six
years.
l Design, implement and evaluate special
programme to increase access and utilization
of FP among adolescents and young people. To
support access to contraceptives information
and services among adolescents and young
people, a peer education programme will be
developed and implemented both in- and
out-of school. Strengthen program design,
implementation and evaluation for Social
and behavior change communication, that
includes development of FP communication
strategy, development of IEC materials and
media messages, evaluation of FP Social and
Behavioural Change Communication (SBCC),
development of communication tools package
focused on the targeted groups and building
capacity of partners working in SBCC. Ensure
that BCC interventions address needs of
newly married young people to delay rst
pregnancy.
l Increase knowledge about FP among
individuals/couples to facilitate decision –
making on contraceptive use. BCC materials
will be developed to target specic groups
of population with higher unmet need
for modern FP methods. Communication
campaigns will be supported in 2015 and
2018.
l Reduce socio-cultural barriers to access
FP services. Support community-
based programmes on FP to strengthen
communication skills and capacity on FP
among FCHV and health workers.
l Reduce fear of side eects, myths and
misconceptions about FP through
various communication channels. Support
development of IEC materials that
emphasize value of daughters and clarify
information about modern contraceptives
to be used by FCHVs, health workers and
community leaders. Organize forums and
interactive sessions on clients’ satisfaction in
communities’.
l Develop and implement micro-plans for
specic groups. Districts’ micro-plans will
be developed based on existing evidence on
barriers to FP utilization among underserved
groups of population.
l Develop and implement a programme
focused on needs for FP among migrants
and their spouses. The programme will
provide information and services to returning
migrants and their spouses to prevent
unintended pregnancy. In addition integrated
information on preventing STIs/HIV and
unintended pregnancy will be provided to
migrants prior to their departure.
l Develop and implement FP programme
targeting hard-to-reach people. The program
will use national guidelines for reaching the
unreached population during development
of targeted programmes. This would include
a mapping exercise to identify communities
with high unmet need for FP followed by
designing of targeted approaches to reach out
to marginalized population with information
and counseling on FP through existing
mechanisms including community mobilizers.
The programme will be implemented in urban
slums as well as in rural areas. Total Market
Approach will be introduced to ensure that
underserved target populations have access

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
16
to contraceptives. A market segmentation
action plan will be developed.
l Provide information on FP to women in
post-partum and post-abortion period.
Support and strengthen group counseling
and provision of contraceptive information
for couples and women visiting Expanded
Program on Immunization (EPI) clinics
during vaccination days as well as promoted
counseling among women in postpartum
period in Health Mother Groups (HMGs).
Incorporate information on FP into
Comprehensive Abortion Care (CAC)
services.
Strategic Action Area: Enhancing
Quality Service Delivery
The key interventions are designed to increase
access to services, particularly for vulnerable
as well as hard to reach populations, and to
increase the quality of services being provided.
Such activities range from supporting NGOs
who are providing FP services to strengthening
coordination with the private sector to improve
access and quality of services. Among government
services activities designed to enhance service delivery
include improving services across all levels (FCHV/
Community Level; PHC/ORC clinics; SHP/HP/
PHCs, including birthing centres; District Zonal &
Regional and central level Hospitals) and enhancing
coordination at the central and district levels. It is
also designed to improve facility recording and
reporting, to strengthen the management capacity
of FP ocers and to establish a dedicated Quality
of Care unit. Additional activities will include
supporting Medical College Teaching Hospitals,
eorts to ensure contraceptive security and support
to strengthening social marketing and private
sector role.
Beer quality FP, greater coordination of FP
services, and an integration of the FP services
across government, NGO and private providers
combined with improvements in management
and quality assurance will go a long way to
enhancing the supply side of service delivery, thus
stimulate demand for and increasing the uptake
of FP services. Estimated resources required to
implement the key interventions are presented in
Annex E.
KEY INTERVENTIONS
l Improve FP integrated services at FCHV/
Community Level. Update FP orientation
package including post-partum FP for FCHVs
and conduct refresher training for FHCVs
using the updated FP training package. In
addition build capacity of FCHVs in conducting
pregnancy test, counseling on family planning,
antenatal care and post-abortion care. To
increase access to condoms, especially among
youth, support establishment of condom
boxes at appropriate places in community.
Mobilize and provide support to expand
access to long-acting reversible contraceptives
through satellite clinics and comprehensive
FP camps. Support South-South Cooperation
by organizing study-visits to countries with
successful and eective community based
programme son FP(e.g. Bangladesh, Indonesia)
l Improve services at PHC/ORC clinics.
Conduct rapid assessment of PHC/ORC
situation and develop 1-2 model PHC/ORCs
per VDC (high unmet need districts), later
to be static Service Delivery Points (SDP).
Strengthen capacity of urban health clinics to
deliver FP services (20 municipalities).
l Improve services at HP/PHCs, including
birthing centers. Support health facilities
with commodities (long-acting ad short-
acting methods) and ensure that communities
are properly informed about available services
though appropriate communication channels.
Launch a pilot programme on expanding use
of Post-Partum Intrauterine Contraceptive
Device (PPIUCD) in birthing centers. Promote
task-shiing to expand services especially in
districts with high unmet need.
l Improve services in District Hospitals.
Expand availability of all short and long-acting
reversible methods and one VSC method
by supporting procurement and supply of
contraceptives to district hospitals, conducing
capacity building events for health providers
and strengthening supportive supervision.
Develop the 24 Integrated Family Planning
Service Centers (IFPSCs) as comprehensive RH
clinics. Support development of district-level
FP micro-planning & commodity forecasting
including situation analysis and training.

17
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
l Improve services in Zonal and Regional
Hospitals. Strengthen integrated FP services
in multi-disciplinary hospitals by conducting
training, ensuring supportive supervision
and introducing clinical guidelines/protocols
on FP service provision. Expand training on
recanalization.
l Social marketing. Revive private provider’s
network and implemented interventions
through Private Public Partnership (PPP)
models for strengthening supply chain
commodity management.
l Support NGOs providing FP services. Revive
work of Non-Governmental Organization
Coordination Commiee (NGOCC) to
strengthen role of NGOs working in FP in
coordination of national FP programmes.
Support NGOs capacity building in family
planning.
l Support Medical College Teaching Hospitals
by establishing FP service centers in each
medical college and including LAFP training
in doctor and nurse pre-service curriculum.
l Strengthen coordination of private sector.
Ensure that guidelines are in place for
adequate coordination of reporting on FP
services provided by private sector.
l Improve integration of FP services with
other services like immunization, HIV,
Postpartum, Post-abortion, morbidities,
urban health. Develop national FP service
integration strategy and operational
guidelines to implement the strategy. Pilot
new integration approaches in 2016 and scale
up the eective models in following years.
l Improve facility recording and reporting.
Strengthen and update recording/reporting
system as well as coordination with HMIS.
Develop M&E tools for private providers that
are in line with HMIS tool
l Establish Quality of Care unit. Support
establishment of quality of care unit within
FHD.
l Improve Quality of Contraceptives. Continue
the process of raising awareness of the
importance of moving towards consistently
high levels of quality of contraceptives
across the whole method mix. This would
include developing a national strategy and
implementation plan to progress to a situation
in which all contraceptives are: of certiable
quality [WHO pre-qualication scheme as
desired global standard; national plan to
move towards improved national standards
for non-WHO prequalied RH medicines].
l Strengthen management capacity of FP
Ocers. Support development of training
curriculum for building capacity of FP ocers
following by series of training and evaluation.
l Support contraceptive security. Strengthen
coordination with LMD and capacity in
Supply Chain Management (SCM) at all
levels.
l Enhance coordination at the central and
district levels. Support coordination
mechanism at central and district levels to
implement the FP interventions.
Strategic Action Area: Capacity
Building
Capacity building is a critical component of
ensuring that current stas (managers and health
care providers) are equipped to operate more
eciently and more eectively. Capacity building
also provides for the realisation of cost-savings
in the longer-term through task-shiing and
task sharing activities. Such activities are going
to be crucial if Nepal is to reduce unmet need
and ultimately eliminate the existing inequalities
in family planning. Estimated costs of key
interventions are shown in Annex F.
KEY INTERVENTIONS
l Strengthen training on contraceptive
technology for service providers. Update
training curriculum on all FP methods for
service providers. Support national training
centers in developing training plan with
travel schedule to cover all levels of service
providers and ensure availability of printed
training materials. Conduct trainings for
enhancing service delivery, particularly on
provision of quality FP counseling services.
Support development and introduction of
e-learning modality on family planning.
l Task-shiing/sharing of Non Scalpel
Vasectomy (NSV) training. Support training
of Health Assistants (HA) on NSV for task
shiing/sharing.

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
18
l Strengthen national FP training capacity
by renovating/upgrading/maintaining the
existing FP clinical training sites, including the
Regional Health Training Centers (RHTCs).
Support establishment of new training sites
where need exists.
l Development of pool of FP trainers. Support
Clinical Training Skill (CTS) training; prepare
clinical mentors in FP. Ensure availability
of physician trainers and nurse trainers on
family planning.
l Recanalization training, Strengthen and
expand recanalization training (including
microsurgery skills).
l Strengthen Post training follow up. Support
trained service providers to practice new
skills by establishing/strengthening regular
follow up system.
Strategic Action Area: Research and
Innovation
Research and innovation are key components
of programming. The Research & Innovation
activities included in the scale-up of FP services
costed in this analysis deal with specic areas of
the FP programme and are intended to contribute
to eorts at improving outcomes; of iterating
to nd more eective and less costly means
of reaching more patients with beer quality
services in a shorter period of time. Estimated
costs of research and innovation interventions are
presented in Annex G.
KEY INTERVENTIONS:
l Generate evidence through operational
research, to promote innovations in FP.
Support implementation research to understand
the factors that lead to discontinuation
of contraceptives including Long-Acting
Reversible Contraceptive (LARC) as well as
factors aecting FP care-seeking behavior
among poor urban residents. Document cases
of unintended pregnancy among Female Sex
Workers (FSWs) including on incidence, causes,
consequences and complications. Conduct
analysis of barriers for FP uptake among specic
communities, including youth and hard-to-
reach population. Evaluate m-health approach,
which is being implemented for reaching
adolescents with FP information. Support a
feasibility study on use of social media and
health-apps for FP messages with focus on youth.
Evaluate the existing program on Postpartum
FP and PP-IUCD and make recommendation
for national level implementation in 2015,
conduct a review of the national program aer
2 years of implementation. Conduct periodic
reviews/evaluations of FP program (specic for
advocacy and demand generation activities).
Market segmentation study to describe the
current market and service providers for FP.
Support formative research on task-shiing;
LARC, quality of care of integrated services, etc.

19
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
scaling up family planning
Demographic impact
TOTAL POPULATION
Figure 6 shows total population projections for
Nepal. Under the counterfactual scenario, the total
population is projected to rise to almost 33.5m by
2030. In contrast, the total population is projected
to reach just over 32m by 2030 under the FP scale-
up scenario. Population estimates from the latest
UN World Population Prospects (green dots) are
given as reference points for the available years of
2013 and 2025.
FIGURE 6: Total population projections for Nepal
(2011-2030)
35,000,000
34,000,000
33,000,000
32,000,000
31,000,000
30,000,000
29,000,000
28,000,000
27,000,000
26,000,000
25,000,000
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
2026
2027
2028
2029
2030
Counterfactual FP scale-up UN WPP
DEPENDENCY RATIO
In addition to a slower rate of population growth
under the FP scale-up scenario, our modelling
also shows important projected changes to the age
structure of the population. Table 3 gives various
dependency ratios, a key indicator of changing
population dynamics. The (total) dependency
ratio is declining over time under both scenarios;
however the decline is more rapid under the FP
scale-up scenario, with 58 children and older
people for every 100 working age people in 2030
compared to a counterfactual of 63. A lower (total)
dependency ratio means that there are fewer
children and older people for every working age
person, and therefore less of a burden to support
those who are oen economically dependent,
allowing for greater investment to be made in
ensuring that each child is educated, healthy
and has the opportunity to develop the skills to
contribute to a more prosperous society.
The (total) dependency ratio can be disaggregated
into the youth dependency ratio and the old-age
dependency ratio. As would be expected, the
decline is almost entirely being driven by the
Table 3: Dependency ratios
2015 2020 2025 2030
Total dependency ratio (A+B)
Counterfactual
0.70 0.64 0.62
0.63
FP Scale-up 0.70 0.63 0.59 0.58
Youth dependency ratio (A)
Counterfactual 0.55 0.49 0.46 0.45
FP Scale-up
0.55 0.48 0.43
0.40
Old-age dependency ratio (B)
Counterfactual 0.14 0.15 0.16 0.18
FP Scale-up 0.14 0.15 0.16 0.18
Source: OneHealth modelling

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
20
decline in the youth dependency ratio (fewer
children for every working age person) than any
change in the old-age dependency ratio (fewer
older people for every working age person). In
fact, the old-age dependency ratio has started
to rise by 2030. The demographic dividend that
could potentially be catalysed by a lower (total)
dependency ratio is quantied and discussed
further in the subsequent sections.
DEMOGRAPHIC DIVIDEND
Under certain social and economic circumstances,
having a larger proportion of the population of
working age can lead to economic benet. Figure
7 illustrates the demographic dividend that could
be catalysed by lower fertility rates if other policies
are also in place. It shows the ratio of projected
income per capita for the FP scale-up scenario
compared to the counterfactual scenario. Income
per capita is projected to be 4.6% higher by 2030.
This demographic dividend is coming about
primarily from the lower dependency ratio but
also from increased labour force participation
by mothers, as well as, in the later years, higher
savings, investment and productivity. This is not
included in these benet-cost calculations because
it is not a guarantee. It will not come about from
scaling up FP alone but requires investment in
other areas—in particular, education, health,
governance and the economy more widely—to be
realised.
1.1000
1.0800
1.0600
1.0400
1.0200
1.0000
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
2026
2027
2028
2029
2030
FP Scale-up compared to Counterfactual Scenario
FIGURE 7: Increase in income per capita
COUPLE YEARS OF PROTECTION
The number of couple years of protection (CYPs),
which is a function of both population growth
and increased contraceptive use, is estimated
at 2.9 million by 2030 under the FP scale-up
scenario, which is 0.24 million more than under
the counterfactual scenario.
MATERNAL HEALTH
The health benet of scaling up FP services is
positive. The modelling shows that there are
projected to be 230 fewer maternal deaths a year
by 2030 under the FP scale-up scenario compared
to the counterfactual scenario. The maternal
mortality rate is projected to decrease to 18.1 in
2030 under the FP scale-up scenario compared to
the counterfactual scenario of 20.8 in 2030. (Figure
8) It should be noted that this is a conservative
estimate of the impact on maternal mortality. This
is because there is not enough of an evidence base
to robustly quantify the impact of FP scale-up
through other channels such as higher levels of
maternal education.
25
20
15
10
5
0
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
2026
2027
2028
2029
2030
Counterfactual FP scale-up
FIGURE 8: Maternal mortality rate
INFANT AND CHILD HEALTH
There is currently not enough of an evidence
base to robustly quantify the impact of FP on
infant and child mortality. However, if we adopt
the approach taken by the Gumacher Institute
in its Adding It Up report and simply apply
the current Infant Mortality Rate (IMR) to the
estimated number of births in each scenario, then
by 2030 there would be approximately 3,000 fewer
infant deaths a year in the FP scale-up scenario
compared to the counterfactual scenario. This is
a conservative estimate given that FP not only
reduces the number of births but reduces the
chance of children dying in their rst year.
In terms of child mortality, FP can help a woman
space her births. One study has found that child
mortality can be reduced by 13% with birth
spacing of two years or more and 25% with birth
spacing of three years or more (Rustein, 2008). The
Gumacher Institute in its Adding It Up report
21
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
does not quantify this in terms of child deaths
prevented and so we do not include that here.
Slower rates of population growth and healthier
population translate into sectoral cost savings
as there are fewer people who need education
and health services. In this section, the benet is
quantied in terms of:
• Fewer children age 6-10 requiring primary
education;
• Fewer children under age 1 requiring
immunisation;
• Fewer children under age 5 being treated for
pneumonia;
• Fewer mothers requiring maternal health
care; and
• Fewer people requiring access to clean
drinking water.
Table 4 shows the cumulative cost savings (2015-
2030) in primary education, child immunisation,
child pneumonia, maternal health and the
Water, Sanitation and Hygiene (WASH) sectors
under the FP scale-up scenario compared to the
counterfactual scenario.
Table 4:
Sector Not
discounted
(NPR million)
Discounted
at 3% (NPR
million)
Primary
education
20,231.9 13,629.0
Child
immunization
10,057.0 7,530.4
Child
pneumonia
1,865.2 1,384.7
Maternal health 13,511.9 10,081.9
WASH 904.0 641.1
Total 46,569.9 33,267.1
Source: OPM calculations
Both scenarios assume universal primary education
by 2021, at a unit cost of 10,000 Nepalese Rupees
(NPR) per child. Under the counterfactual scenario,
primary education spending would increase from an
estimated 29,127.9m NPR a year in 2015 to 30,215.6m
NPR a year in 2030, whereas under the FP scale-up
scenario, it would only increase to 26,219.8m NPR a
year in 2030. The cumulative savings over the period
of 2015-2030 would be 20,231.9m NPR, or 13,629.0m
NPR if discounted at 3%.
Both scenarios assume that all children receive a
full set of basic vaccinations by age 1 by 2021 at a
unit cost of 9,187 NPR per child, at a total cost of
6,089.9m NPR a year by 2030 in the counterfactual
scenario but only a cost of 5,271.1m NPR a year in
the FP scale-up scenario. The cumulative savings
over the 2015-2030 periods would be lower than
that of primary education at 10,057.0m NPR, or
7,530.4m NPR if discounted at 3%.
Other cost savings in the health sector include
those related to child pneumonia and maternal
health. Assuming that by 2021, Nepal has reached
the target of 80% of children with suspected
pneumonia are taken to the appropriate health
provider (as in Bhua et al, 2013), total costs
for treatment of children under 5 with severe
pneumonia would reach 1,012.3m NPR a year
by 2030 in the counterfactual scenario but only
876.6m NPR a year in the FP scale-up scenario.
The cumulative savings over the period of 2015-
2030 would be 1,865.2m NPR, or 1,384.7m NPR if
discounted at 3%. It should be noted that to prevent
double counting with other sectors, only the costs
of treating severe pneumonia are included in the
calculation, not the broader costs of preventative
interventions for pneumonia.
The unit cost of universal maternal health provision
is higher at an estimated 12,206 NPR per birth and the
cumulative cost savings are correspondingly higher,
even though there is more children under-5 than
new mothers in a year. The cumulative cost savings
over the period of 2015-2030 would be 13,511.9m
NPR, or 10,081.9m NPR if discounted at 3%. Annual
costs would reach 8,324.7m NPR by 2030 under the
counterfactual scenario and 7,205.7m NPR by 2030
under the FP scale-up scenario.
Finally, assuming that the proportion of people
with access to an improved water source increases
so that universal coverage is reached by 2021, total
costs would reach 3,904.7m NPR a year in 2030 in
the counterfactual scenario and 3,777.5m NPR a year
in the FP scale-up scenario. This smaller discrepancy
in cost is because universal coverage is assumed
to have been reached by this time, and continuing
to supply water to people is less expensive than
connecting them in the rst place. The cumulative
cost savings over the period of 2015-2030 would be
903.0m NPR, or 641.1m NPR if discounted at 3%.

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
22
Figure 9 shows these cumulative cost savings over
time. The main point to note here is the timing
of the cost savings in the dierent sectors: in
particular, cost savings in primary education take
some time to materialise because it takes 6 years
for the impact of FP on the population age 6-10 to
occur. However, by 2030, cumulative cost savings
are the largest for primary education.
Investment requirements
PROJECTED TOTAL COSTS
Figure 10 shows the expenditure required to
reach the FP scale-up scenario compared to the
counterfactual scenario. Costs are in constant 2014
NPR, thus showing the results without ination
and, for the USD total, without exchange rate
uctuations. Whereas additional total expenditure
is estimated at 1,081.8 million NPR a year in 2015,
because programme expenditure is front-loaded,
the model projects additional costs declining to 671.7
million NPR a year in 2020.
3,000,000,000
2,500,000,000
2,000,000,000
1,500,000,000
1,000,000,000
500,000,000
0
2015
2016
2017
2018
2019
2020
2021
2022
2023
2024
2025
2026
2027
2028
2029
2030
Counterfactual FP Scale-up
FIGURE 10: Projected expenditure under the FP
Scale-up and Counter factual scenarios capita
FIGURE 9: Cumulative cost savings
25,000,000,000
20,000,000,000
15,000,000,000
10,000,000,000
5,000,000,000
0
2014 2015 2016 2017 2018 2019 2020 2021 2022 2023 2024 2025 2026 2027 2028 2029 2030
Primary education Child immunization Child pneumonia Maternal health WASH
Table 5 shows that in the FP scale-up scenario cost
per CYP is 894 NPR in 2015 and declines to 693
NPR in 2020, rising somewhat to 845 NPR in 2030.
Cost per user follows a similar paern, starting at
853 NPR in 2015 and declining to 616 NPR in 2020
in rising to 667 NPR in 2030.
Table 5: Cost per CYP and cost per user
2015 2020 2025 2030
Cost per CYP
Counterfactual 583 590 586 586
FP Scale-up 894 693 843 845
Cost Per User
Counterfactual 494 467 481 480
FP Scale-up 853 616 660 667
Source: One Health Modelling
In theory, it should be possible to compare our
unit cost estimates (i.e. cost per user and cost per
CYP) with those produced by other studies. For
example, our annual cost per user estimate in
the FP scale-up scenario is higher than 388 NPR,
which the Gumacher Institute’s estimate for Asia
as a whole (Singh and Darroch, 2012). However,
our estimate includes a comprehensive costing of
the programme costs required to achieve this scale
up whereas many other cost-benet analyses of
FP programmes consider only direct intervention
costs. We adopted this approach because we
believe that it provides a far more realistic picture
of all the costs involved in scaling up FP coverage.

23
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Return on investment
The most commonly reported summary metric
of a cost-benet analysis is the Benet-Cost Ratio
(BCR). This simply divides total discounted
benets by total discounted costs. A BCR of greater
than one therefore means that the benets of the
programme outweigh its costs. It is important to
note that, as with all economic evaluations, there
is an implicit counterfactual built into the BCR; in
this case, it reports the benets and costs to the
FP scale-up scenario that are incremental to the
Counterfactual scenario.
The net present value of a programme is another
commonly reported metric. This is total discounted
benet minus total discounted costs to give the net
benet of the programme. For this metric, benets
outweighing costs is a value of greater than zero.
Table 6 gives the benet-cost ratio and net present
value at key time horizons for the FP scale-up
scenario relative to the counterfactual scenario.
These results all use a discount rate of 3% as base
case, which is standard practice for health sector
economic evaluation; in our sensitivity analysis,
we calculated these metrics at other discount rates
(5% and 7%), also shown below.
Table 6: Investment metrics
2020 2025 2030
3%
Benet- cost ratio 1.0 2.2 3.1
Net present value
(NPR Million)
-130 7,490 22,400
5%
Benet- cost ratio 0.9 2.1 2.9
Net present value
(NPR Million)
-230 6,130 17,500
7%
Benet- cost ratio 0.9 2.0 2.7
Net present value
(NPR Million)
-320 5,020 13,720
Source: OPM calculations
Looking at the longer time horizon (to 2030) and
at discount rate of 3%, for every rupee spent on
family planning, Nepal would save 3.1 rupees
in the ve sectors: primary education, child
immunisation, child pneumonia, maternal
health and WASH. This calculated by dividing
the net present benets of 33,267.1 million NPR
by the net present costs of 10,661.6 million NPR.
This is a conservative estimate of the return on
investment on FP for Nepal because we are only
including the cost savings to these sectors. There
are likely to be cost savings to other sectors not
included here – those related to health sector
(like improved pregnancy outcomes, reduced
unsafe abortion from unwanted pregnancies and
improved protection from HIV and other STIs)
and outside health sector (cost saving in providing
social services, climate change benets and
improvement in women’s right, empowerment
and gender equality . There are also other benets
that we have not included in our benet-cost
calculations.

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
24
The way forward
Institutional Arrangements for
Implementation
The Government of Nepal has responsibility
and leadership for ensuring that all women and
girls are enabled to make informed decision on
number and timing of having children through
providing universal access to quality FP services.
Operationally, implementation of the CIP requires
multi-sectoral approach in the coordination and
management of the national eort.
Based on stakeholders’ consultation, a streamlined
coordination and management structure is
proposed for CIP implementation as shown
in Figure 11. The purpose of the coordination
mechanism is to ensure multi-sectoral approach;
optimize nancial and technical support to
FP provided by donors/INGOs; ensure strong
linkages and coordination with NHSP III; support
eective implementation of the CIP and strengthen
engagement of NGOs and other stakeholders,
as well as to improve tracking/dissemination of
results and lessons learned.
l The coordination and management mechanism
is built on the existing coordination structure.
Implementation of the CIP will be steered
by MoHP (policy level) and coordinated by
DoHS, while the execution of CIP will be
overseen and managed under the leadership
of FHD.
l Reproductive Health Steering Commiee
(RHSC) at the MoHP will be engaged in
steering the CIP in order to ensure a multi-
sectoral approach for the CIP implementation.
To harmonize eorts on FP with national
interventions on preventing HIV and
ensuring gender equality, RHSC may include
representatives of commiees working on
gender issues and HIV.
l National Reproductive Health Coordination
Commiee (RHCC) will be engaged in
coordination of the CIP implementation
using the existing processes such as regular
meetings, updates, etc. Co-ordination and
collaboration amongst divisions and centres
particularly FHD, NHTC, NHEICC, LMD,
PHCRD, NCASC and CHD will be enhanced
for successful implementation of the CIP.
NGOs participation will be strengthened
though NGOCC.
l At the level of FHD, collaboration and
coordination between FP, ASRH, safe
motherhood and neonatal, Monitoring and
Research units will be strengthened through
existing for a particularly FPSC but also
through SMNSC and Research sub-commiee.
In addition through implementation of the
CIP, in particular, interventions related to
Reporting and Monitoring and Evaluation,
linkage with Management Division /HMIS
unit will be enhanced.
l Collaboration and coordination amongst relevant
stakeholders to implement and monitor the CIP at
regional and district levels will be accomplished
through Regional- RHCC (R-RHCC) and
District-RHCC (D-RHCC) respectively.
l Focal Points will be part of coordination
mechanism.
Policy level: Chief Policy, Planning and
International Cooperation Division
(PPICD) – facilitate coordination with line
Ministries and Partners
Coordination: Director General, DoHS –
ensure that other divisions are engaged in
the CIP FP implementation
Management: Chief of FP section, FHD -
ensure that the CIP is translated in AWP
and support districts to develop their plans
accordingly and support implementation
through the QI unit.
Regional Director – monitor
implementation of action plans at district
level
FP Supervisor – with support from D/
PHO and Public Health Nurse (PHN)
coordinate and support implementation
of the CIP FP at district and below levels
and provide feedback to FHD.

25
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
LINE
AGENCIES
MoF
NPC
MoE
NHTC
NHEICC
NCASC
LMD
MD
CHD
PHCRD
INSTITUTION
MoHP
RHSC
DoHS
FHD
RHD
D/PHO
RHCC
FPSC
NGOCC
COORDINATION
MECHANISM
R-RHCC
D-RHCC
FIGURE 11: CIP Coordination and Management
Structure
District-level Planning
The Ministry of Health and Population developed
the Costed Implementation Plan on Family
Planning to provide a roadmap for reaching 62.9%
of demand satised by modern contraceptives
which brings CPR for modern contraceptives up
to 50%. Reaching this goal will require signicant
district-level leadership and coordination in
the planning and implementation process. This
document provides a foundation and guidance
for designing district micro-plans.
This undertaking will require for each district
to conduct a situation analysis, and initiate a
planning process in close collaboration with all
partners. The 75 districts have dierent priorities
for FP and require dierent interventions. For
example, districts with a relatively high CPR
and high unmet need will require a dierent
strategy than those with a lower CPR and lower
unmet need. Beyond FP statistics, other factors
dierentiate districts and how FP must be scaled
up. For example, geographical access to services,
the care-seeking behavior among residents, level
of mass media exposure, availability of health
sta and community workers, etc.
Ultimately, districts will follow a similar process
to that of the MOHP in creating the CIP. Districts
and community level health managers and
health care providers will be enabled to develop
micro-plans in order to implement the national
costed implementation plan for family planning.
Microplanning for FP services is an innovative
approach that enables district managers and
healthcare providers to generate and analyze
local, disaggregated data; use them to identify
pockets of inequity within the districts, in terms
of both access to and utilization of FP services;
identify context-specic strategies/approaches
and implement them. MoHP/FHD initiated this
in 7 districts in 2014 with support from partners
including DFID and UNFPA and plans to expand
it, in a phase-wise manner, to other districts with
high unmet needs.
The planning process will follow the key steps such
as: engage the appropriate stakeholders, diagnose
specic priorities, set a district-wide goal for family
planning, dene the most appropriate interventions,
and create a detailed and costed plan. This process
will require substantial leadership at the district
level from the MoHP as well as other government
agencies and, crucially, the support of the governor/
other key stakeholders and champions.
District plans should build on existing FP
programmes and identify other health initiatives
and programmes for coordination or integration
in order to ensure the eective use of resources
and leveraging of opportunities to take advantage
of successful interventions.
Resource Mobilization
The national CIP estimates that more than US$
153 million is required to scale up FP in Nepal
by 2020. Although the CIP provides costs of key
interventions, it does not include information
about allocated funding. A review and analysis
of available domestic and donor resources for FP
should be conducted to identify a funding gap
and develop a resource mobilization plan.
The resource mobilization can address this funding
gap in two ways. First, allocate already commied
FP funds to the priority activities identied in the
CIP and if possible to have a multi-year funding
framework for all partners supporting FP in the
country. This will help ensure that current donor
funding and partner activities are aligned to the
greatest areas of need. Second, identify sources
for additional funding from local governments,
private sector and donors.
The costed national- and district-level
implementation plans will be used as key

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
26
advocacy tools to demonstrate both the needs for
and potential impacts of new funding.
The costed implementation plan (CIP) outlines the
GOAL:
Women and girls-in particular those that are
poor, vulnerable and marginalized- exercise in-
formed choice to access and use voluntary qual-
ity family planning services.
STRATEGIC OBJECTIVES:
a) To strengthen enabling environment for fam-
ily planning.
b) To increase health care seeking behavior
among population with high unmet need for
modern contraception.
c) To enhance family planning service deliv-
ery including commodities to respond to the
needs of marginalized, rural residents, mi-
grants, adolescents and other special groups.
d) To strengthen capacity of service providers to
expand FP service delivery network.
e) To strengthen evidence base for eective pro-
gramme implementation through research
and innovations.
RESULTS RELATED TO FIVE STRATEGIC AREAS:
1. Enabling environment
2. Demand generation
3. Service delivery
4. Capacity building
5. Research and innovation
OUTPUTS
OUTCOMES
IMPACT
Monitoring and
Evaluation Framework
goal, purpose, objectives and strategic directions
of family planning programme of Nepal for the
period of 2015-2020, with details of interventions
a n d c o s t s o f e a c h i n t e r v e n t i o n .
The scheme of the CIP is outlined as below:

27
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Monitoring and Evaluation Indicators
IMPACT INDICATORS
Goal Indi-
cator
code
Indicators Data
source
Respon-
sible
organiza-
tion
Moni-
toring
frequen-
cy
Disaggregation Baseline
value
2015
Target
value
2020
Women and
girls-in particular
those that are
poor, vulnerable
and marginalized-
exercise informed
choice to access
and use voluntary
quality family
planning services.
FPG1 Total fertility
rate
NDHS,
MICS
MoHP Five
years
Wealth quintile,
urban/rural,
eco-region,
ethnicity
2.5 2.1
FPG2 Adolescent
fertility rate
NDHS,
MICS
MoHP Five
years
Wealth quintile,
urban/rural,
eco-region,
ethnicity
81 per
1000
(NDHS,
2011)
70 per
1000
FPG3 Number of
unintended
pregnancies
averted
due to
contraception
use
Model
-
ing
FHD Five
years
Wealth quintile,
urban/rural,
eco-region,
ethnicity, age
NA TBD
FPG4 Number
of mater
-
nal deaths
averted due
to contracep-
tion use
Model-
ing
FHD Five
years
Wealth quintile,
urban/rural,
eco-region,
ethnicity, age
NA TBD
FPG5 Number of
abortions
averted due
to contracep
-
tion use
Model-
ing
FHD Five
years
Wealth quintile,
urban/rural,
eco-region,
ethnicity, age
NA TBD

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
28
OUTCOME INDICATORS
Outcomes Indi-
cator
code
Indicators Data
source
Re
-
spon-
sible
organi
-
zation
Moni-
toring
fre
-
quency
Disaggregation Baseline
value
2015
Target
value
2020
OC1. Strengthened enabling
environment for eective,
equitable and sustainable
family planning program
-
ming.
OC1.1 Percentage of total health bud-
get allocated for FP programme
Budget
analy-
sis
report
MoHP Annu-
ally
- NA TBD
OC2. Increase FP service
seeking behavior among
population with high
unmet need for modern
contraception.
OC2.1 Contraceptive prevalence rate
(disaggregated) (mCPR)
NDHS MoHP Five
years
Wealth quintile, urban/
rural, eco-region, eth
-
nicity, age
44.4 49.0
OC2.2 Percentage of demand satised
for Family Planning
NDHS MoHP Five
years
Wealth quintile, urban/
rural, eco-region, eth
-
nicity, age
65
(NDHS,
2011)
76
OC2.3 Percentage of women with a
unmet need for family planning
NDHS,
MICS
MD Five
years
Wealth quintile, urban/
rural, eco-region, eth
-
nicity, age
26.2 22.7
OC3. Improved and equi
-
table FP service delivery.
OC3.1 Percentage of demand satised
by modern method of contra-
ception (disaggregated)
NDHS MoHP Five
years
Wealth quintile, urban/
rural, eco-region, eth
-
nicity, age
55.9
(NDHS
2011)
62
OC4. Strengthened capac
-
ity of service providers to
expand FP service delivery
network.
OC4.1 Number/percentage of hos
-
pitals and PHCCs oering all
seven family planning services
Pro
-
gramme
report/
Health
facility
survey
FHD Annu
-
ally
PHCCs, hospitals TBD
OC4.2 Number/percentage of health
posts providing all ve tempo
-
rary methods of family planning
Pro-
gramme
report
FHD Annu
-
ally
- TBD
OC5. Improved availability
and use of FP evidence in
decision-making processes
at all levels.
OC5.1 Evidence of research/study rec
-
ommendations incorporated in
the national FP programme/ plan
Pro
-
gramme
report
MoHP Five
years
- - -

29
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Output Indicators
ENABLING ENVIRONMENT
Outputs Indicator
code
Indicators Data source Responsible
organization
Monitoring
frequency
Increased advocacy for family
planning
EE1 Number of FP sub-commiee meetings conducted Programme report FHD Annually
EE2 Number of awareness/advocacy events conducted Programme report FHD Annually
Legal and socio-cultural barriers
addressed to ensure increased
access to FP services
EE3 Development of national strategy on increasing ac-
cess to voluntary LAPM services
Programme report FHD Five years
EE4 National ASRH strategy updated Programme report FHD Five years
Integration of FP services at
all level of health care service
delivery
EE5 Development of national FP service integration strat-
egy and operational guidelines
Programme report FHD Five years
EE6 Clinical protocols, standards and guidelines for FP
services updated
Programme report FHD Five years
Task shiing in FP services
delivery
EE7 Development of a national strategy on task shiing Programme report FHD/NHTC Five years

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
30
DEMAND GENERATION
Outputs Indicator
code
Indicators Data source Responsible
organization
Monitoring
frequency
Integration of comprehen-
sive sexuality education in
education curriculum
DG1 Comprehensive sexuality education incorporated in
school curriculum
Programme report FHD/MoHP/
MoE
Five years
Increased access of adoles-
cents to FP messages
DG2 Number of adolescents and young people reached by
family planning promotion activities using SMS and
mobile technology
Programme report/
Survey report
FHD/NHEICC Annually
DG3 Number of districts with hotline counseling services
on FP/SRH
Programme report FHD Annually
DG4 Percentage of health facilities certied as being adoles-
cent friendly health facilities
Programme report FHD Annually
DG5 FP communication strategy updated Programme report FHD Five years
DG6 Communication tools developed to reach targeted
group (including newly married couples)
Programme report NHEICC Annually
Increased knowledge/evi-
dence to facilitate decision
making for FP
DG7 Rapid assessments of PHC/ORC conducted Programme report FHD Five years
DG8 Percentage of women with comprehensive knowledge
on at least one method of FP*
Survey report FHD Five years
DG9 Percentage of women who make family planning deci-
sions alone or jointly with their husbands
NDHS MoHP Five years
DG10 Percentage of men and women who were informed of
the permanence of sterilization
Survey report FHD Five years
Targeted FP programmes
developed and imple-
mented
DG11 Percentage of women who were provided with infor-
mation on FP during their last visit in health facility
Client exit survey
report
FHD Five years
* Comprehensive knowledge mean that the women had heard about the method, knows where to get it and how to use it.

31
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
SERVICE DELIVERY
Outputs Indicator
code
Indicators Data source Responsible
organization
Monitoring fre-
quency
Improved FP service delivery at
all levels
SD1 Percentage of WRA new acceptors by modern methods HMIS MD Annually
SD2 Couple years of protection (CYP) HMIS MD Annually
SD3 Number of comprehensive FP camps organized per dis-
trict
Programme
report
FHD Annually
SD4 Number of model PHC/ORC clinics developed Programme
report
FHD Annually
SD5 Number of hospitals providing recanalization services Programme
report
FHD Annually
SD6 Number of birthing centers providing post-partum intra-uter-
ine contraceptive device (PPIUCD) insertion services
Programme
report
FHD Annually
SD7 Percentage of women who received long acting family
planning contraceptives aer abortion
HMIS MD Annually
SD8 Percentage of safe abortion (surgical and medical) sites with
post-abortion long acting family planning services
Programme
report
FHD Annually
Improved FP integrated service
delivery (FP/EPI integration,
ASRH/FP integration)
SD9 Number of integrated RH service centers developed Programme
report
FHD Annually
SD10 Number of adolescents reached with RH programme HMIS MD Annually
Institutionalized quality of care in
FP service delivery
SD11 Quality of care unit established at FHD Programme
report
FHD Five years
SD12 Number of RHCC meeting conducted at the center and
district
Programme
report
FHD Annually
Improved recording and report-
ing systems across the sector
SD13 Number/percentage of registered private institutions
reporting on FP service data
HMIS MD Annually
Improved availability of quality
contraceptives at all health service
delivery points
SD14 Number/percentage of health facilities reporting no stock out
of FP commodities over the last three months
LMIS LMD Annually
SD15 Percent distribution of users of modern contraceptive
methods by most recent source of method, according to
method, Nepal 2011
NDHS MoHP Five years

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
32
CAPACITY BUILDING
Outputs Indicator
code
Indicators Data source Responsible
organization
Monitoring
frequency
Strengthened
training on
contraceptives
CB1 FP training packages updated Programme report NHTC Five years
CB2 National training package on long acting and permanent f FP methods
incorporated in the in-service curriculum of MDGP, DGO and MD (Gy-
necology & Obstetrics)
Programme report NHTC Five years
CB4 Number of health workers trained on LAPM Programme report NHTC Annually
CB5 Number of doctors trained on recanalization Programme report NHTC Annually
CB6 Number of paramedics trained on non-scalpel vasectomy Programme report NHTC Annually
CB7 Number of health workers trained on PPIUCD Programme report NHTC Annually
CB8 PPIUCD package incorporated into SBA package Programme report NHTC/FHD Five years
National
capacity on
FP training
enhanced
CB9 E-learning package on FP developed Programme report NHTC/FHD Five years
CB10 Number of functional FP training sites Programme report NHTC/FHD Annually
CB11 Number of new FP training sites established Programme report NHTC/FHD Annually
CB12 Percentage of FP trainees followed up Programme report NHTC Annually
RESEARCH AND INNOVATION
Outputs Indicator
code
Indicators Data source Responsible
organization
Monitoring
frequency
Operational research conducted to generate
evidences
RI1 Number of studies and researches
conducted on family planning
NHRC/Programme
report
FHD Annually
Use of FP evidences in plan and programme
development
RI2 National programme on FP reviewed Programme report FHD Five years
RI3 Number of successful innovations
scaled up at national level
Programme report FHD Five years

33
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
References
Ashraf, Q. et al (2013): The Eect of Fertility
Reduction on Economic Growth. Population and
Development Review, 39(1): 97—130.
Barne B. and J. Stein (1998): Women’s Voices,
Women’s Lives: The Impact of Family Planning,
Research Triangle Park, NC, USA: Family Health
International (FHI).
Cleland, J. et al (2006): ‘Family planning: The
unnished agenda,’ in Lancet 368, 1810-1827.
Department for International Development (2011):
Improving Reproductive, Maternal and Newborn
Health: Reducing unwanted pregnancies. Evidence
Overview.
Friberg, I. and B. Winfrey (2012): Understanding
how FamPlan calculates the numbers of abortions and
their impact on MMR in LiST. Futures Institute.
Government of Nepal (2007): National Development
Plan, 2007/2008–2010/2011.
Government of Nepal (2012): National Population
and Housing Census 2011 (National Report).
Government of Nepal. (2011) Nepal Population
Report 2011. Kathmandu, Nepal: Ministry of
Health and Population. Saugat Printing Press.
Gribble, J.N. and J. Bremner (2012): ‘Achieving a
Demographic Dividend,’ Population Bulletin 67
(2). Population Reference Bureau.
Heston, A. et al (2009): Penn World Table Version
6.3. Center for International Comparisons of
Production, Income and Prices at the University
of Pennsylvannia.
Huon, G. (2012) ‘Global costs and benets of
drinking water supply and sanitation interventions
to reach the MDG target and universal coverage,’
World Health Organisation.
International Labour Organisation (2011):
Economically Active Population, Estimates and
Projections (6th Edition). ILO Department of
Statistics, LABORSTA.
International Monetary Fund (2013): World
Economic Outlook.
James, C. (2012): The costs of delivering health services
in Tanzania.
Khanal M. N., Shrestha D.R., Panta P.D., and
Mehata S. (2013) Impact of Male Migration on
Contraceptive Use, Unmet Need, and Fertility in Nepal:
Further Analysis of the 2011 Nepal Demographic and
Health Survey. Calverton, Maryland, USA. Nepal
Ministry of Health and Population, New ERA,
and ICF International.
Mills, A. (1990): ‘The economics of hospitals in
developing countries,’ Health Policy and Planning,
5(3): 203-218.
Ministry of Health and Population Nepal
(2009): Mid-Term Review of the Nepal Health Sector
Programme Implementation Plan II (NHSP–IP
II), 2010 – 2015. Kathmandu, Nepal: Ministry
of Health and Population, Health & Education
Advice and Resource Team (HEART) and Oxford
Policy Management.
Ministry of Health and Population Nepal (2012):
Nepal Demographic and Health Survey 2011.
Kathmandu, Nepal: Ministry of Health and
Population, New ERA, and ICF International,
Calverton, Maryland.
Ministry of Health and Population Nepal (2009):
Nepal Health Sector Programme Implementation
Plan II (NHSP–IP II), 2010 – 2015
Ministry of Health and Population Nepal (2005):
The Second Long-Term Health Plan, 2006-2017.

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
34
Moreland, J. et al (2009): Achieving the Millennium
Development Goals in Kenya: The Contribution of
Family Planning. Paper prepared for the Population
Association of America 2009 Annual Meeting.
Rutstein, S.O. (2008): Further Evidence of the Eects
of Preceding Birth Intervals on Neonatal, Infant, and
Under-Five-Years Mortality and Nutritional Status in
Developing Countries: Evidence from the Demographic
and Health Surveys. DHS Working Paper Series.
Singh, S. et al (2003): Adding It Up: The benets of
investing in sexual and reproductive health care. New
York, NY, USA: The Gumacher Institute and
UNFPA.
Smith, R. et al (2009): Family Planning Saves Lives.
Fourth Edition. Washington, DC, USA: Population
Reference Bureau.
Stenberg, K. et al (2013): Advancing social and
economic development by investing in women’s
and children’s health: a new Global Investment
Framework. Lancet.
United Nations Development Programme (2014).
Nepal Human Development Report 2014: Beyond
Geography, Unlocking Human Potential, Government
of Nepal; National Planning Commission; Singha
Durbar, Kathmandu.
United Nations (2013): World Population Prospects:
The 2012 Revision, Highlights and Advance Tables.
Working Paper No. ESA/P/WP228.
Wilkinson, D., Acharya, S., Devkota, B., Singh-
Rana, P., and Uprety, A. (2011) Evaluation of
UNFPA’s Sixth Country Programme in Nepal (2008-
2012); UNFPA Nepal.
Wolfson, L.J. et al (2008): ‘Estimating the
costs of achieving the WHO-UNICEF Global
Immunization Vision and Strategy, 2006-2015’
Bulletin of the World Health Organization, 86 (1).
World Health Organisation (2010): ‘Constraints to
Scaling Up the Health Millennium Development
Goals: Costing and Financial Gap Analysis.
Background Document for the Taskforce on
Innovative International Financing for Health
Systems.’
World Health Organisation (2011): Choosing
interventions that are cost-eective: country specic
unit costs. Available from: hp://www.who.int/
choice/country/country_specic/en/ [16 April
2014].

35
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Annex
ANNEX A
ESTIMATED TOTAL RESOURCES REQUIRED AND DISAGGREGATED BY AREA
Table 7: Estimated Total Resources (millions)
2015 2016 2017 2018 2019 2020
Total
NPR
Total
USD
Direct intervention costs 1,229.6 1,258.9 1,289.3 1,336.1 1,365.8 1,363.6 7,843.3 87.9
Programme costs 1,099.3 1,094.5 860.6 780.4 456.2 506.8 4,797.7 53.8
Indirect costs 172.7 178.6 184.4 190.3 196.3 201.9 1,124.1 12.6
Total 2,501.6 2,531.9 2,334.3 2,306.8 2,018.4 2,072.2 13,765.2 154.2
Source: OneHealth modelling and OPM calculations
Table 8: Estimated Costs for Strategic Areas and Programme Management (millions)
PROGRAMME COSTS 2015 2016 2017 2018 2019 2020
Total
NPR
Total
USD
1. Demand Generation 258.4 90.6 108.1 196.8 56.9 27.7 738.4 8.27
2. Enhancing Service Delivery 303.1 424.7 292.9 272.1 272.1 272.1 1,836.9 20.59
3. Capacity Building 188.6 207.8 183.6 71.8 71.3 70.8 793.8 8.89
4. Research & Innovation 150.8 103.5 91.5 98.5 2.0 0.0 446.3 5.00
5. Enabling Environment 147.9 217.4 134.0 90.7 3.4 85.8 679.2 7.61
6. General Programme Manage-
ment
50.5 50.5 50.5 50.5 50.5 50.5 303.1 3.40
Total 1,099.3 1,094.5 860.6 780.4 456.2 506.8 4,797.7 53.76
Source: TWG estimates and OPM calculations
Table 9: Estimated drug and supply costs under the scale-up FP scenario (millions)
The table below shows the estimated expenditure on drugs and supplies required for the FP scale-up sce-
nario. This is in constant NPR, so does not include ination.
Source: OneHealth
modelling
2015 2016 2017 2018 2019 2020 Total
NPR
Total
USD
Pill 153.3 157.9 162.5 166.9 171.5 176.0 988.1 11.1
Condom 80.3 83.2 85.9 88.7 91.6 94.4 524.1 5.9
Injectable 224.3 231.6 238.8 245.9 253.2 260.4 1,454.3 16.3
IUD 70.7 74.9 79.2 84.1 88.7 92.2 489.8 5.5
Implant 137.1 148.0 159.2 171.6 183.5 194.1 993.5 11.1
Female sterilization 217.4 211.0 205.3 208.9 201.7 177.1 1,221.3 13.7
Male sterilization 156.0 156.7 157.6 163.0 163.4 155.0 951.7 10.7
Total 1,039.0 1,063.3 1,088.6 1,129.0 1,153.7 1,149.1 6,622.8 74.2
Source: OneHealth modelling

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
36
Table 10: Estimated number of FTE medical personnel required under FP scale-up scenario
2015 2016 2017 2018 2019 2020
Community Health Workers 111 115 119 122 126 129
Auxillary Nurse Midwives 451 466 481 497 513 528
Sta Nurses 53 56 59 61 64 67
Medical Ocers 57 56 56 57 56 51
Obstetricians/Gynaecologists 26 26 25 26 26 23
Total 698 719 740 763 784 798
Source: OneHealth modelling
Table 10 shows the estimated number of full-time equivalent [FTE] medical personnel required for the FP
scale-up scenario. It must be remembered that the FTE numbers below assume that medical personal work
full time on family planning. This is rarely the case. A more realistic assumption would be that sta task
share and only spend some of their time on family planning. For example, if we assume that only 10% of
time is spent on family planning, then these numbers would need to be multiplied by 10 to give the number
of medical personnel who deliver FP interventions as part (10%) of their jobs.
Table 11: Estimated medical personnel costs under FP scale-up scenario (millions)
2015 2016 2017 2018 2019 2020
Total
NPR
Total
USD
Community Health Workers 17.2 17.7 18.3 18.8 19.4 19.9 111.3 1.2
Auxillary Nurse Midwives 120.3 124.4 128.5 132.6 136.8 140.9 783.7 8.8
Sta Nurses 16.9 17.8 18.6 19.5 20.4 21.2 114.3 1.3
Medical Ocers 23.5 23.1 22.9 23.5 23.1 21.1 137.1 1.5
Obstetricians/Gynaecologists 12.7 12.5 12.4 12.7 12.5 11.4 74.2 0.8
Total 190.6 195.6 200.7 207.1 212.2 214.5 1,220.6 13.7
Source: OneHealth modelling
Table 11 shows the estimated expenditure on medical personnel required for the FP scale-up scenario.
Again, this is constant NPR, so does not include ination.
ESTIMATED INDIRECT COSTS
Table 12 shows the estimated indirect costs associated with outpatient visits at dierent levels of health
service provision. The cost of the user in traveling is not included in the estimation; however, it can be ad-
ditional costs for service delivery.
Table 12: Estimated indirect costs under FP scale-up scenario (millions)
2015 2016 2017 2018 2019 2020
Total
NPR
Total
USD
Community 14.1 14.6 15.0 15.5 16.0 16.4 91.6 1.0
Outreach 46.8 48.2 49.6 51.1 52.5 53.8 302.0 3.4
Clinic 66.3 68.6 70.8 73.1 75.4 77.6 431.8 4.8
Hospital 45.5 47.2 48.9 50.7 52.5 54.1 298.8 3.3
Total 172.7 178.6 184.4 190.3 196.3 201.9 1,124.1 12.6
Source: OneHealth modelling

37
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
ANNEX B
Estimated resource requirements of General Programme Management, by key interventions, related programmatic activities and year, (natural units)
GENERAL PROGRAMME MAN-
AGEMENT
2015 2016 2017 2018 2019 2020 Total NPR Total USD
MOHP, District/Regional Level 48,379,695 48,379,695 48,379,695 48,379,695 48,379,695 48,379,695 290,278,170 3,252,781
FP Supervisor 24,107,200 24,107,200 24,107,200 24,107,200 24,107,200 24,107,200 144,643,200 1,620,834
Regional FP Ocer 1,651,000 1,651,000 1,651,000 1,651,000 1,651,000 1,651,000 9,906,000 111,004
Public Health Nurse 4,896,775 4,896,775 4,896,775 4,896,775 4,896,775 4,896,775 29,380,650 329,232
District Health Ocer 2,870,400 2,870,400 2,870,400 2,870,400 2,870,400 2,870,400 17,222,400 192,990
Facility Manager 12,053,600 12,053,600 12,053,600 12,053,600 12,053,600 12,053,600 72,321,600 810,417
Regional Safe Motherhood Ocer 390,000 390,000 390,000 390,000 390,000 390,000 2,340,000 26,221
HMIS Ocer 2,410,720 2,410,720 2,410,720 2,410,720 2,410,720 2,410,720 14,464,320 162,083
MOHP, Central Level (FHD) 2,134,470 2,134,470 2,134,470 2,134,470 2,134,470 2,134,470 12,806,820
143,510
Director 125,190 125,190 125,190 125,190 125,190 125,190 751,140
8,417
FP Focal Point 382,720 382,720 382,720 382,720 382,720 382,720 2,296,320
25,732
FP Support Sta 1,148,160 1,148,160 1,148,160 1,148,160 1,148,160 1,148,160 6,888,960
77,196
FCHV Focal Point 191,360 191,360 191,360 191,360 191,360 191,360 1,148,160
12,866
Demographer/Statisticians 229,632 229,632 229,632 229,632 229,632 229,632 1,377,792
15,439
Safe Motherhood Focal Point 57,408 57,408 57,408 57,408 57,408 57,408 344,448
3,860
Total 50,514,165 50,514,165 50,514,165 50,514,165 50,514,165 50,514,165 303,084,990 3,396,291
Source: TWG estimates and OPM calculations
Note: Includes programme sta for whom FP activities constitute a signicant share of their current daily work at FTE. Personnel from NHEICC, NHTC, LMD, MD, Finance & Admin play cross-cuing
roles & are not costed

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
38
ANNEX C
Estimated resource requirements of Enabling Environment, by key interventions, related programmatic activities and year, (natural units)
ENABLING ENVIRONMENT 2015 2016 2017 2018 2019 2020 Total NPR Total USD
1. Increase Advocacy for Family Planning 139,172,500 217,385,500 133,952,500 90,713,000 2,325,000 85,758,000 669,306,500 7,500,073
1.1 Identify national level champions of FP from
multiple elds and facilitate their advocacy
role
450,000 450,000 450,000 450,000 450,000 450,000 2,700,000 30,255
1.2 Develop and distribute advocacy package (in
English and Nepali) for key stakeholders
3,420,000 0 0 3,420,000 0 0 6,840,000 76,647
1.3 Organize advocacy events at central level 1,800,000 0 0 1,535,000 0 0 3,335,000 37,371
1.4 Organize advocacy events at district level 5,612,500 5,612,500 5,612,500 1,875,000 1,875,000 1,875,000 22,462,500 251,709
1.5 Organize advocacy events at community level 127,890,000 127,890,000 127,890,000 0 0 0 383,670,000 4,299,305
1.6 Celebrate FP day at community level 0 83,433,000 0 83,433,000 0 83,433,000 250,299,000 2,804,785
2. Address legal and socio-cultural barriers to ac-
cess to FP for young people and other groups
including people with disability
2,620,500 0 0 0 1,100,000 0 3,720,500 41,691
2.1 Update the National ASRH strategy 1100000 0 0 0 1100000 0 2200000 24652.62214
2.2 Advocate with MOE, CDB & others to in-
corporate CSE components in curriculum for
Grade 9-10
220500 0 0 0 0 0 220500 2470.865083
2.3 Develop a national strategy on meeting RH/
FP needs of disabled group and support
implementation through multi-sectoral co-
ordination
1300000 1300000 14567.45854
3. Strengthen integration of services 4,650,000 0 0 0 0 0 4,650,000 52,107
3.1 Develop national FP service integration strat-
egy
2,950,000 0 0 0 0 0 2,950,000 33,057
3.2 Based on strategy, develop operational guide-
lines
1,700,000 0 0 0 0 0 1,700,000 19,050
4. Promote task shiing 1,500,000 0 0 0 0 0 1,500,000 16,809
4.1 Develop a national strategy on task shiing 1,500,000 0 0 0 0 0 1,500,000 16,809
Total 147,943,000 217,385,500 133,952,500 90,713,000 3,425,000 85,758,000 679,177,000 7,610,679
Source: TWG estimates and OPM calculations

39
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
ANNEX D
Estimated resource requirements of Demand Generation, by key interventions, related programmatic activities and year, (in natural units)
DEMAND GENERATION 2015 2016 2017 2018 2019 2020 Total NPR Total USD
1. Support to enhance Comprehensive Sexual
-
ity Education for in-school and out-of-school
young people.
9,076,500 3,836,000 21,350,000 750,000 750,000 750,000 36,512,500 409,149
1.1 Support implementation of CSE in Grades 6-10 8,226,500 3,086,000 20,600,000 0 0 0 31,912,500 357,603
1.2 Conduct interactive sessions with students on
CSE, Grade 11-12
850,000 750,000 750,000 750,000 750,000 750,000 4,600,000 51,546
2. Increase knowledge of FP amongst individuals/
couples to facilitate decision-making on con
-
traceptive use through designing, implemen-
tation and evaluation of high quality SBCC
interventions
38,375,000 0 0 38,375,000 0 0 76,750,000 860,040
2.1 Develop and disseminate FP information
through dierent media (in 2015 & 2018)
38,375,000 0 0 38,375,000 0 0 76,750,000 860,040
3. Reach adolescents with FP messages through
innovative approaches (m-health & e-health)
15,250,000 8,750,000 8,750,000 13,750,000 8,750,000 8,750,000 64,000,000 717,167
3.1 Utilize SMS technology to promote FP use
amongst adolescents/youth
2,000,000 1,000,000 1,000,000 1,000,000 1,000,000 1,000,000 7,000,000 78,440
3.2 Introduce FP messages through mobile health
apps
4,500,000 0 0 4,500,000 0 0 9,000,000 100,852
3.3 Implement hotline telephone program for
adolescents
7,500,000 7,500,000 7,500,000 7,500,000 7,500,000 7,500,000 45,000,000 504,258
3.4 Pilot & implement e-health FP program for
adolescents in urban areas
1,250,000 250,000 250,000 750,000 250,000 250,000 3,000,000 33,617
4. Reduce socio-cultural barriers to accessing FP
services
90,500,000 15,000,000 15,000,000 90,500,000 15,000,000 15,000,000 241,000,000 2,700,583
4.1 Implement community interaction programs
with FCHVs/health workers providing detailed
info
90,500,000 15,000,000 15,000,000 90,500,000 15,000,000 15,000,000 241,000,000 2,700,583
5. Address fear of side-eects (perceived and
real), myths & misconceptions
9,700,000 3,000,000 3,000,000 3,000,000 3,000,000 0 21,700,000 243,165

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
40
DEMAND GENERATION 2015 2016 2017 2018 2019 2020 Total NPR Total USD
5.1 Develop IEC materials, including value of
daughters
6,500,000 0 0 0 0 0 6,500,000 72,837
5.2 Orient HW, FCHVs, community leaders in vari
-
ous forums [no add. cost, merged with other
activities]
0 0 0 0 0 0 0 0
5.3 Organize satised client interaction program at
community level
3,200,000 3,000,000 3,000,000 3,000,000 3,000,000 0 15,200,000 170,327
6. Develop and implement micro-plan for specic
groups
25,202,500 21,000,000 21,000,000 21,000,000 0 0 88,202,500 988,374
6.1 Review existing evidence on barriers to FP utili
-
zation for specic groups
4,202,500 0 0 0 0 0 4,202,500 47,092
6.2 Develop and implement district-specic action
plan (for districts with lowest CPR)
21,000,000 21,000,000 21,000,000 21,000,000 0 0 84,000,000 941,282
7. Design, implement & evaluate special program
for improved FP access & utilization of adoles
-
cents/youth
31225000 29000000 29000000 29000000 29000000 2750000 149975000 1680580.46
7.1 Develop age-specic peer education program
(both in-school and out-of-school youth)
29,225,000 27,000,000 27,000,000 27,000,000 27,000,000 750,000 137,975,000 1,546,112
7.2 Implement targeted activities to delay rst
pregnancy for newly married young couples
2,000,000 2,000,000 2,000,000 2,000,000 2,000,000 2,000,000 12,000,000 134,469
7.3 Integrate FP into school health programme (no
additional costs)
0 0 0 0 0 0 0 0
8. Special program for migrants and their spouses
particularly focused on in districts with high
seasonal out-migrations 600000 600000 600000 400000 400000 400000 3000000 33617.212
8.1 Ensure timely and correct dissemination of
information for returnee to prevent unwanted
pregnancy (pre-departure & upon arrival)
600,000 600,000 600,000 400,000 400,000 400,000 3,000,000 33,617
9. Special program for postpartum women 26,785,000 0 0 0 0 0 26,785,000 300,146
9.1 Group counseling for couples during vaccina
-
tion days/EPI clinics on PP FP (esp. on myths)
2,175,000 0 0 0 0 0 2,175,000 24,372
9.2 Promote counseling among pregnant & post
-
partum women in HMGs
24,610,000 0 0 0 0 0 24,610,000 275,773
10. Special program for post-abortion women 650,000 0 0 0 0 0 650,000 7,284

41
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
DEMAND GENERATION 2015 2016 2017 2018 2019 2020 Total NPR Total USD
10.1 Incorporate FP info in the existing info pack
-
ages on CAC services
650,000 0 0 0 0 0 650,000 7,284
11. Special program for individuals and couples
in hard-to-reach communities
10,755,000 9,405,000 9,405,000 0 0 0 29,565,000 331,298
11.1 Identify communities/areas with low FP utili
-
zation (including l among MDAG population)
750,000 0 0 0 0 0 750,000 8,404
11.2 Implement community interaction program to
identify clients for counseling (explore success
stories)
8,430,000 7,830,000 7,830,000 0 0 0 24,090,000 269,946
11.3 Utilize community mobilisers (25 districts
each year for 3 years)
1,375,000 1,375,000 1,375,000 0 0 0 4,125,000 46,224
11.4 Increase FP use amongst urban slum dwellers
(in 20 municipalities)
200,000 200,000 200,000 0 0 0 600,000 6,723
Total 258,119,000 90,591,000 108,105,000 196,775,000 56,900,000 27,650,000 738,140,000 8,271,403
Source: TWG estimates and OPM calculations

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
42
ANNEX E
Estimated resource requirements of Enhancing Service Delivery, by key interventions, related programmatic activities and year, (natural units)
ENHANCING SERVICE DELIVERY 2015 2016 2017 2018 2019 2020 Total NPR Total USD
1. Improving services at Community Level 37,370,000 156,230,500 24,380,000 4,805,000 4,805,000 4,805,000 232,395,500 2,604,163
1.1 Update FP orientation package for capacity
building of FCHVs (including on PPFP)
12,990,000 0 0 0 0 0 12,990,000 145,563
1.2 Conduct refresher orientation for FHCVs, based
on revised package
0 131,850,500 0 0 0 0 131,850,500 1,477,482
1.3 Establish condom boxes at appropriate places in
community (shops, etc.)
20,880,000 20,880,000 20,880,000 1,305,000 1,305,000 1,305,000 66,555,000 745,798
1.4 Train FCHVs on urine pregnancy test kit, FP
counseling, ANC, safe abortion services
-
1.5 Organize visits to countries with strong com
-
munity-based FP programs (e.g. Bangladesh,
Indonesia)
3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 21,000,000 235,320
2. Improving services through PHC/ORC clinics
and other out-reach approaches
168,065,250 164,900,000 164,900,000 164,900,000 164,900,000 164,900,000 992,565,250 11,127,382
2.1 Rapid assessment of the situation of the PHC/
ORC Clinics across the country
1,800,000 0 0 0 0 0 1,800,000 20,170
2.2 Develop 1-2 model PHC/ORCs per VDC (low
CPR districts), later to be static SDP
600,000 0 0 0 0 0 600,000 6,723
2.3 Utilize urban health clinics at each tole for FP
services (20 municipalities)
1,265,250 500,000 500,000 500,000 500,000 500,000 3,765,250 42,192
2.4 Conduct comprehensive FP camps (focused on
LAPM) in all 75 districts
150,000,000 150,000,000 150,000,000 150,000,000 150,000,000 150,000,000 900,000,000 10,089,686
2.5 Conduct satellite clinics to improve the access to
LARM among women residing in remote, rural
areas.
14,400,000 14,400,000 14,400,000 14,400,000 14,400,000 14,400,000 86,400,000 968,610
3. Improving services at HP/PHCs, including
birthing centers
12,950,000 22,950,000 22,950,000 22,950,000 22,950,000 22,950,000 127,700,000 1,430,973
3.1 Expand availability of all temporary FP methods 7,500,000 7,500,000 7,500,000 7,500,000 7,500,000 7,500,000 45,000,000 504,258
3.2 Reinforce availability of FP services 0 0
3.3 Expand PPIUCD in birthing centers: launch pilot
program
5,000,000 15,000,000 15,000,000 15,000,000 15,000,000 15,000,000 80,000,000 896,459
3.4 Expand NSV to PHCC, promoting task-shiing
(PHCs selected on lower CPR districts)
450,000 450,000 450,000 450,000 450,000 450,000 2,700,000 30,255

43
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
ENHANCING SERVICE DELIVERY 2015 2016 2017 2018 2019 2020 Total NPR Total USD
3.5 FP at all levels of HF (reporting and quality as
-
surance in public, NGO and private sector, and
inventory & stock management in HF). Use vac
-
cinator in their free days for FP services
3.6 Add responsibilities to ANM/SN including for
facilitation of community level meetings.
3.7 Focus on quality FP counseling during 3rd & 4th
ANC, include this in the ANC card
0 0 0 0 0 0 0 0
4. Improving services in District Hospitals 20,500,000 18,400,000 18,400,000 18,400,000 18,400,000 18,400,000 112,500,000 1,260,645
4.1 Expand availability of all temporary FP methods
& 1 VSC method
500,000 0 0 0 0 0 500,000 5,603
4.2 Develop 24 IFPSC as comprehensive RH clinics 1,300,000 0 0 0 0 0 1,300,000 14,567
4.3 Develop district-level FP micro-planning & com
-
modity forecasting
18,700,000 18,400,000 18,400,000 18,400,000 18,400,000 18,400,000 110,700,000 1,240,475
5. Improving services in Zonal and Regional Hos
-
pitals
0 0 0 0 0 0 0 0
5.1 Establish FP services in multi-disciplinary hos
-
pitals
0 0 0 0 0 0 0 0
5.2 Establish re-canalization services 0 0 0 0 0 0 0 0
6. Social marketing 5,000,000 5,000,000 5,000,000 5,000,000 5,000,000 5,000,000 30,000,000 336,172
6.1 Revive private provider's network (implemented
through PPP model)
5,000,000 5,000,000 5,000,000 5,000,000 5,000,000 5,000,000 30,000,000 336,172
6.2 PPP for strengthening supply chain commodity
management.
0 0 0 0 0 0 0 0
7. Support NGOs providing FP services 260,000 160,000 160,000 160,000 160,000 160,000 1,060,000 11,878
7.1 Revive NGOCC for organizations working in FP 250,000 150,000 150,000 150,000 150,000 150,000 1,000,000 11,206
7.2 Facilitate NGOs to provide FP services 10,000 10,000 10,000 10,000 10,000 10,000 60,000 672
8. Support Medical College Teaching Hospitals 800,000 0 0 0 0 0 800,000 8,965
8.1 Establish FP service centers in each medical col
-
lege
500,000 0 0 0 0 0 500,000 5,603
8.2 Include LAFP training in doctor and nurse pre-
service curriculum
300,000 0 0 0 0 0 300,000 3,362
9. Strengthen coordination of private sector 25,000 25,000 25,000 25,000 25,000 25,000 150,000 1,681

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
44
ENHANCING SERVICE DELIVERY 2015 2016 2017 2018 2019 2020 Total NPR Total USD
9.1 Strengthen coordination mechanism and report
-
ing, to ensure functionality
25,000 25,000 25,000 25,000 25,000 25,000 150,000 1,681
10. Improved integration of FP services with EPI,
HIV, and Postpartum, Post-abortion, RH-mor
-
bidities, urban health and other programs.
10,000,000 10,000,000 10,000,000 10,000,000 10,000,000 10,000,000 60,000,000 672,344
10.1 Pilot new integration approaches (10 approach
-
es)
10,000,000 0 0 0 0 0 10,000,000 112,057
10.2 Scale-up proven models in next 5 years 0 10,000,000 10,000,000 10,000,000 10,000,000 10,000,000 50,000,000 560,287
11. Improve facility recording and reporting 100,000 100,000 100,000 100,000 100,000 100,000 600,000 6,723
11.1 Strengthen and update recording/reporting
system, coordination with HMIS
100,000 100,000 100,000 100,000 100,000 100,000 600,000 6,723
11.2 Develop M&E tools for private providers in
line with HMIS tools
[in 11.1] [in 11.1]
12. Establish Quality of Care unit 3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 21,000,000 235,320
12.1 Establish quality of care unit 3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 21,000,000 235,320
13. Strengthen management capacity of FP Ocers 5,700,000 4,700,000 4,700,000 3,500,000 3,500,000 3,500,000 25,600,000 286,867
13.1 Development of training curriculum 1,000,000 0 0 0 0 0 1,000,000 11,206
13.2 Conducting training of FP ocers 1,200,000 1,200,000 1,200,000 0 0 0 3,600,000 40,341
13.3 Conduct observation study tour 3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 3,500,000 21,000,000 235,320
14. Help ensure contraceptive security 25,000 25,000 25,000 25,000 25,000 25,000 150,000 1,681
14.1 Coordination with LMD to ensure regular sup
-
ply
25,000 25,000 25,000 25,000 25,000 25,000 150,000 1,681
15. Enhance coordination at the central and district
levels
38,730,000 38,730,000 38,730,000 38,730,000 38,730,000 38,730,000 232,380,000 2,603,989
15.1 Improved coordination at central level 105,000 105,000 105,000 105,000 105,000 105,000 630,000 7,060
15.2 Improved coordination at district level 38,625,000 38,625,000 38,625,000 38,625,000 38,625,000 38,625,000 231,750,000 2,596,930
Total 303,025,250 424,720,500 292,870,000 272,095,000 272,095,000 272,095,000 1,836,900,750 20,588,784
Source: TWG estimates and OPM calculations

45
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
ANNEX F
Estimated resource requirements of Capacity Building, by key interventions, related programmatic activities and year, (natural units)
CAPACITY-BUILDING 2015 2016 2017 2018 2019 2020 Total NPR Total USD
1. Core FP training to service provid
-
ers (training/DSA cost)
42,720,591 59,913,719 59,913,719 21,352,704 21,352,704 21,352,704 226,606,141 2,539,289
1.1 IUCD 5,737,324 6,895,316 6,895,316 3,473,976 3,473,976 3,473,976 29,949,884 335,611
1.2 Implant 8,371,756 10,056,637 10,056,637 5,001,992 5,001,992 5,001,992 43,491,008 487,349
1.3 CoFP/C 14,492,100 19,322,800 19,322,800 6,473,138 6,473,138 6,473,138 72,557,114 813,056
1.4 NSV 3,226,260 3,858,860 3,858,860 1,897,800 1,897,800 1,897,800 16,637,380 186,434
1.5 Minilap 2,226,610 2,657,567 2,657,567 1,364,696 1,364,696 1,364,696 11,635,832 130,388
1.6 PPIUCD 263,180 315,816 315,816 157,908 157,908 157,908 1,368,536 15,335
1.7 Sangini/Depo 8,403,361 16,806,723 16,806,723 2,983,193 2,983,193 2,983,193 50,966,387 571,116
2. Core FP training to service provid
-
ers (travel costs)
76,771,247 111,588,629 111,588,629 38,277,495 38,277,495 38,277,495 414,780,990 4,647,927
2.1 Travel cost (except Sangini) 63,152,321 91,793,233 91,793,233 31,487,214 31,487,214 31,487,214 341,200,427 3,823,402
2.2 Travel cost (Sangini) 13,618,926 19,795,396 19,795,396 6,790,281 6,790,281 6,790,281 73,580,563 824,524
3. Core FP training to service provid
-
ers (printing of training material)
20,366,124 10,031,076 0 0 0 0 30,397,200 340,623
1.1 IUCD 1,756,740 865,260 0 0 0 0 2,622,000 29,381
1.2 Implant 2,557,524 1,259,676 0 0 0 0 3,817,200 42,775
1.3 CoFP/C 8,681,190 4,275,810 0 0 0 0 12,957,000 145,193
1.4 NSV 544,040 267,960 0 0 0 0 812,000 9,099
1.5 Minilap 662,630 326,370 0 0 0 0 989,000 11,082
1.6 PPIUCD 134,000 66,000 0 0 0 0 200,000 2,241
1.7 Sangini/Depo 6,030,000 2,970,000 0 0 0 0 9,000,000 100,852
4. FP training material development 1,600,000 800,000 0 0 0 0 2,400,000 26,894
4.1 Training material revision 1,600,000 800,000 0 0 0 0 2,400,000 26,894
5. Development and use of alterna
-
tive training approaches
8,250,000 8,250,000 0 0 0 0 16,500,000 184,895
5.1 Material and implementation of
modied computer/web-based
learning
8,250,000 8,250,000 0 0 0 0 16,500,000 184,895
6. Task-shiing on NSV 500,000 1,000,000 1,000,000 1,000,000 500,000 0 4,000,000 44,823

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
46
CAPACITY-BUILDING 2015 2016 2017 2018 2019 2020 Total NPR Total USD
6.1 Train Health Assistants to provide
NSV
500,000 1,000,000 1,000,000 1,000,000 500,000 0 4,000,000 44,823
7. Strengthen national FP training
capacity
17,740,000 740,000 740,000 740,000 740,000 740,000 21,440,000 240,251
7.1 Renovation/upgrading of existing
FP clinical training sites
11,000,000 0 0 0 0 0 11,000,000 123,263
7.2 Maintenance of sites 440,000 440,000 440,000 440,000 440,000 440,000 2,640,000 29,583
7.3 Establishment of new sites 6,000,000 0 0 0 0 0 6,000,000 67,234
7.4 Renovation/upgrading of existing
RHTC
300,000 300,000 300,000 300,000 300,000 300,000 1,800,000 20,170
8. Development of pool of FP trainers 10,291,200 5,068,800 0 0 0 0 15,360,000 172,120
8.1 CTS training 1,206,000 594,000 0 0 0 0 1,800,000 20,170
8.2 Preparation of clinical mentors in
FP
1,206,000 594,000 0 0 0 0 1,800,000 20,170
8.3 Physician trainers 4,596,200 2,263,800 0 0 0 0 6,860,000 76,871
8.4 Nurse trainers 3,283,000 1,617,000 0 0 0 0 4,900,000 54,908
9. Recanalization training 390,000 390,000 390,000 390,000 390,000 390,000 2,340,000 26,221
9.1 Recanalization training (including
microsurgery skills)
390,000 390,000 390,000 390,000 390,000 390,000 2,340,000 26,221
10.Continue capacity building of
health workers even aer comple
-
tion of formal training
10,000,000 10,000,000 10,000,000 10,000,000 10,000,000 10,000,000 60,000,000 672,344
10.1 Strengthen Post training follow
up through on-site coaching and
o-site supportive supervision
10,000,000 10,000,000 10,000,000 10,000,000 10,000,000 10,000,000 60,000,000 672,344
Total 188,629,162 207,782,224 183,632,348 71,760,199 71,260,199 70,760,199 793,824,331 8,895,387
Source: TWG estimates and OPM calculations

47
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
ANNEX G
Estimated resource requirements of Research & Innovation, by key interventions, related programmatic activities and year, (natural units)
RESEARCH AND INNOVATION 2015 2016 2017 2018 2019 2020 Total NPR Total USD
1. Generate evidence through operational research, to
promote innovations in FP
150,840,000 103,500,000 91,500,000 98,500,000 2,000,000 0 446,340,000 5,001,569
1.1 Understand the factors that lead to discontinuation
of contraceptives including LARC
4,000,000 0 0 0 0 0 4,000,000 44,823
1.2 Document unintended pregnancy among FSWs (in
-
cidence, causes, consequences, complications)
0 2,000,000 0 0 0 0 2,000,000 22,411
1.3 Analysis of barriers for FP uptake among specic
communities, including youth & hard to reach
0 2,000,000 0 0 0 0 2,000,000 22,411
1.4 Evaluate m-health approach (being implemented)
for reaching adolescents with FP information
2,500,000 0 0 0 0 0 2,500,000 28,014
1.5 Feasibility study on use of social media and health-
apps for FP messages, especially for youth
2,500,000 2,500,000 0 0 5,000,000 56,029
1.6 Evaluate the existing program on Postpartum FP
and PP-IUCD.
1,500,000 1,500,000 0 0 3,000,000 33,617
1.7 Research on implementing PP FP/IUCD based on
the best practices identied from evaluation
7,500,000 0 0 0 0 0 7,500,000 84,043
1.8 Periodic review/evaluation of FP program (specic
for advocacy and demand generation activities)
5,000,000 0 0 5,000,000 0 0 10,000,000 112,057
1.9 Assessment of barriers in delivering CSE among
school teachers
3,500,000 0 0 0 0 0 3,500,000 39,220
1.10 FP care-seeking behavior among urban slum dwell
-
ers
2,000,000 0 0 0 0 0 2,000,000 22,411
1.11 Using operational research ndings to expand
contraceptive choices
0 2,000,000 0 0 2,000,000 4,000,000 44,823
1.12 Using operational research to follow up PP women
and defaulters
3,000,000 0 0 0 0 0 3,000,000 33,617
1.13 Conduct operational research on implementing
task shiing in FP (minimum 1 year of complete
implementation followed by evaluation of the
outcome)
7,000,000 3,000,000 10,000,000 112,057
1.14 Performance evaluation of SBAs on provision of
IUCD services
5,000,000 5,000,000 56,029

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
48
RESEARCH AND INNOVATION 2015 2016 2017 2018 2019 2020 Total NPR Total USD
1.15 Performance evaluation of medical ocer on provi
-
sion of NSV services
5,000,000 5,000,000 56,029
1.16 Further analysis of NDHS 2016 on relevant issue 2,000,000 2,000,000 22,411
1.17 Improving women and men's understanding of
the risk of pregnancy at dierent time during the
life course and during the menstrual cycle (fertility
awareness)
89,500,000 89,500,000 89,500,000 89,500,000 0 0 358,000,000 4,000,000
1.18 Market segmentation study to describe the current
market and service providers for FP in Nepal
17,840,000 17,840,000 200,000
Total 150,840,000 103,500,000 91,500,000 98,500,000 2,000,000 0 446,340,000 4,990,004
Source: TWG estimates and OPM calculations

49
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
ANNEX H
SCENARIO MODELLED
Assumptions (50%
MCPR by 2021)
2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2021
CPR, all methods 49.7 49.8 49.9 50.0 51.1 52.1 53.2 54.3 55.4 56.4 57.5
CPR, modern meth-
ods
43.2 43.3 43.4 43.5 44.4 45.3 46.2 47.2 48.1 49.0 50.0
TFR 2.6 2.6 2.6 2.5 2.5 2.4 2.3 2.3 2.2 2.1 2.1
Unmet need 27.0 26.9 26.9 26.8 26.2 25.5 24.8 24.2 23.5 22.7 22.0
Demand satised by
modern methods
56.3 56.4 56.5 56.6 57.4 58.4 59.3 60.1 61.0 62.0 62.9
FP Method Mix 2016 2017 2018 2019 2020 2021
Condom 10.2 10.3 10.3 10.4 10.4 10.5
Female sterilization 30.9 29.9 28.9 27.9 27 26
Injectable 21.5 21.6 21.7 21.8 21.9 22
IUD 4.5 4.8 5.1 5.4 5.7 6
Male sterilization 18 18 18 18 18 18
Implant 5.3 5.8 6.3 6.8 7.3 7.8
Pills 9.7 9.7 9.7 9.7 9.7 9.7
Total 100 100 100 100 100 100

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
50
Members of the Target Seing Group
1. Mr. Paban Ghimire (FHD)
2. Mr. Mukti Khanal (HMIS Section)
3. Dr. Sharad Sharma (MoCTCA)
4. Mr. Bharat Ban (SCF/SNL) – Group Co-coordinator
5. Mr Ashoke Shrestha (Freelancer)
6. Dr Prakash Dev Pant (FHI 360/GGMS)
7. Mr Ajit Pradhan (Freelancer)
8. Mr. Tirtha Tamang (UNFPA)
9. Mr Sujan Karki (UNICEF)
10. Mr Pradeep Poudel (NHSSP)
Members of the Technical Working Group
1. Dr Pushpa Chaudhary (Director, FHD)
2. Dr Kiran Regmi (Ex-Director, FHD)
3. Mr Ghanshyam Pokharel (FP Section Chief, FHD)
4. Mr Bhogendra Raj Dotel (Ex-FP Section Chief, FHD)
5. Dr Laxmi Raj Pathak (Consultant)
6. Mr Dirgha Raj Shrestha (IPAS)
7. Dr Rajendra Bhadra (H4L)
8. Mr Sitaram Devkota (PSI)
9. Mr Netra Bhaa (USAID)
10. Dr Deepak Paudel (DFID)
11. Dr Shilu Adhikari (UNFPA)

51
NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
Amit Aryal , NHSSP Hari Sharan Karki, NHEICC (Dr.) Rajendra Gurung, NHSSP
Anita Subba, DHO/Morang (Dr.) Ishwor Upadhyaya , MWICTC (Dr.) Ram Adhar P. Mahato, NHTC
Ananta Pd. Sharma, DHO/Kavre Jagadishwor Ghimire, PSI Nepal Ram Bhandari, NEPHA
Arjun Aryal , FPAN (Dr.) Janardan Lamichhane, Lifeline Ramesh Adhikary, DPHO/Kaski
Badri Bahadur Khadka, NHEICC (Dr.) Jasmine Shrestha, CFWC (Dr.) Ramesh Kharel, PHCRD
Badri Gyawali, FHD (Dr.) Jeewan Bhaarai, Freelancer (Dr.) Rishi Kesh Kae, CRS
(Dr.) Bal Krishna Subedi, PHCRD Jhalak Sharma Poudel, DHO/Palpa Rishi Kesh Sharma , Lifeline Nepal
Basant Thapa, SSP/ FHI 360 Justine Coulson , SPN/MSI Ron Hess, HC3
Bhagawan Shrestha, SSP Kamal Tara Bajracharya Ruchita Rayamajhi, SPN/MSI
Bharat Ban, SAVE Kanak Raj Shrestha, FHD Sabitri Sapkota, SPN/MSI Nepal
Bidya Shrestha, PSI Nepal (Dr.) Khageshwor Gelal, NHTC Sabita Tuladhar, H4L
Bikalpa Upadhyaya , Lifeline Nepal Khemraj Shrestha, H4L Sagar Dahal, MoHP
Binda Ghimire, NAN Krishna Bahadur Rayamajhi, CRS (Dr.) Sameena Rajbhandari, Suaahara
Bishal Gole, UNFPA Kristine Blokhus, UNFPA Sarah Keen, OPM
Bishnu Banskota, FHD Latika Maskey Pradhan, UNFPA Sarita Dhakal, PMWH
Bobby Rawal Basnet, UNFPA Laxman Nepali, CRS Satish Raj Pandey, FHI 360
Catherine Breen Kamkong, UNFPA Laxmi Gaudel, LMD (Dr.) Senendra Raj Uprety, DoHS
Chandeshwari Tamrakar, ADRA Machhindra Neupane, DHO/Dhading Shakun Sharma, ADRA Nepal
Chandra Bahadur B.C., FHD Madan Raj Bha, FHI 360 (Dr.) Shanti Joshi, CFWC
Chandra Mani Dhungana, UNFPA Mahendra Prasad Shrestha, NHTC (Dr.) Shilu Aryal , FHD
Chandra Rai, Jhpiego (Dr.) Manav Bhaarai, World Bank Shiva Hari Bhaa, Naubise HP
Chris James, OPM Mangala Manandhar, FHD Srana Nepal, UNFPA
Chuda Mani Bhaarai, NHTC Manjila Sharma, SPN/MSI Sujeena Shakya, ADRA Nepal
Dev Kant Jha, RHTC/Janakpur (Dr.) Megh Raj Banjara, Consultant Sunil Shrestha, NCDA/Bagmati
Dharani Niroula, DHO/Sunsari (Dr.) Meera Upadhyaya , WHO (Dr ) Suresh Mehta, NHSSP
Dilli Raman Adhikari, DHO/Sunsari (Dr.) Maureen Dariang, NHSSP Susheel Lekhak, WHO
Dinesh Chapagain, DPHO/Bhaktapur Naramaya Limbu, USAID Sushma Chitrakar , CRS
Dinesh Pradhan, FPAN (Dr.) Neeta Shrestha, FHI 360 Tanka Bhaarai, NHTC
Gajendra Rai, USAID (Dr.) Om Maharjan, FPAN Tika Ram Bhandari, WRHTC
Geeta Koirala, Koshi Zonal Hospital Pareka Rai, TUTH Tulasa Bharati, GIZ
Giulia Vallese, UNFPA Paritra Tamrakar, PSI Nepal Udev Maharjan, Lifeline Nepal
Gyan Bahadur B.C., LMD Pema Lhaki, NFCC (Dr.) Yam Basnet, WRH
Hare Ram Bhaarai, GGMS/ FHI 360 Phulgendra Singh, UNFPA Yub Raj Poudel, NHSSP
Hari D Maharjan, Maternity Hospital Pranab Rajbhandari, HC3
LIST OF CONTRIBUTORS

52

NatioNal Family PlaNNiNg Costed imPlemeNtatioN PlaN 2015-2020
54
