
176 International Family Planning Perspectives
Although governments develop family planning policies
to guide program design and implementation, these poli-
cies can have both intended and unintended consequences.
As a result, policies may need periodic revision to achieve
the desired outcomes. Over the last two decades, the gov-
ernment of Peru has instituted a series of laws and policies
designed to enhance access to family planning services and
commodities. In practice, these policies have not always
had their desired effect. This paper examines the policies
Peru’s Ministry of Health has developed and implement-
ed to promote access to family planning for all, and how
those policies have affected contraceptive prevalence,
method mix and source mix.
In this article, we review policies and laws relevant to
family planning and provide insight on how the family plan-
ning policies have evolved and affected access to services,
as well as how characteristics of and trends in the family
planning market* have changed over time. Our assessment
draws on multiple information sources, including family
planning market segmentation data and literature on Peru’s
family planning program. Additional sources, such as om-
budsman reports, user and provider interviews and health
facility studies, clarify specific points.
A historic overview of key family planning policies and
programs implemented in Peru, focusing on three time pe-
riods, 1985–1995, 1995–2000 and 2000–2004, provides
information on policies that have been put in place and the
degree to which they have affected access to family plan-
ning among the poor.
Establishing Peru’s Family Planning Program
In 1983, as a result of available donor funds, a favorable
political environment and the government’s concern for
population growth, the Ministry of Health began provid-
ing family planning services. It began with a vertical pro-
gram that was relatively autonomous in program content
and supervision and in use of financial resources and com-
modities.
1
This effort was followed in 1985 by the estab-
lishment of the first National Population Policy, which stat-
ed that individuals and couples should be provided with
information, health services and contraceptive methods,
with the exception of voluntary sterilization, to assist them
in making informed decisions about family size and fertil-
ity.
2
Under the first National Family Planning Program
(1987–1990), developed to implement the National Pop-
ulation Policy and financed by a combination of donor and
government funds, the Ministry of Health coordinated
public- and private-sector family planning programming
and established goals for reductions in fertility and targets
for increases in contraceptive use. Implementation of the
program began in 1988, and despite political support, faced
multiple challenges, including a national economic crisis,
public-sector reorganization and the Ministry of Health’s
limited service delivery capacity; as a result, it was not im-
plemented as broadly or as rapidly as envisioned. Despite
the program’s limitations, it contributed to a substantial
reduction in the country’s total fertility rate—from 4.1 in
1986 to 3.5 in 1991
3
—which was likely due to the increased
availability of contraceptives, especially in rural areas.
4
Peru’s second National Family Planning Program
(1991–1995), which also received considerable political
commitment, continued to focus on expanding service de-
livery in underserved and predominantly rural areas. This
expansion of services was financed by increased funding
from government, which paid 20% of program costs, and
donors, who paid 80%.
4
Annual government spending on
health in general increased from 52 soles (US$16) per capi-
ta during the late 1980s to 59 soles (US$18) per capita dur-
ing the period 1991–1995.
5
Meanwhile, annual donor in-
vestment in population-related activities in Peru increased
from US$5.2 million in 1987 to US$12.9 million in 1994
and, spurred in part by the focus of the International Con-
ference on Population and Development (ICPD) on fami-
ly planning and donor priorities in the late 1990s, to US$28
million in 1998.
6,7
In the early 1990s, in keeping with the worldwide trend
of user fees in the public sector, most Ministry of Health
facilities in urban areas charged clients for family planning
services and products, while free family planning was avail-
able in rural areas, where the majority of the poor reside.
In 1992, 41% of women reported obtaining family plan-
ning products and services from the commercial sector
(pharmacies and private providers), while 36% obtained
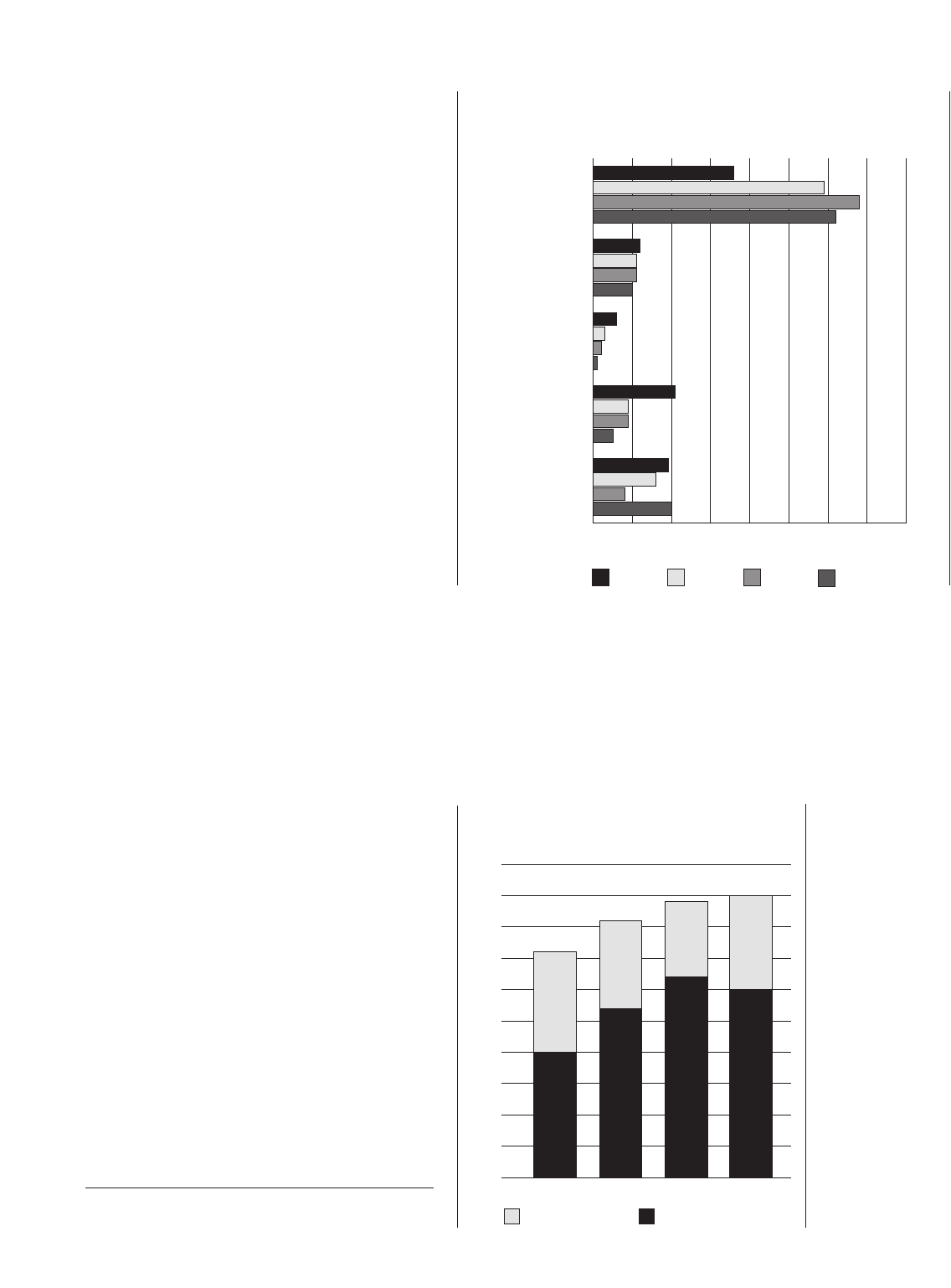
them from the Ministry of Health (see Figure 1).
3
Social
security and nongovernmental organizations served 18%
of women; precise information on method sources for the
remaining 5% was not available. The Ministry of Health’s
policy of targeting free services to poor people in rural areas
and levying service fees in urban areas likely provided an
opportunity for commercial family planning providers to
thrive: Individuals who could afford to pay for family plan-
ning products and services may have found it more con-
COMMENT
Family Planning Policies and Their Impacts
On the Poor: Peru’s Experience
James N. Gribble is
director of the
BRIDGE Project,
Population Reference
Bureau, Washington,
DC. Suneeta Sharma
is senior health
economist and
reproductive health
team leader, Health
Policy Initiative,
Constella Futures,
Washington, DC.
Elaine P. Menotti is
technical advisor,
U.S. Agency for
International
Development,
Washington, DC.
By James N.
Gribble, Suneeta
Sharma and Elaine
P. Menotti
*The components of the family planning market include providers (gov-
ernment, social security, commercial, social marketing and nongovern-
mental organizations), consumers (women of reproductive age, 15–49 years)
and contraceptive methods (long-term and temporary modern methods).
177Volume 33, Number 4, December 2007
Fund’s procurement mechanism.
9
Between 1992 and 2000, a time in which Peru’s public
sector was assuming an increasingly dominant role in the
family planning market, private providers found it difficult
to compete with such widespread provision of free or high-
ly subsidized products and services.
12
The commercial sec-
tor’s market share fell from 39% to 17% between 1992 and
2000. Between 1996 and 2000, the decline was driven pri-
marily by a 50% drop in market share for pharmacies (from
venient to purchase them from the numerous commercial
outlets available and forgo the opportunity costs associat-
ed with using Ministry of Health facilities (i.e., distance,
travel, quality of services).
Family Planning for All
In 1995, after the implementation of the ICPD Programme
of Action (under which Peru is a signatory) and with po-
litical support from the president, the Ministry of Health
instituted a policy to provide free family planning products
and services to all who wanted them. Donors provided
100% of Ministry of Health contraceptive commodities, as
well as substantial technical assistance and resources for
training; supervision; information, education and com-
munication; and other program components. As a result,
the Ministry of Health was able to direct its resources to
expansion of family planning service delivery. In 1994, the
Ministry of Health introduced an ambitious program (Salud
Básica) to expand its network of primary health care facil-
ities, whose services included family planning. The num-
ber of health posts, health clinics and health centers run
by the Ministry increased by more than 50% between 1995
and 2000, and more than 10,000 medical and paramed-
ical staff were added across the country. In addition, the
legalization of female sterilization as a contraceptive method
for all women in 1995 increased access to the method.
8
Annual government spending on health increased from 59
soles (US$18) per capita during the early 1990s to 93 soles
(US$29) per capita during the 1996–2000 period.
5
As a
result of both public-sector investments and donor sup-
port, the National Family Planning Program was deliver-
ing services through more than 6,000 facilities by the late
1990s.
9
The expansion in service delivery and availability of free
contraceptives in Ministry of Health facilities no doubt con-
tributed to the increase in contraceptive prevalence from
41% to 44% between 1996 and 2000—Figure 2. Overall,
women increased their use of modern methods from 27%
to 32%, with the poorest women increasing their modern
method use from 18% to 25% (Figure 3, page 178). In ad-
dition, the policy was responsible for the dramatic increase
in family planning market share for the Ministry of Health,
which rose from 59% in 1996 to 68% in 2000.
10,11
At the same time, donors were beginning to reduce con-
traceptive commodity donations to the government of
Peru,* potentially threatening the availability of contra-
ceptives. In response, the Peruvian government earmarked
funds for family planning in its annual budget in 1997 and
agreed to begin purchasing contraceptives in increasing
quantities. The government’s first purchase, however, was
not made until two years later, in 1999, when funding for
contraceptives was actually allocated for the first time, en-
abling the National Family Planning Program to purchase
contraceptives through the United Nations Population
FIGURE 1. Among Peruvian women aged 15–49 practicing family planning, percent-
ages obtaining services and methods from specific sources, 1992–2004
2004
2000
1996
1992
0 1020304050607080
Pharmacies
Private providers
Nongovernmental
organizations
Social Security
Ministry of Health
% of women
FIGURE 2. Contraceptive prevalence, by type of method,
among Peruvian women aged 15–49, by year, 1992–2004
Traditional methods
Modern methods
0
10
20
30
40
50
2004200019961992
% of women
*On the basis of a combination of contraceptive prevalence, total fertility
and economic indicators, donors had decided that Peru was ready to move
toward more self-sustaining family planning efforts.

178 International Family Planning Perspectives
16% to 8%).
10,11
Total commercial sales of oral contracep-
tives and injectables decreased from 1.4 million units in
1995 to 1.1 million units in 1996—and continued to decline
consistently until 2001.
9
According to several studies, public-sector prices for tem-
porary family planning methods are one of the major
determinants of the use of commercial outlets for those
methods.
13–15
Their findings show that if high-quality con-
traceptive methods are available free of charge in Ministry
of Health facilities, private-sector users are likely to switch
to these outlets. From 1996 to 2000, the share of Ministry
of Health clients made up of women in the three upper so-
cioeconomic quintiles rose from 46% to 53%, while the
share accounted for by women in the two lower quintiles
decreased from 54% to 47% (Figure 4).* Use of pharma-
cies for contraceptive supplies declined from 17% to 7%
among women in the middle quintile and from 23% to 13%
among those in the upper middle quintile.
10,11
In other
words, women with the ability to pay were benefiting from
public subsidies.
The 1995 policy expanded access to family planning and
initially adopted the focus of the ICPD Programme of Ac-
tion on individual women’s needs, instead of population
control. In 1996, however, Peru’s family planning program
returned to employing the targets it had used when first
established.
16
By 1999, the government had changed its
service delivery strategy and renounced the use of targets
and quotas; measures were put in place to improve quality
of care, including procedures to ensure informed consent
for female sterilization.
8
Changes in Commitment to Family Planning
At the beginning of the current decade, program changes
within the Ministry of Health affected family planning’s
priority status on the national agenda. From 2000 to 2003,
some government officials and prominent figures in the
Ministry of Health who opposed family planning for moral
reasons undertook deliberate measures to restrict access
to family planning products, services and information in
Peru. These measures included publicly disputing that con-
doms and IUDs were safe and effective, blocking commodity
distribution and proposing modifications to the constitu-
tion and the general health law that would restrict access
to family planning.
9,16
Although these government officials were not success-
ful in altering or removing policies that supported Peru-
vians’ access to family planning, their efforts coincided with
the introduction of health sector reforms that affected the
way in which family planning services were managed and
delivered by the Ministry of Health. Since its inception in
the 1980s, the National Family Planning Program had been
vertically planned and managed by the Ministry of Health,
as was the case for all other national health programs. At
the service delivery level, family planning was provided by
the Ministry’s clinics, often having its own program ad-
ministration and providers. In 2001, however, to improve
efficiency and to reduce the costs of managing and deliv-
ering health services, the government combined all 14 na-
tional health programs into an integrated health model that
was based on the life course and reorganized the Ministry
of Health accordingly, decentralizing management func-
Family Planning Policies and Their Impacts on the Poor
FIGURE 3. Contraceptive prevalence, by type of method, among Peruvian women
aged 15–49 in the poorest and wealthiest quintiles, by year, 1996–2004
0
10
20
30
40
50
Wealthiest
Poorest
Traditional methods
Modern methods
Quintile
1996
2000 2004 1996 2000 2004
% of women
FIGURE 4. Percentage distribution of Peru’s Ministry of
Health clients, by socioeconomic status, according to year,
1996–2004
0
10
20
30
40
50
60
70
80
90
100
200420001996
Upper middle and wealthiest
Middle
Poorest and lower middle
% of women
*Through a principal components analysis, a household’s ability to pay for
family planning is established using a standard of living index based on
number of household assets. Households are then divided into quintiles
(poorest, lower middle, middle, upper middle and wealthiest) according
to standard of living. Here we calculated the standard of living index using
the 1996, 2000 and 2004 Peru Demographic and Health Surveys.

179Volume 33, Number 4, December 2007
cess to contraceptive methods, which included a reduction
in the availability of surgical contraception, limited access
to information about contraceptives, stockouts of contra-
ceptive methods and unauthorized fees for services that
were supposed to be free in health centers.
20
Perhaps as a result of reduced access to family planning
services and commodity stockouts in Ministry of Health
facilities, the reported number of abortions increased. About
35,000 cases of incomplete abortion were treated in Min-
istry of Health facilities in both 2000 and 2001; the num-
ber rose to 38,851 in 2002 and to 41,993 in 2003.
19
Another study of family planning providers operating
in Ministry of Health facilities, conducted between 2002
and 2004, provides further insight.
21
In the 2002–2003
round of the study, 34% of the 238 providers interviewed
reported that, in the 12 months prior to the survey, the
method supply was continuous; 40% thought that the sup-
ply was sufficient and 25% indicated that the supply was
both continuous and sufficient. However, in the 2003–2004
round of the study, only 6% of 242 providers interviewed
stated that the supply of contraceptives had been contin-
uous; 17% thought the supply of methods was sufficient
and 2% reported that the supply of methods was both con-
tinuous and sufficient. Also, in this round of the study, 83%
of providers said that when facing stockouts of contraceptive
commodities—especially injectables and oral contracep-
tives—they advised their patients to use another method
temporarily, with 60% providing a prescription to be filled
at a commercial outlet or pharmacy and 23% changing the
patient’s contraceptive method to one in stock. These find-
ings reveal not only reduced access, but also reduced qual-
ity of family planning services—which was likely to affect
use—especially among women who could not afford com-
mercial sector prices.
DISCUSSION
Peru’s family planning policies have, in general, been de-
signed to address all women’s needs. Some policies, how-
ever, focus particularly on the poor, in accordance with the
public sector’s mandate to serve people whose access to
and receipt of preventive and curative health services and
products depends on subsidies and assistance. The evidence
presented here suggests that the poor are particularly vul-
nerable to unanticipated policy outcomes, highlighting the
need for well-designed policies and significant thought
about both implementation and consequences. As Figure
4 shows, wealthier Peruvian woman made up an increas-
ing share of government family planning clients between
1996 and 2004. This fact reveals a universal lesson: Given
that developing countries have limited resources, provid-
ing universal coverage through the public sector, although
conceptualized as a strategy to reach the poor, often ends
tions to the regions, eliminating separate budgets and down-
sizing or reassigning family planning staff to other Ministry
of Health divisions. As a result, the Ministry of Health lost
its core expertise in family planning at the central level, along
with its ability to plan, supervise and monitor family plan-
ning services.
9
The change in the model of care created bar-
riers for family planning clientele, including less privacy,
lack of educational materials, long waiting times and the
requirement of a visit to the hospital or clinic pharmacy
after consultation.
1,17
Additionally, an economic crisis strik-
ing the country in the early 2000s decreased per capita ex-
penditures for health from 95 soles (US$30) in 2001 to 88
(US$27) in 2002 and 78 (US$24) in 2003.
5
During the same period, donors continued to reduce con-
traceptive commodity donations to the government of Peru.
In 2002, as part of the donor contraceptive commodity
phase-out plan, the government declared that contracep-
tives were strategic public health commodities,* which
helped to ensure that contraceptives received special pro-
tection and funding in the national budget. However, the
government’s inability to compensate for decreased donor
funding left the Ministry of Health unable to meet the de-
mand for contraceptives. As a result, from 2002 through
2004, government facilities experienced stockouts of con-
traceptives. Logistic problems, such as poor planning and
information systems, a long supply chain and insufficient
or incorrect commodity mix, exacerbated the problem.
After a steady increase during the previous decade, con-
traceptive use stagnated at 44% in 2004, likely a result of
stockouts and a weakened family planning program. Mod-
ern method use declined in 2004, especially among those
in the poorest quintile, but stayed stable among the wealth-
iest quintile. Although use of traditional methods declined
from 14% in 1996 to 12% in 2000, their use rose again to
15% in 2004. This increase occurred in all quintiles except
the wealthiest. In the poorest quintile, use of traditional meth-
ods increased from 14% to 23% between 2000 and 2004.
18
Also between 2000 and 2004, Ministry of Health’s mar-
ket share shrank from 68% to 62%; this was most likely
due to the government’s insufficient funding for com-
modities. Interestingly, during the same period, the com-
mercial sector’s market share rebounded from 17% to 25%,
dominated by pharmacies. The shift back to the commer-
cial sector was led by women of the two wealthiest quin-
tiles, who doubled their use of pharmacies between 2000
and 2004.
11,18
Studies that focus on the experiences of public- and
private-sector providers further elucidate the changes that
took place in the Ministry of Health program between 2000
and 2004. One study found a decline in family planning
services in the Ministry of Health, including an absence
of follow-up, evaluation and training activities; a lack of
regard for family planning and reproductive health as
national priority issues by certain health officials and polit-
ical leaders; and periods of stockouts of contraceptives that
affected users for many months.
19
The Ombudsman’s
Office reported consumer complaints about restricted ac-
*Many of Peru’s programs, such as those for tuberculosis, HIV/AIDS, and
sexual and reproductive health, have been converted from vertical pro-
grams into “Health Strategies,” interventions for which it is the responsi-
bility of the government to carry out objectives. The Ministry of Health is
therefore responsible for making available to the public the medicines and
supplies critical to the success of these strategies.

180 International Family Planning Perspectives
up serving a considerable proportion of people who can
afford to pay for care and restricts access among those peo-
ple who can least afford it.
In Peru, increasing service availability and providing free
donated contraceptives through the Ministry of Health in-
creased contraceptive prevalence for all women in the short-
term, but likely reduced the role of the commercial sector
and shifted some wealthier clients to the Ministry of Health.
The 1995 policy decision had the positive impact of in-
creasing contraceptive use among women in the lowest two
socioeconomic quintiles and those in rural areas. From 1996
to 2000, women in the poorest quintile increased use of
modern methods. However, from 2000 to 2004, use of mod-
ern methods declined in the poorest quintiles, and use of
traditional methods among these groups increased. The
general trend between 1996 and 2004 shows that the pro-
portion of Ministry of Health clients from the wealthiest
quintiles increased over time and that the proportion from
the two poorest quintiles decreased. In light of the fact that
the Ministry of Health’s per capita financial resources have
declined, priority should be given to refocusing those re-
sources on the poorest groups, who have no other option
for health services and products.
Although the overall trend in contraceptive prevalence
shows a leveling off of modern method use from 2000 to
2004, closer analysis by socioeconomic subgroups shows
that the plateau in levels of use was not universal; use of
modern methods declined in the two poorest quintiles be-
tween 2000 and 2004. A number of factors could explain
why poor women—especially those in rural areas—decreased
their use of modern contraceptives and increased their use
of traditional methods: reduced access to family planning
facilities, methods of choice or information in rural areas
as a result of service integration; contraceptive stockouts
in rural Ministry of Health facilities; levying of unofficial
fees in public health centers; the inability to pay for meth-
ods in private-sector outlets; and the public discrediting of
modern methods. Even if services for the poor were read-
ily available, misinformation often affects women’s inter-
est in seeking family planning methods and services. A re-
cent study conducted among rural, poor Peruvian women
found that misinformation about family planning meth-
ods discourages contraceptive use; however, these women
also indicated a strong interest in receiving information
about family planning methods.
22
These findings also sug-
gest that for policies designed to improve access among the
poor to be effective, they must also address a wider range
of barriers that undermine utilization of services.
Improving Access Among the Poor
Currently, the government of Peru is taking steps to address
the decline in modern method use among the poor and to
improve access to accurate information. The use of condi-
tional cash transfers, which is in the process of being im-
plemented, and the expansion of services under social in-
surance programs may increase access to modern family
planning methods among the poor.
•Conditional cash transfers. Peru is in the early stages of
rolling out a conditional cash transfer program as part of
a poverty alleviation strategy. To date, the program has been
implemented in 14 of Peru’s poorest regions. The program
provides 100 soles monthly (approximately US$31) to
women who complete certain requirements, which include
registering births, immunizing their children, obtaining
prenatal care and supplementary nutrition and ensuring
their children’s school attendance. In addition, women have
the opportunity to participate in information sessions on
family planning and reproductive health.
•Social insurance programs. Peru has implemented a so-
cial insurance program that covers a range of curative and
preventive health services for children, adolescents, preg-
nant women, the very poor and other vulnerable groups.
In March 2007, the president of Peru and the minister of
health signed a resolution to expand the package of bene-
fits to include provision of family planning services and com-
modities. Given that the social insurance program is actu-
ally more successful in reaching the poor in general with
its current care package than the Ministry of Health is in
reaching the poor with family planning,
23
it is a promising
mechanism for ensuring that the poor have access to fam-
ily planning information, services and methods.
Conclusion
Peru’s experience reveals that when well-intentioned poli-
cies are implemented, they can have adverse outcomes on
the people they are designed to help. Consequently, poli-
cymakers must think through both the short- and long-term
consequences of policies prior to implementation. More-
over, as the experience of Peru demonstrates, they should
continuously monitor and evaluate how policies are being
implemented and be willing to make adjustments when it
is clear that a policy is not achieving its desired outcomes.
REFERENCES
1. Subiria, G, Informe de disponibilidad asegurada de insumos anti-
conceptivos región Junín, internal document, Lima, Peru: Iniciativa de
Políticas en Salud, 2006.
2. Sobrevilla LA, Peru: population and policy, Population Manager, 1987,
1(1):40–44.
3. Instituto Nacional de Estadística e Informática, Asociación Benéfica
PRISMA and Macro International, Perú Encuesta Demográfica y de Salud
Familiar, 1991/1992, Columbia, MD, USA: Macro International, 1992.
4. Angeles G, Guilkey DK and Mroz TA, The determinants of fertility
in rural Peru: program effects in the early years of the national family
planning program, Journal of Population Economics, 2005, 18(2):367–
389.
5. Asociación Pro Derechos Humanos (APRODEH) and Centro de
Asesoría Laboral del Perú (CEDAL), Informe Sobre la Situación de los
Derechos Económicos, Sociales y Culturales 2002–2003: Dos Años de
Democracia . . . y ¿los DESC?, Lima, Peru: APRODEH and CEDAL, 2005.
6. United Nations Population Fund (UNFPA), Global Population
Assistance Report 1995, New York: UNFPA, 1997.
7. UNFPA, Financial Resource Flows for Population Activities in 2004, New
York: UNFPA, 2006.
8. Leon FR, Providers’ Compliance with Quality of Care Norms, Lima, Peru:
Population Council, 1999.
9. Taylor PA et al., Peru: Contraceptive Security Assessment, September 1–12,
Family Planning Policies and Their Impacts on the Poor

181Volume 33, Number 4, December 2007
International, Perú Encuesta Demográfica y de Salud Familiar, 2004,
Calverton, MD, USA: ORC Macro, 2004.
19. Ferrando D, El aborto clandestino en el Perú: nuevas evidencias,
PowerPoint presentation, Lima, Peru: Flora Tristan and Pathfinder
International, 2004.
20. Defensoria del Pueblo, La anticoncepción quirúrgica y los dere-
chos reproductivos III, casos investigados por la Defensoría del Pueblo,
Informe Defensorial No. 69, Lima, Peru: Defensoria del Pueblo, 2002.
21. Proyecto POLICY/Peru, Encuesta de Proveedores de Planificación
Familiar en el Ministerio de Salud, Lima, Peru: Proyecto POLICY, 2005.
22. Diaz M, Reporte de Actividades: Grupos Focales con Mujeres Pobres,
Lima, Peru: Iniciativa de Políticas en Salud, 2006.
23. Petrera M, Evaluación de la Inclusión de Atenciones de Planificación
Familiar en los Planes de Beneficios del Seguro Integral de Salud, Lima, Peru:
Iniciativa de Políticas en Salud, 2006.
Acknowledgments
The authors wish to acknowledge Roberto Lopez, Patricia Mosta-
jo, Varuni Dayaratna, Rebecka Lundgren, Nancy Murray, Carol
Shepherd and Gracia Subiria for reviewing drafts of this comment.
The U.S. Agency for International Development (USAID) Health
Policy Initiative provided partial funding for this project under con-
tract GPO-I-01-05-00040-00. The views expressed in this comment
are those of the authors and do not necessarily reflect the views of
USAID or the U.S. government.
Author contact: jg[email protected]
2003, Arlington, VA: John Snow/DELIVER, and Washington, DC: Futures
Group International/POLICY II, 2004.
10. Instituto Nacional de Estadística e Informática and Macro
International, Perú Encuesta Demográfica y de Salud Familiar, 1996,
Calverton, MD, USA: ORC Macro, 1996.
11. Instituto Nacional de Estadística e Informática and Macro
International, Perú Encuesta Demográfica y de Salud Familiar, 2000,
Calverton, MD, USA: ORC Macro, 2000.
12. Sharma S, Gribble JN and Menotti EP, Creating options in family
planning for the private sector in Latin America, Pan American Journal
of Public Health, 2005, 18(1):37–44.
13. Foreit KGF, Broadening commercial sector participation in repro-
ductive health: the role of public sector prices on markets for oral con-
traceptives, Commercial Market Strategies Technical Paper Series,
Washington, DC: Commercial Market Strategies, 2002, No. 3.
14. Bulatao R, What influences the private provision of contraceptives?
Commercial Market Strategies Technical Paper Series, Washington, DC:
Commercial Market Strategies, 2002, No. 2.
15. Winfrey W et al., Factors influencing the growth of the commer-
cial sector in family planning service provision, POLICY Project Working
Paper, Washington, DC: Futures Group International, 2000, No. 6.
16. Coe AB, From anti-natalist to ultra-conservative: restricting repro-
ductive choice in Peru, Reproductive Health Matters, 2004, 12(24):56–69.
17. Sarley D et al., Options for Contraceptive Procurement: Lessons Learned
from Latin America and the Caribbean, Arlington, VA, USA: DELIVER,
and Washington, DC: USAID Health Policy Initiative, 2006.
18. Instituto Nacional de Estadística e Informática and Macro
