1
ID NOW COVID-19
For Use Under an Emergency Use Authorization – US only (EUA)
For use with the ID NOW Instrument
For use with anterior nasal, throat or nasopharyngeal specimens
For in vitro Use
Rx Only
INTENDED USE
ID NOW COVID-19 assay performed on the ID NOW Instrument is a rapid molecular in vitro diagnostic
test utilizing an isothermal nucleic acid amplification technology intended for the qualitative detection of
nucleic acid from the SARS-CoV-2 virus in direct anterior nasal (nasal), nasopharyngeal or throat swabs
from individuals who are suspected of COVID-19 by their healthcare provider within the first seven days of
the onset of symptoms. Testing is limited to laboratories certified under the Clinical Laboratory
Improvement Amendments of 1988 (CLIA), 42 U.S.C. §263a, that meet the requirements to perform high,
moderate, or waived complexity tests. The ID NOW COVID-19 assay is also authorized for use at the Point
of Care (POC), i.e., in patient care settings operating under a CLIA Certificate of Waiver, Certificate of
Compliance, or Certificate of Accreditation.
Results are for the identification of SARS-CoV-2 RNA. The SARS-CoV-2 RNA is generally detectable in
respiratory samples during the acute phase of infection. Positive results are indicative of the presence of
SARS-CoV-2 RNA; clinical correlation with patient history and other diagnostic information is necessary
to determine patient infection status. Positive results do not rule out bacterial infection or co-infection with
other viruses. The agent detected may not be the definite cause of disease. Testing facilities within the
United States and its territories are required to report all results to the appropriate public health authorities.
Negative results should be treated as presumptive and, if inconsistent with clinical signs and symptoms or
necessary for patient management, should be tested with different authorized or cleared molecular tests.
Negative results do not preclude SARS-CoV-2 infection and should not be used as the sole basis for patient
management decisions. Negative results should be considered in the context of a patient’s recent
exposures, history and the presence of clinical signs and symptoms consistent with COVID-19.
The ID NOW COVID-19 test is intended for use by medical professionals or trained operators who are
proficient in performing tests using the ID NOW Instrument. The ID NOW COVID-19 test is only for use
under the Food and Drug Administration’s Emergency Use Authorization.
SUMMARY AND EXPLANATION OF THE TEST
Coronaviruses are a large family of viruses which may cause illness in animals or humans. SARS-CoV-2 is
an enve loped, single-stranded RNA virus of the β genus. The virus can cause mild to severe respiratory
illness and has spread globally, including the United States.
ID NOW COVID-19 is a rapid (13 minutes or less), instrument-based isothermal test for the qualitative
detection and diagnosis of SARS-CoV-2 from nasal, nasopharyngeal and throat swabs. The ID NOW
Instrument has a small footprint and easy to use graphical user interface for convenience within a busy
hospital or near patient testing environments. The ID NOW CO V ID-19 kit contains all components required
to carry out an assay for SARS-CoV-2 on the ID NOW Instrume nt.

2
PRINCIPLES OF THE PROCEDURE
ID NOW COVID-19 is an automated assay that utilizes isothermal nucleic acid amplification technology for
the qualitative detection of SARS-CoV-2 viral nucleic acids. It is comprised of a Sample Receiver, containing
elution/lysis buffer, a Test Base, comprising two sealed reaction tubes, each containing a lyophilized pellet,
a Transfer Cartridge for transfer of the eluted sample to the Test Base, and the ID NOW Instrument.
The reaction tubes in the Test Base contain the reagents required for amplification of SARS-CoV-2, as well
as an internal control. The templates (similar to primers) designed to target SARS-CoV-2 RNA amplify a
unique region of the RdRp segment. Fl u ore scently-labeled molecular be acons are use d to specifically
identify each of the amplified RNA targets.
To perform the assay, the Sample Receiver and Test Base are inserted into the ID NOW Instrument. The
sample is added to the Sample Receiver and transferred via the Transfer Cartridge to the Test Base,
initiating target amplification. Heating, mixing and detection are provided by the instrument.
REAGENTS AND MATERIALS
Materials Provided
Test Bases: Orange plastic components containing two re action tubes of lyophilized
reagents for the targeted amplification of SARS-CoV-2 viral RNA
and an internal
control.
Sample Receivers: Blue plastic components containing 2.5 mL of elution buffer.
Transfer Cartridges: White p lastic comp onents us ed to tr
ansfe r 2 x 100 µL of sample
extract from the Sample Receiver to the Test Base.
Patient Swabs: Sterile swabs (foam) for use with the ID NOW COVID-19 Test.
Positive Control Swab: The positive control swab ensures sample elution/lysis and workflow
were performed correctly.
Negative Control Swab: The use of a sterile patient swab ensures appropriate negative results
are obtained.
Package Insert
Quick Reference Instructions
Materials Required but not Provided
ID NOW Instrument
Nasopharyngeal Swabs
PRECAUTIONS
1. For in vitro diagnostic use under the FDA Emergency Use Authorization.
2. For prescription use only.
3. This product has not been FDA cleared or approved; but has been authorized for emergency use by
FDA under an EUA for use by authorized laboratories.
4. This product has been authorized only for the detection of nucleic acid from SARS-CoV-2, not for
any other viruses or pathogens.
5. The emergency use of this product is only authorized for the duration of the declaration that
circumstances exist justifying the authorization of emergency use of in vitro diagnostics for
detection and/or diagnosis of COVID-19 under Section 564(b)(1) of the Federal Food, Drug, and
Cosmetic Act, 21 U.S.C. § 360bbb-3(b)(1), unless the declaration is terminated or authorization is
revoked sooner.
6. This product has been authorized by FDA under an EUA for use by laboratories certified under the
3
Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. §263a, to perform high,
moderate, or waived complexity tests and for use at the Point of Care (POC), i.e., in patient care
settings operating under a CLIA Certificate of Waiver, Certificate of Compliance, or Certificate of
Accreditation.
7. Federal Law restricts this device to sale by or on the order of a licensed practitioner (US only).
8. This test has been authorized only for the detection of nucleic acid from SARS-CoV-2, not for any
other viruses or pathogens.
9. Laboratories within the United States and its territories are required to report all results to the
appropriate public health laboratories.
10. To be used in conjunction with the ID NOW Instrument.
11. Treat all specimens as potentially infectious. Follow universal precautions when handling samples,
this kit and its contents.
12. Proper sample collection, storage and transport are essential for correct results.
13. Leave test pieces sealed in their foil pouches until just before use.
14. Do not tamper with test pieces prior to or after use.
15. Do not use kit past its expiration date.
16. Do not mix components from different kit lots or from other ID NOW assays.
17. Solutions used to make the p ositive control swab are inactivated using standard methods. However,
patient samples, controls, and test pieces should be handled as though they could transmit disease.
Observe established precautions against microbial hazards during use and disposal.
18. Wear clean personal protection equipment and gloves when running each te st. Change gloves
between the handling of specimens suspected of COVID-19.
19. If any assay components are dropped, cracked, found to be damaged or opened when
received, DO NOT USE and discard. Do not use scissors or sharp objects to open foil
pouches as damage to test pieces can occur.
20. Do not open the Sample Receiver before placing in the instrument. It will prohibit the Elution
Buffer from reaching temperature and may impact test performance.
21. If the Sample Receiver is spilled while opening, clean the instrument per instructions provided in
the instrument User Manual and cancel test. Repeat test with a new Sample Receiver.
22. All test pieces must be removed from the instrument according to removal instructions displayed
on the instrument and disposed of according to country and local requirements. Pieces must not
be separated once they are assembled.
23. All test pieces are single use items. Do not use with multiple specimens.
24. Once reacted, the Test Base contains large amounts of amplified target (Amplicon). Do not
disassemble the Test Base and Transfer Cartridge. In the case of a positive sample, this
could lead to amplicon leakage and potential ID NOW COVID-19 false positive test results.
25. At a low frequency, clinical samples can contain inhibitors that may generate invalid results. Site
to site invalid rates may vary.
26. Due to the high sensitivity of the assays run on the instrument, contamination of the work area with
previous positive samples may cause false positive results. Handle samples according to standard
laboratory practices. Clean instruments and surrounding surfaces according to instructions
provided in the cleaning section of the instrument User Manual. Refer to Section 1.6, Maintenance
& Cleaning, for further information.
STORAGE AND STABILITY
Store kit at 2-30°C. The ID NOW COVID-19 kit is stable until the expiration date marked on the outer
packaging and containers. Ensure all test components are at room temperature before use.
QUALITY CONTROL
ID NOW COVID-19 has built-in procedural controls. The result of the Procedural Control is d isplayed on
the screen and is automatically stored in the instrument with each test result. This can be reviewed later by
selecting Review Memory on the instrument.

4
Procedural Controls:
ID NOW COVID-19 contains an internal control that has been designed to control for sample inhibition and
assay reagent function. In positive samples where target amplification is strong, the internal control is
ignored, and the target amplification serves as the ‘control’ to confirm that the clinical sample was not
inhibitory, and that assay reagent performance was robust. At a very low frequency, clinical samples can
contain inhibitors that may generate invalid results.
Procedural Control Valid displayed on the instrument screen indicates that the assay reagents m aintained
their functional integrity and the sample did not significantly inhibit assay performance.
External Positive and Negative Controls:
Good laboratory practice suggests the use of positive and negative controls to ensure that test reagents are
working and that the test is correctly performed. ID NOW COVID-19 kits contain a Positive Con t rol Swab
and Sterile Swabs that can be used as a Negative Control Swab. These swabs will monitor the entire assay.
Test these swabs once with each new shipment received and once for each untrained operator. Further
controls may be tested in order to conform with local, state and/or federal regulations, accrediting groups,
or your lab’s standard Quality Control procedures.
CONTROL SWAB PROCEDURE
Positive and Negative Controls should be tested following the Run QC Test instructions on the ID NOW
Instrument. A Positive Control Swab is included in the kit. Use a sterile swab provided in the kit as the
Negative Control Swab. Refer to Quality Control Swab Test Procedure or Instrument User Manual for
further details.
Note: The ID NOW Instrument reports QC results as Pass or Fail.
If the correct control results are not obtained, do not perform patient tests or report patient results. Contact
Technical Support during normal business hours before testing patient specimens.
SPECIMEN COLLECTION AND HANDLING
Use freshly collected specimens for optimal test performance. Inadequate specimen collection or improper
sample handling/storage/transport may yield erroneous results. Refer to the CDC Interim Guidelines for
Collecting, Handling, and Testing Clinical Specimens from Persons for Coronavirus Disease 2019 (COVID-
19) https://www.cdc.gov/coronavirus/2019-nCoV/lab/guidelines-clinical-specimens.html
ID NOW COVID-19 is intended for testing a swab directly without elution in viral transport media as
dilution will result in decreased detection of low positive samples that are near the limit of detection of the
test.
Follow Standard Precautions when handling clinical specimens, all of which may contain potentially
infectious materials. Standard Precautions include hand hygiene and the use of personal protective
equipment (PPE), such as laboratory coats or gowns, gloves, and eye protection.
To minimize risk of contamination of PPE and swab package during sample collection, it is recommended
to widely open the package by pulling from the top down. Carefully remove the swab and perform sample
collection.
Throat Swab
For optimal test performance, use the swabs provided in the test kit. Alternatively, foam, polyester,
Hy draFlock® and nylon flocked throat swabs can be used to collect throat swab samples.
Rayon swabs are not suitable for use in this assay.
5
Collect patient specimen by swabbing the posterior pharynx, tonsils and other inflamed areas. Avoid
touching the tongue, cheeks and teeth with the swab.
1
Nasal Swab
For optimal test performance, use the swabs provided in the test kit. Alternatively, rayon, foam,
HydraFlock® Flocked swab (standard tip), HydraFlock® Flocked swab (mini tip), Copan Mini Tip Flocked
Swab, or Copan Standard Flocked swabs can be used to collect nasal swab samples.
Puritan PurFlock Standard Tip Ultra Flocked Swabs, Puritan PurFlock Mini Tip Ultra Flocked Swabs and
Copan Standard Rayon Tip Swabs are not suitable for use in this assay.
To collect a nasal swab sample, carefully insert the swab into the nostril exhibiting the most visible drainage,
or the nostril that is most congested if drainage is not visible. Using gentle rotation, push the swab until
resistance is met at the level of the turbinates (less than one inch into the nostril). Rotate the swab several
times against the nasal wall then slowly remove from the nostril. Using the same swab, repeat sample
collection in the other nostril.
Nasopharyngeal Swab
Use sterile rayon, foam, polyester or flocked flexible-shaft NP swabs to collect a nasopharyngeal sample.
To collect a nasopharyngeal swab sample, carefully insert the swab into the nostril exhibiting the most
visible drainage, or the nostril that is most congested if drainage is not visible. Pass the swab directly
backwards without tipping the swab head up or down. The nasal passage runs parallel to the floor, not
parallel to the bridge of the nose. Using gentle rotation, insert the swab into the anterior nare parallel to the
palate advancing the swab into the nasopharynx, leave in place for a few seconds, and then slowly rotate
the swab as it is being withdrawn.
To ensure proper collection, the swab should be passed a distance that is halfway of that from the nose to
the tip of the ear. This is about half the length of the swab. DO NOT USE FORCE while inserting the swab.
The swab should travel smoothly with minimal resistance; if resistance is encountered, withdraw the swab
a little bit without taking it out of the nostril. Then elevate the back of the swab and move it forward into
the nasopharynx.
SPECIMEN TRANSPORT AND STORAGE
For best performance, direct nasal, throat or nasopharyngeal swabs should be tested as soon as possible
after collection. If immediate testing is not possible, and to maintain best performance, it is highly
recommended the nasal, throat or nasopharyngeal swab is placed in a clean, unused tube labeled with
patient information, and capped tightly at room temperature (15-30°C) for up to one (1) hour prior to
testing. Ensure the swab fits securely within the tube and the cap is tightly closed. If greater than one (1)
hour delay occurs, dispose of sample. A new sample must be collected for testing.
If the swab is to be returned to its package for transport, carefully return to allow the swab head to only
come into contact with the lower portion of the packaging. Avoid touching the outside of the wrapper with
the swab.
TEST PROCEDURE
Please refer to the ID NOW Instrument User Manual for full instructions.
Before testing with ID NOW COVID-19:
• Put on a clean pair of gloves.
• Allow all samples to reach room temperature.
• Allow all test pieces to reach room temperature.

6
• Check that a reagent pellet is visible at the bottom of each of the reaction tubes prior to inserting
the Test Base in the ID NOW Instrument. Do not use the Test Base if a pellet is not visible at the
bottom of each reaction tube.
To Perform a Test:
Step 1
Turn on the ID NOW Instrument - press the power button
on the side of the instrument.
Note: If the unit is unattended for one hour, the instrument
will go to a black screen power save mode. Touch the screen
to return the unit to active display operation.
Enter User ID
Press ‘’ after entry.
Touch ‘Run Test’
This will begin the test process.
Touch ‘COVID-19 Test’
This starts a COVID-19 te st.
Select Swab Sample Type (if prompted)
If the sample type has already been specified by the Admin,
the instrument will automatically advance to the next step.
Caution: VTM Samples are not an appropriate
sample type for the ID NOW COVID-19 test.

7
Enter Patient ID using on screen keyboard or barcode
scanner.
Touch ‘’.
Verify that the ID was entered correctly, then touch ‘’ to
confirm entry.
Step 2
Open the Lid and Insert Orange Test Base into
Orange Test Base holder
Caution: Do not apply excessive force. Excessive
force could damage the instrument.
Confirm that the correct test is displayed on the
screen.
Touch ‘OK’ to proceed.
Caution: Once the Test Base has been placed in the
holder, the user will have 10 minutes to confirm the
test. If the test is not confirmed within 10 minutes,
the instrument will time out and the Test Base must
be removed and discarded.
If the incorrect Test Base has been inserted, remove and
dispose of the incorrect Test Base. Close the lid. The
instrument will then run a self-test before proceeding to the
Home screen. Press Run Test and restart the test using the
correct Test Base.
Step 3
Insert Blue Sample Receiver into the Blue Sample
Receiver holder
Caution: Do not apply excessive force. Excessive
force could damage the instrument.
Caution: Once the Sample Receiver has been placed
in the holder, the user will have 10 minutes to start
the test (Steps 3 through 5). If the test is not started
within 10 minutes, the instrument will time out and

8
all test pieces (Test Base and Sample Receiver) must
be removed and discarded. The instrument will
proceed to the Home screen. Press Run Test and
restart the test using a new Test Base and Sample
Receiver.
Wait for the Sample Receiver to Warm Up. Do not
remove the Sample Receiver from the instrument
once Warm Up begins.
Caution: DO NOT REMOVE THE FOIL SEAL
UNTIL PROMPTED BY THE INSTRUMENT. DO
NOT close the lid or insert the sample until prompted by
the instrument.
Step 4
Direct Nasal, Throat or Nasopharyngeal Swab Test
Procedure
When prompted, remove the foil seal and place the
patient swab to be tested into the Sample Receiver.
Mix the swab in the liquid for 10 seconds. This helps
remove the sample from the swab. Lift the swab out of the
liquid and press the swab head against the side of the
Sample Receiver to remove excess liquid. Once the swab is
removed, touch ‘OK’ to proceed.
Discard the swab into a biohazard waste container.
Caution: To ensure that the Sample Receiver
remains in the instrument while removing the foil
seal, place two fingers along the outer edge of the
Sample Receiver to hold it in place. If the Sample
Receiver spills after warm up, cancel the test by
pressing the Home button. Remove and discard the
test pieces (Sample Receiver and Test Base) and
clean the instrument. Press Run Test to start a new
test using a new Test Base and Sample Receiver.
Step 5a
Press the White Transfer Cartridge into the Blue
Sample Receiver
Listen for a click.
When the Transfer Cartridge is properly attached to the
Sample Receiver, the orange indicator on the Transfer

9
Cartridge will rise. If the orange indicator does not rise,
continue pushing onto the Sample Receiver until it does.
Caution: The orange indicator should be observed
closely. If the orange indicator does not fully rise,
the Transfer Cartridge may not collect enough
sample.
Step 5b
Lift and then connect the Transfer Cartridge to the
Test Base
When the Transfer Cartridge is properly attached to the Test
Base, the orange indicator on the Transfer Cartridge will
descend. If the orange indicator does not descend, continue
pushing onto the Test Base until it does.
Caution: If the orange indicator does not fully
descend, not enough sample will be dispensed.
This may potentially result in invalid or false test
results.
Step 6
Close the Lid.
DO NOT OPEN THE LID until the Test Complete
message appears on the screen.
Note: The test will be cancelled if the lid is opened.
Caution: This screen will be displayed for up to 30
seconds once the Transfer Cartridge is detected. If
the instrument does not detect that the lid has been
closed by then, it will time out and all test pieces
(Sample Receiver, Test Base, and Transfer
Cartridge) must be removed and discarded. The
instrument will proceed to the Home screen.
Collect a new sample from the patient. Press Run
Test and restart the test using a new Test Base and
Sample Receiver.
Caution: DO NOT OPEN THE LID. The test will be
cancelled and all test pieces (Sample Receiver, Test
Base, and Transfer Cartridge) must be removed and
discarded. A test result will not be reported or saved
in the instrument memory.
When amplification and detection is complete, the
instrument will automatically save the data before
advancing to the re sults screen.
Caution: The test is not saved until the completed
result is displayed. Do not open the lid until the
results are displayed.

10
The Test Results screen displays either a Negative or
Positive result for a successfully completed test. If a test
error occurs, the display will read ‘Invalid’. Refer to the
Result Interpretation Section for Interpretation of Results.
Press Print to print test results, press New Test to
run another test, Press Home to return to the Home
screen
After printing, or if New Test or Home are selected, the
instrument will prompt to open the lid and discard the used
test pieces.
Remove test pieces by lifting the Transfer Cartridge attached
to the Test Base, and clicking it into the Sample Receiver, by
pressing into the Sample Receiver.
Caution: Do not try to remove the Sample Receiver
by any other method as there is a risk of spilling the
patient sample.
All test pieces will be connected and can now be removed
from the instrument and disposed of according to federal,
state and local regulations.
Caution: DO NOT disassemble the Transfer
Cartridge and the Test Base before disposal.
Close the lid. The instrument will then run a Self-Test before
showing the Home screen or Enter Patient ID screen,
depending on the previous selection.
Remove and dispose of gloves.
Quality Control Swab Test Procedure
For QC testing, select Run QC Test on the Home screen, and follow the displayed instructions. Refer to
Running a QC Test in the ID NOW Instrument User Manual for further details.
1. Touch ‘Run QC Test’

11
2. Touch ‘COVID-19’
3. Select the QC Test to be Run
4. Confirm Test
Confirm the test type to match the QC sample intended
for testing by touching ‘OK’ and following the on screen
prompts to complete testing.
The use has the option to enter an ID for the QC Sample
being run.
Note: The QC test is run in the same manner as a Direct
Nasal/Throat/Nasopharyngeal Swab Patient Test. See
the To Perform a Test section above for step by step
instructions for direct nasal/throat/ nas o pharyngeal
swab samples.

12
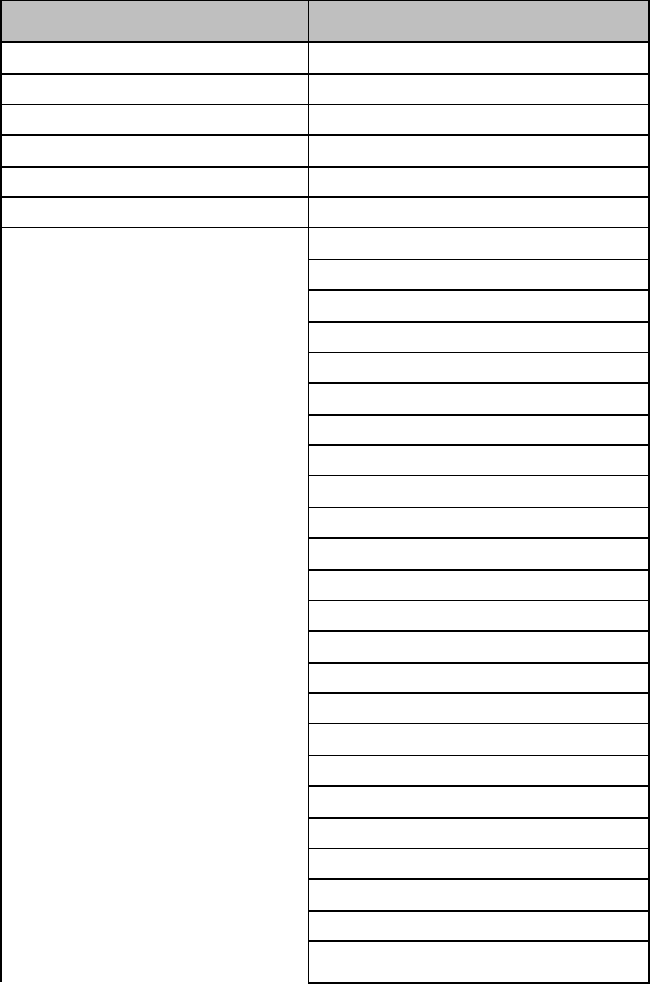
RESULT INTERPRETATION
When the test is complete, the results are clearly displayed on the instrument screen.
Instrument Display
Interpretation of Results and Follow-up Actions
COVID-19 Positive
Positive results do not rule out bacterial infection or co-
infection with other viruses.
COVID-19 Negative
Negative results should be treated as presumptive and, if inconsistent with
clinical signs and symptoms or necessary for patient management, should be
tested with an alternative molecular assay.
A ne gative result does not rule out co-infections with other pathogens.
The presence or absence of COVID-19 Viral RNAs cannot be
determined.
Repeat testing of the sample using new test components. If repeated Invalid
results are obtained, results should be confirmed by another method prior to
reporting the results.
If an Invalid result is received, one additional test may be run using the same Sample Receiver. The
instructions below should be followed:
• Remove the connected Test Base and Transfer Cartridge from the instrument and connect the Test
Base portion to an open, UNUSED Sample Receiver. The connected Test Base and Transfer
Cartridge MUST be attached to a Sample Receiver prior to disposal. The Sample Receiver from a
new Transfer Cartridge package may be used for this.
• Remove the blue Sample Receiver separately and carefully from the instrument. The Sample
Receiver should be retained and kept upright to avoid spilling the liquid contents.
• From the Home Screen, start a new test. Follow the screen prompts; however, when asked to insert
the Sample Receiver, reuse the Sample Receiver and DO NOT re-elute the swab.
LIMITATIONS
• The performance of the ID NOW COVID-19 test was evaluated using the procedures provided in this
product insert only. Modifications to these procedures may alter the performance of the test.
• Negative results should be treated as presumptive and tested with an alternative FDA authorized
molecular assay, if necessary for clinical management, including infection control.
• False negative results may occur if a specimen is improperly collected, transported or handled. False
negative results may also occur if amplification inhibitors are present in the specimen or if inadequate
levels of viruses are present in the specimen. Negative results should be considered in the context of a
patient’s recent exposures, history and the presence of clinical signs and symptoms consistent with
COVID-19.

13
• As with any molecular test, mutations within the target regions of the Abbott ID NOW COV ID-19 test
could affect primer and/or probe binding resulting in failure to detect the presence of the virus.
•
The test cannot rule out diseases caused by other bacterial or viral pathogens.
• ID NOW COVID-19 is intended for testing a swab directly without elution in viral transport media as
dilution will result in decreased detection of low positive samples that are near the limit of detection of
the test.
• Swab samples eluted in VTM are not appropriate for use in this test.
• The clinical performance has not been established in all circulating variants but is anticipated to be
reflective of the prevalent variants in circulation at the time and location of the clinical evaluation.
Performance at the time of testing may vary depending on the variants circulating, including newly
emerging strains of SARS-CoV-2 and their prevalence, which change over time.
CONDITIONS OF AUTHORIZATION FOR LABORATORIES
The ID NOW COVID-19 Letter of Authorization, along with the authorized Fact Sheet for Healthcare
Providers, the authorized Fact Sheet for Patients, and authorized labeling are available on the FDA website:
https://www.fda.gov/medical-de vices/coronavirus-disease-2019-cov id-19-emergency-use-
authorizations-medical-devices/in-vitro-diagnostics-euas.
However, to assist clinical laboratories and patient care settings (authorized laboratories
1
) using the ID
NOW COVID-19 (“your product” in the conditions below), the relevant Conditions of Authorization are
listed below:
A. Authorized laboratories using your product must include with test result reports, all authorized
Fact Sheets. Under exigent circumstances, other appropriate methods for disseminating these Fact
Sheets may be used, which may include mass media.
B. Authorized laboratories using your product must use your product as outlined in the package insert.
Deviations from the authorized procedures, including the authorized instruments, authorized
extraction methods, authorized clinical specimen types, authorized control materials, authorized
other ancillary reagents and authorized materials required to use your product are not permitted.
C. Authorized laboratories that receive your product must notify the relevant public health authorities
of their intent to run your product prior to initiating testing.
D. Authorized laboratories using your product must have a process in place for reporting test results
to healthcare providers and relevant public health authorities, as appropriate.
E. Authorized laboratories must collect information on the performance of your product and report
to DMD/OHT7-OIR/OPEQ/CDRH (via email: CDRH-EUA-Reporting@fda.hhs.gov
) and you (via
e m a il : ts.scr@abbott.com) any suspected occurrence of false positive or false negative results and
significant deviations from the established performance characteristics of your product of which
they become aware.
F. All operators using your product must be appropriately trained in performing and interpreting the
results of your product, use appropriate personal protective equipment when handling this kit, and
use your product in accordance with the authorized labeling.
G. Abbott, authorized distributor(s), and authorized laboratories using your product must ensure that
any records associated with this EUA are maintained until otherwise notified by FDA. Such records
will be made available to FDA for inspection upon request.
1
The letter of authorization refers to, “laboratories certified under the Clinical Laboratory Improvement
Amendments of 1988 (CLIA), 42 U.S.C. §263a, that meet requirements to perform high, moderate, or waived
complexity tests and use at the Point of Care (POC), i.e., in patient care settings operating under a CLIA Certificate
of Waiver, Certificate of Compliance, or Certificate of Accreditation” as “authorized la boratories.”
PERFORMANCE CHARACTERISTICS

14
Clinical Study:
The performance of ID NOW COVID-19 was evaluated using contrived clinical nasopharyngeal (NP) swab
specimens obtained from individuals with signs and symptoms of respiratory illness. The samples were
prepared by spiking clinical NP swab matrix with purified viral RNA containing target sequences from the
SARS-CoV-2 genome at concentrations approximately 2x LOD and 5x LOD. Negative NP swab samples
were also tested in this study.
The table below presents ID NOW COVID-19 test agreement with the expected results by sample
concentration.
ID NOW COVID-19 Test Agreement with the Expected Results by Sample Concentration
Target
Concentration
Number
Concordant/
Number Tested
% Agreement
[95% CI]
2X LOD
20/20
100% [83.9% - 100%]
5X LOD
10/10
100% [72.3% - 100%]
Negative
30/30
100% [88.7% - 100%]
ANALYTICAL STUDIES:
Analytical Sensitivity (Limit of Detection)
ID NOW COVID-19 limit of detection (LOD) in natural nasopharyngeal swab matrix was determined by
evaluating different concentrations of purified viral RNA containing target sequences from the SARS-CoV-
2 genome.
Presumed negative natural nasopharyngeal swab specimens were eluted in ID NOW COVID-19 elution
buffer. Swab elutes were combined and mixed thoroughly to create a clinical matrix pool to be used as the
diluent. Viral RNA was diluted in this natural nasopharyngeal matrix pool to generate virus dilutions for
testing.
The LOD was determined as the lowest concentration that was detected ≥ 95% of the time (i.e.,
concentration at which at least 19 out of 20 replicates tested positive).
The confirmed LOD in natural nasopharyngeal swab matrix is presented in the table below:
Limit of Detection (LOD) Study Results
Virus
Claimed LOD
(Genome Equivalents/mL)
Positive/Replicates
SARS-CoV-2 RNA
125
19/20
Analytical Reactivity (Inclusivity)
An alignment was performed with the oligonucleotide primer and probe sequences of the ID NOW COVID-
19 assay with all publicly available SARS-CoV-2 genomic sequences submitted to NCBI Genbank, GISAID
and COG-UK databases between June 1 – June 30, 2021 to demonstrate the predicted inclusivity of the ID
NOW COVID-19 assay. A total of 26,855 complete SARS-CoV-2 sequences plus a reference genome were
submitted to NCBI GenBank and 262,260 high quality were submitted to GISAID database. The COG-UK
database contained 97,873 high quality sequences, which came from samples obtained within the same
timeframe. To avoid redundancy only the GISAID copies of any duplicated sequences were retained for
analysis bringing the total number of high quality human SARS-CoV-2 sequences available from all 3
databases to 320,634. Of the total number of sequences analyzed, 399 sequences contained at least 1 N
(unknown or unidentified nucleotide) within the target region, bringing the total number of isolates suitable
for inclusivity analysis down to 320,235. From this analysis 99.32% of the sequences provided 100%
homology to the ID NOW COVID-19 primer and probe sequences.
15
Analytical Specificity (Cross Reactivity)
An in silico analysis for possible cross-reactions with all the organisms listed in the table below was
conducted by mapping primers and probes of the ID NOW COVID-19 target nucleic acid sequence to the
sequences download from the NCBI Genbank and GISAID databases.
The ID NOW COVID-19 assay, designed for the specific detection of SARS-CoV-2, showed no significant
combined homologies with human genome, other coronaviruses, or human microflora that would predict
potential ID NOW COVID-19 false results.
ID NOW COVID-19 Analytical Specificity Microorganisms
Microorganisms from the
Same Genetic Family
High Priority Organisms
Human coronavirus 229E
Human adenovirus A
Human coronavirus OC43 Human adenovirus B
Human coronavirus HKU1
Human adenovirus B1
Human coronavirus NL63 Human adenovirus C
SARS-coronavirus
Human adenovirus D
MERS-coronavirus
Human adenovirus E
Human adenovirus F
Human adenovirus G
Human adenovirus 7
Human adenovirus 8
Human metapneumovirus (hMPV)
Human parainfluenza virus 1 - 4
Influenza A
Influenza B
Enterovirus A-L
Human respiratory syncytial virus
Rhinovirus A - C
Chlamydia pneumoniae
Haemophilus influenzae
Legionella pneumophila
Mycobacterium tuberculosis
Streptococcus pneumoniae
Streptococcus pyogenes
Bordetella pertussis
Mycoplasma pneumoniae
Pneumocystis jiroveci (PJP)
Candida albicans
Pseudomonas aeruginosa
Staphylococcus epidermis
Staphylococcus salivarius
(Rhodotorula mucilaginosa)

16
Microorganisms from the
Same Genetic Family
High Priority Organisms
Streptococcus salivarius
FDA SARS-CoV-2 Reference Panel Testing
The evaluation of sensitivity and MERS-CoV cross-reactivity was performed using reference material (T1),
blinded samples and a standard protocol provided by the FDA. The study included a range finding study
and a confirmatory study for LoD. Blinded sample testing was used to establish specificity and to confirm
the LoD. The results are summarized in the table below.
Summary of LoD Confirmation Result using the FDA SARS-CoV-2 Reference Panel
Reference Materials
Provided by FDA
Specimen
Type
Product LoD
Cross-
Reactivity
SARS-CoV-2
Nasopharyngeal
Swab
3.0x10
5
NDU/mL
N/A
MERS-CoV
N/A
ND
NDU/mL = RNA NAAT detectable units/mL
N/A: Not app li cable
ND: Not detected
SYMBOLS
Fragile, handle with care
Test Base
Transfer Cartridge
Sample Receiver
Prescription Only
Caution, consult accompanying documents

17
ORDERING AND CONTACT INFORMATION
Reorder numbers:
190-000: ID NOW COVID-19 Test Kit
190-080: ID NOW COVID-19 External Control Kit
US + 1 877 441 7440
Technical Support Advice Line
Further information can be obtained by contacting Technical Support on:
US
+ 1 855 731 2288 ts.scr@abbott.com
REFERENCES
1. Manual of Clinical Microbiology, 11th Edition, Vol. 1, ASM. (2015) pg. 279.
Abbott Diagnostics Scarborough, Inc.
10 Southgate Road
Scarborough, Maine 04074 USA
www.abbott.com/poct
© 2020 Abbott. All rights reserved.
All trademarks referenced are trademarks of either the Abbott group of companies or their respective owners.
Software © 2020 Axxin, used under license.
All trademarks referenced are trademarks of their respective owners.
This product is licensed and sold under agreement with Biosearch Technologies, Inc.
This product is sold under license from PHRI Properties and may be used under PHRI Properties patent rights only
for human in vitro diagnostics.
IN190000 Rev. 8 2021/08
